A diagnosis for autoimmune disease happens when the patient’s immune system mistakenly attacks their own body. Our immune system normally protects us from germs, viruses, and borrelia bacteria. When the immune system senses these foreign invaders, it takes an army of cells to attack the threat. Under normal circumstances, our immune system can distinguish dangerous foreign cells from cells produced by our bodies.
What Are Autoimmune Diseases?
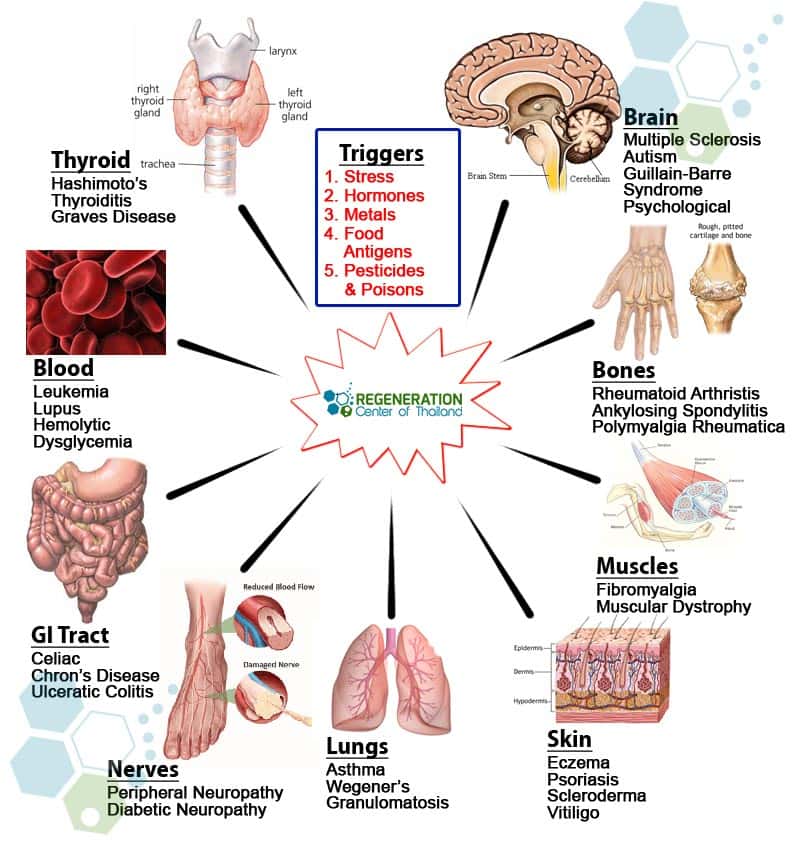
In autoimmune diseases, our immune system mistakes friends from foe and releases auto-antibodies that attack normal healthy cells in the body, like skin cells, organs, or joints. There are over 100 known Autoimmune Diseases, each causing damage to different parts of the body. For example, patients with Type 1 diabetes, get autoimmune damage to the pancreas while other autoimmune diseases, like systemic lupus erythematosus and Fibromyalgia, affect the entire body.[1] Autoimmune brain diseases are diagnosed when the immune system attacks healthy neural cells and tissues in the spinal cord or brain which results in inflammation. The inflammatory response is what causes impaired cognitive and neurological function.
Why does the immune system attack our own body?
Medical researchers don’t know what triggers an immune-system misfire, but some people are more likely to acquire the autoimmune disease than others. A recent study found that women get diagnosed with autoimmune diseases at a rate of 2 to 1 compared to men. For women, Autoimmune disease generally starts during the ages of 15 to 45, which are a woman’s childbearing years. Some autoimmune diseases are also much more common in some ethnic groups. Lupus, as an example, affects more people with African and Hispanic populations than Caucasians. Some cases can be genetic autoimmune disease and run in families. While it doesn’t affect every person in the family, it does increase the risk of acquiring an autoimmune condition. Learn about genetic screenings for autoimmune disease.
Risk factors of Autoimmune Diseases
Over the last 40 years, regenerative medical researchers have also noted a steep rise in autoimmune diseases that may be contributed to exposure to environmental exposure to solvents and chemicals. Other suspected risk factors for developing autoimmune disease & arthritis include food high in fat, artificial sugars, and processed foods. Learn about healthy fats for breakfast and dinner. It is believed that some processed foods lead to systemic inflammation, which can trigger an immune response. Other known factors that can increase the risk of having autoimmune disease include age, genetics, gender, viral & bacterial infections.[2]
The 10 Common Autoimmune Diseases in 2024
The list of autoimmune diseases is quite large with more than 100 known types autoimmune inflammatory disorders but 10 of the most common ones include:
1. Type 1 diabetes (TD1) was previously known as juvenile diabetes or insulin-dependent diabetes is a chronic autoimmune disease where our pancreas produces very little or no insulin. Our pancreas is responsible for producing the hormone insulin, which regulates our blood sugar levels. Their immune system attacks insulin-producing cells for patients with type 1 diabetes, which slowly destroys pancreatic function. Over time, higher blood sugar levels damage blood vessels and surrounding organs like the kidneys, eyes, peripheral nerves and can lead to heart failure.
2. Rheumatoid Arthritis (RA) is an common systemic autoimmune rheumatic disease and chronic inflammatory disorder that affects various joints in the body but can affect other areas. A diagnosis of rheumatoid arthritis can lead to low red blood cell counts, inflammation around the heart and lungs. RA typically results in painful swollen joints in the wrists and hands. Patients with RA often report pain and stiffness following periods of rest. Unlike osteoarthritis (OA), which commonly affects older adults as they get older, autoimmune rheumatoid arthritis can start in the early 30s or sometimes sooner.
3. Multiple sclerosis (MS) is an autoimmune disease that attacks and damages the myelin sheath (central nervous system) and spinal cord. The myelin sheath is the protective coating surrounding nerve cells and motor neurons. Myelin is primarily made up of fatty substances and proteins. The myelin sheath helps electrical impulses and neurotransmitters send and receive paracrine signals quickly and efficiently along in the central nervous system. Damage to myelin sheath results in slowing down the speed of messages between the brain and spinal cord. Over time, the damage leads to other symptoms like neuropathy, visual disturbances, numbness, prickling (pins and needles), balance issues, weakness, thinking, memory problems, and trouble walking. There are several types of neurological autoimmune diseases including Multiple sclerosis which can progress at different speeds. Statistics show that multiple sclerosis t cell reductions affects women more often than men an usually begins between the ages of 18 and 40.
4. The systemic lupus erythematosus (SLE) is another common autoimmune disease. In SLE, the immune system mistakenly attacks healthy tissue throughout the body. In the 19th century, lupus was thought of as a skin disease because of a typical rash that it produces and tnf induced psoriasis. The most common type of lupus is a systemic version that typically affects organs like the kidneys, brain, and heart but can also result in severe joint pain, chronic fatigue, cardiovascular issues and body rashes. The underlying causes of lupus erythematosus are still unknown but doctors believe it may be due to heredity causes, bacterial or viral infections, reaction to medications, or prolonged exposure to ultraviolet light. Lupus can affect patients of all ages (including children). However, it is most often diagnosed in women during childbearing years. Women are affected by lupus far more than men. Learn about stem cell therapy for lupus.
5. Inflammatory bowel disease (IBD) is an autoimmune disease that causes chronic inflammation in the intestinal wall’s linings. There are two primary types of IBD, including Crohn’s disease and Ulcerative colitis. The symptoms of IBD are characterized by inflammation in the gastrointestinal (GI) tract, but the GI tract area depends on the type of IBD the patient is diagnosed with. Patients with Crohn’s disease can get inflammation in any part of the gastrointestinal tract, from the inside of the mouth down to the anus. On the other hand, ulcerative colitis primarily affects the linings of the rectum and large intestine (colon).[3] Common symptoms of IBD can include:
- Bloody Diarrhea
- Iron deficiency (anemia) due to blood loss
- malabsorption due to processing of common elements in the human body
- Abdominal pain & cramps
- Aphasia as a Symptom of Autoimmune Encephalitis
- Fever
- Frequent bowel movements
- Loss of appetite
- Weight loss
6. Hashimoto’s thyroiditis (HT) – also known as chronic lymphocytic thyroiditis is an autoimmune condition where the immune system attacks and damages the patients’ thyroid glands, causing it to produce less thyroid hormone an underactive thyroid. HT can be a life-threatening disease that develops after long-term hypothyroidism, often due to untreated Hashimoto’s disease. Signs and symptoms of HT include:
- Drowsiness
- Lethargy and Chronic fatigue
- Muscle aches
- Hair loss
- Constipation
- Facial swelling
- Weight gain
- Stiff and painful joints
- Sensitivity to cold
Causes for Hashimoto’s disease generally include genetic and environmental factors, and the disease affects women more often than men.
7. IgA nephropathy and Glomerulonephritis are autoimmune related to kidney diseases. IgA nephropathy is diagnosed when the IgA protein (albumin) usually helps our body fight infections settles into the kidneys instead of passing. Over time, IgA deposits cause the kidneys to start leaking blood and protein in the urine (proteinuria). When too much protein leaks into our urine, a person’s hands and feet begin to swell. IgA nephropathy is a chronic condition, and over time about 30 percent of patients develop renal failure. IgA nephropathy can happen at any age, but less than 10 percent of children’s cases result in total kidney failure. Chronic kidney failure symptoms include edema (swelling) in the feet & hands, fatigue, headaches, nausea, and sleep disorders. Patients with end-stage kidney failure need hemodialysis and are often placed on a kidney transplant waiting list, for autoimmune IgA nephropathy men are more often diagnosed than women. Besides diabetic nephropathy, PKD and hypertension (high blood pressure), IgA nephropathy is one of the most common kidney diseases.
Glomerulonephritis is another type of autoimmune kidney disease that attacks the waste filtration function of the kidneys. Glomerulonephritis is diagnosed when damage to the glomerulus causes protein and blood to be lost in the urine. The disease often develops quickly, and kidney function can be lost within weeks (rapidly progressive Glomerulonephritis). About 25% of patients diagnosed with chronic Glomerulonephritis have no family history of kidney disease.
The causes for patients are often unknown, but some of the following reasons might increase the risk of acquiring the condition:
- Amyloidosis
- Abscesses
- IgA nephropathy
- Goodpasture syndrome
- Exposure to environmental toxins or hydrocarbon solvents
- Reaction to prescription medications
- Heavy use/misuse of pain relievers including NSAIDs
- Blood or lymphatic system disorders
- Previous history of cancer
- Viruses or bacterial infections
- Heart infections, previous heart attacks or heart disease
- Membranoproliferative GN
- Anti-glomerular basement membrane antibody disease
- Henoch-schonlein purpura
- Lupus nephritis
Common symptoms include dark brown or rust-colored urine, foamy urine, and/or swelling in the face, ankles, eyes, feet, abdomen, or legs.
8. Ankylosing spondylitis (AS) also known as Bechterews disease or spinal arthritis, is an autoimmune disease of the spine. AS causes swelling inside the spinal vertebrae and in the joints between the pelvis and spine. Ankylosing spondylitis is more often diagnosed in men and can often be HLA-B27 variation in persons DNA. Symptoms of Ankylosing spondylitis include severe back pain and chronic stiffness. These symptoms of AS often in early adulthood, and if left untreated, ankylosing spondylitis fuses the spinal vertebrae, thus limiting movement. Ankylosing spondylitis is an autoimmune disease that attacks muscles and also result in pain, inflammation, and stiffness in other joints such as hips, shoulders, ribs, hands, knees and feet. Although rare, AS can sometimes affect the eyes (iritis & uveitis), lungs, and heart function.
9. Axonal & neuronal neuropathy (AMAN) sometimes referred to as Guillain-Barré syndrome, is an autoimmune disease characterized by paralysis and loss of reflexes but without sensory loss. AMAN syndrome appears as a progressive symmetric paralysis resulting in loss of muscle function and absence of normal neurologic reflexes (knee jerk reactions). Axonal & neuronal neuropathy happens when antibodies attack the outer coatings of motor neurons but without causing inflammation. The attacks do not affect sensory neurons, so the patients’ sensations remain but without movement. AMAN is part of multiple autoimmune syndrome (MAS) so patients with axonal & neuronal neuropathy are found in patients diagnosed with chronic obstructive pulmonary disease (COPD) and cases with respiratory failure. A similar type of neuropathic autoimmune disease is chronic inflammatory demyelinating polyneuropathy (CIDP). This rare disorder occurs when the immune system attacks the nerve roots and destroys the myelin sheath resulting in paralysis and/or impairment in the patient’s arm and leg motor function. Patients with CIDP also report a sensory loss, numbness, burning sensations, and tingling. Chronic inflammatory demyelinating polyneuropathy can affect any age group and can begin anytime in life.
10. Fibromyalgia (FMS) is a chronic disease that is characterized by widespread body pain, tenderness, and chronic fatigue. Although Fibromyalgia is not considered a classical autoimmune disease, it accompanies other similar autoimmune rheumatic and endocrine diseases. Patients with Fibromyalgia often experience morning stiffness, sleep disturbances, anxiety, depression, and irritable bowel syndrome. Often it is also accompanied by. FMS can be very difficult to diagnose because many of the symptoms are similar to other disorders. To learn more about how to deal with autoimmune fatigue visit here.
Although there are many types of autoimmune diseases, the symptoms often overlap making them very difficult to diagnose. Disease can manifests itself as mild but distressing symptoms affecting the person’s quality of life for some patients. Still, for others, it can be severe sometimes fatal due to severe tissue damage.
Stem Cell Therapy for Autoimmune disease
In many cases, traditional management strategies include taking medication, changing a person’s diet, and making other lifestyle changes to reduce the symptoms. Autoimmune conditions are most often treated with immune suppressive agents that can provide temporary improvement but carry many long-term adverse effects and require perpetual life-long treatments. Learn about how some foods can increase your circulating stem cells
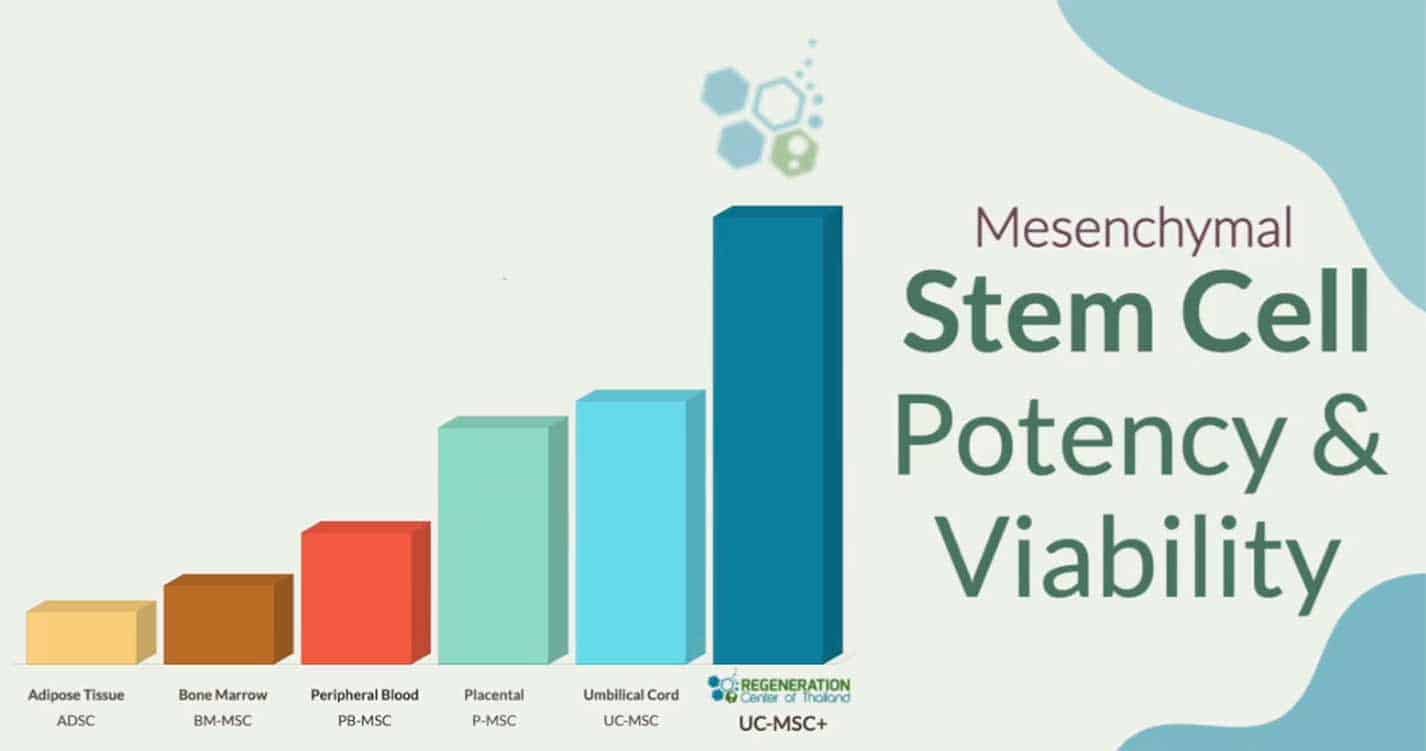
Recent breakthroughs in functional healthcare have shown that enhanced Mesenchymal Stem cells (MSC+), progenitor and SVF cells can be used effectively to promote healing on the cellular level for many common (non-genetic) types of autoimmune diseases such as Sjogren’s Syndrome.[4] For genetic conditions several clinical trials are being done currently to use gene therapies to cure hereditary autoimmune diseases. Learn more about the Regen Center DNA test for Autoimmune disorders such as Myasthenia gravis. Besides the ability to heal damaged tissues, autoimmune disease treatment using stem cells can help modulate the immune system (immunomodulatory properties)[5] to turn off the unwanted pathological responses while preserving the immune systems ability to fight off disease. Isolated and expanded Mesenchymal stem cells and tissue-specific growth factors can be used to target specific areas with inflamed tissue and help the body restart the production of anti-inflammatory agents, macrophages, T cells, neutrophils, and monocytes. These cellular mediators do not suppress the patents immune response while increasing production of B cells, NK cells, dendritic cells, progenitor cells, and T regulatory cells, which is a type of immune cell that protects our body from immunological self-attacks and normalize cell apoptosis, promote angiogenesis and neurogenesis. Learn about stem cells for ibm disease
MSCs+ stem cell transplants are not effective or appropriate for all causes but can be recommended for autoimmune diseases as they provide immunosuppressive and immunomodulatory effects. Stem cell therapy can help renew the lymphatic system, restart a defective immune system, reduce disease activity, and lead to long-term remissions. Stem cells can also be beneficial for patients who are resistant to conventional treatments, failed surgeries, or those who have become sensitive to conventional therapies thanks to the immunomodulatory properties of enhanced mesenchymal (MSCs+) Stem cells.
Published Clinical Citations
[1] ^ F H Abouali, D S Sheha, H M Elsayed, N A Ibrahim, S T Kamal, Y S Sharawy, IgA Deficiency in type 1 Diabetes Mellitus patients, QJM: An International Journal of Medicine, Volume 113, Issue Supplement_1, March 2020, hcaa052.055, https://doi.org/10.1093/qjmed/hcaa052.055
[2] ^ Y.W. Song, E.H. Kang, Autoantibodies in rheumatoid arthritis: rheumatoid factors and anticitrullinated protein antibodies, QJM: An International Journal of Medicine, Volume 103, Issue 3, March 2010, Pages 139–146, https://doi.org/10.1093/qjmed/hcp165
[3] ^ J. A. SNOOK, H. J. de SILVA, D. P. JEWELL, The Association of Autoimmune Disorders with Inflammatory Bowel Disease, QJM: An International Journal of Medicine, Volume 72, Issue 3, September 1989, Pages 835–840, https://doi.org/10.1093/oxfordjournals.qjmed.a068372
[4] ^ J.J. El-Jawhari, Y.M. El-Sherbiny, E.A. Jones, D. McGonagle, Mesenchymal stem cells, autoimmunity and rheumatoid arthritis, QJM: An International Journal of Medicine, Volume 107, Issue 7, July 2014, Pages 505–514, https://doi.org/10.1093/qjmed/hcu033
[5] ^ Bulati Matteo, Miceli Vitale, Gallo Alessia EC. The Immunomodulatory Properties of the Human Amnion-Derived Mesenchymal Stromal/Stem Cells Are Induced by INF-γ Produced by Activated Lymphomonocytes and Are Mediated by Cell-To-Cell Contact and Soluble Factors DOI=10.3389/fimmu.2020.00054 https://www.frontiersin.org/article/10.3389/fimmu.2020.00054