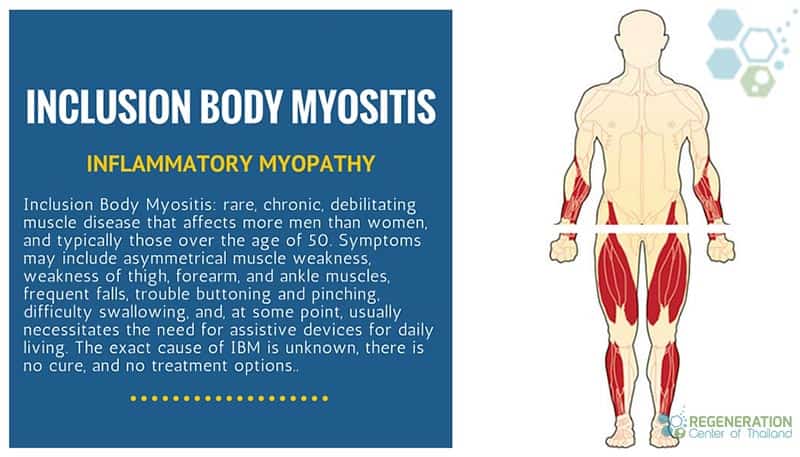
Inclusion Body Myositis (IBM) is a very rare and progressive muscle disorder & autoimmune myopathy affecting men and women, usually over 45 years old. This condition involves the gradual weakening and wasting of muscles in the legs and arms, leading to difficulty performing everyday tasks like walking, lifting, and gripping. IBM can be both sporadic or familial (genetic causes) [1].
Genetic inclusion-body myopathy can be inherited in either a recessive or dominant pattern. Dominant IBM genetic disorders require only one genetic flaw to show themselves. Recessive IBM disorders however require that both parents pass on a flaw in the same gene before their offspring can show signs of the disease. Unfortunately there is no cure for Genetic IBM but researchers hope gene therapies will eventually be able to cure the disease. For patients with Sporadic inclusion body myositis (sIBM) Currently early diagnosis and proper management are the best options for patients and can help slow down the progression of the disease and improve the quality of life for those affected [2].
Recognizing the symptoms of IBM can be challenging, as they typically develop slowly over time and can mimic other muscle disorders. Some common signs of IBM include:
- Weakness in the hands and fingers,
- Difficulty swallowing
- Muscle pain
- Stiffness
- Peripheral neuropathy and loss of sensation in the limbs.
Understanding Inclusion Body Myositis (IBM)
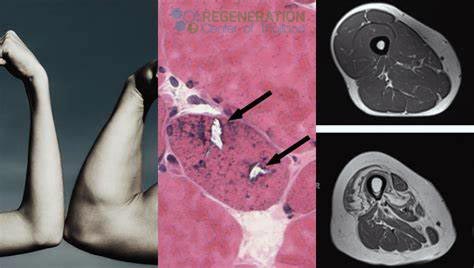
Inclusion Body Myositis (IBM) can affects the body in multiple ways. Myositis is a general term referring to inflammation of the muscles. In muscle cells, abnormal entities known as inclusion bodies may be observed during muscle biopsies of patients suffering from IBM. The existence of these inclusion bodies distinguishes this form of myositis from comparable conditions, like multiple sclerosis, Broca’s Aphasia, polymyositis and dermatomyositis.
Recognizing IBM Symptoms
For many patients the exact cause of IBM is often unknown and classified as Idiopathic, Doctors believe IBM is related to an abnormal immune response that attacks and damages 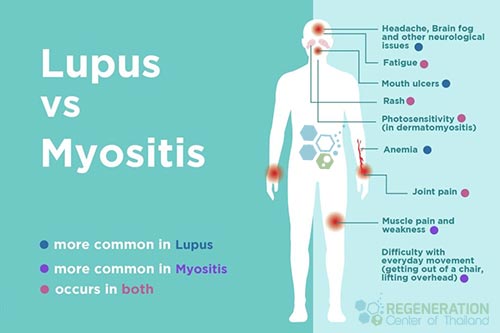 muscle tissues. Spotting the telltale signs of IBM can also be difficult, but there are specific indicators that can help with diagnosis. One of the earliest symptoms is muscle weakness in the quadriceps, which can cause difficulty in standing up from the seated position or when climbing stairs. Over time, weakness in other muscles, such as the finger flexors, wrist extensors, and ankle dorsiflexion, may also develop. In addition, IBM can cause muscle wasting, particularly in the forearms and quadriceps, and difficulty swallowing or speaking due to weakness in the throat muscles[3].
muscle tissues. Spotting the telltale signs of IBM can also be difficult, but there are specific indicators that can help with diagnosis. One of the earliest symptoms is muscle weakness in the quadriceps, which can cause difficulty in standing up from the seated position or when climbing stairs. Over time, weakness in other muscles, such as the finger flexors, wrist extensors, and ankle dorsiflexion, may also develop. In addition, IBM can cause muscle wasting, particularly in the forearms and quadriceps, and difficulty swallowing or speaking due to weakness in the throat muscles[3].
Other common symptoms of IBM include muscle pain, stiffness, and fatigue. These symptoms can be exacerbated by exercise and may be more noticeable after periods of inactivity. Some people with IBM also experience a loss of sensation or numbness in their fingers or toes. It is important to note that while these symptoms may point to IBM, they are not definitive, and a proper diagnosis requires a combination of clinical examination, blood tests, and muscle biopsy.
Investigating the causes of IBM
Patients can better understand IBM by exploring the various factors that can contribute to its pathogenesis. IBM is believed to be an autoimmune disorder, meaning the patients own immune system mistakenly attacks its cells and tissues. Aside from autoimmune factors, age, and genetics may also play a role in the development of IBM. IBM typically affects people over 45 years old, and it is more common in men than women. Additionally, some studies have found that specific genetic mutations may increase a person’s risk of developing IBM. However, more research is needed to determine the genetic factors that contribute to the development of this condition. Understanding the causes of IBM is crucial in developing effective treatments and prevention strategies for this debilitating condition.
Diagnosing IBM Disorder
To accurately diagnose IBM, your doctor may recommend a series of blood tests, biopsies and radiological evaluations to assess a patients muscle strength, range of motion, and overall physical abilities. One standard test used to diagnose IBM is a muscle or tissue biopsy, in which a tiny sample of muscle tissue is surgically removed and examined under a microscope. This can help determine if there are any abnormal protein deposits, or inclusion bodies, in the muscle tissue, which is a hallmark of IBM.
Other tests that may be used to diagnose IBM include electromyography (EMG), which measures the electrical activity in your muscles, and magnetic resonance imaging (MRI), which can help identify any muscle inflammation or damage. Blood tests may also rule out other conditions that can cause muscle weakness, such as thyroid disorders or other autoimmune diseases such as ankylosing spondylitis, lupus, rheumatoid arthritis, connective tissue disease, type 1 diabetes, sjogrens or hashimotos disease, Using a combination of these tests and evaluations, a primary care doctor can make an accurate diagnosis and develop an effective treatment strategy to manage the negative symptoms and improve patient quality of life.
Traditional Treatment options for IBM
Once diagnosed with IBM, managing the condition with various treatment options can significantly improve your quality of life. Although there is no cure for genetic IBM, there are ways to slow down the rate of progression of the disease and alleviate symptoms. Currently some of the most effective strategies use a combination of isolated mesenchymal stem cells, physical therapy, and lifestyle changes can be effective in managing IBM.
So far, clinical trials have not shown many clear benefits for any specific drug treatments of inclusion body myositis. For that reason many experts do not prescribe medications for inclusion body myositis except in some certain limited situations. Traditional medication options for IBM include:
- Immunosuppressive medications (help reduce inflammation and slow down muscle damage)
- Corticosteroids
- Physical therapy and rehab can also help improve muscle strength and mobility and prevent muscle atrophy.
- Lifestyle changes such as a healthy diet and regular exercise can also help manage symptoms and improve symptoms related to IBM and autoimmune myopathies
Other Biological treatments include:
- TNF inhibitors
- Abatacept offers selective co-stimulation inhibitor that inhibits binding of CD28 expressed on effector T cells reducing T-cell activations
- Tocilizumab
- Alemtuzumab
- Anakinra
- MEDI-545 (anti-IFNα antibody)
TREATMENT PRECAUTIONS & RISKS
Please note patients with multiple comorbidities or immune system dysregulation may cause travel limitations to Thailand. All potential candidates seeking therapy should be approved in advance using basic medical records and recent blood panels that can include tissue biopsy results along with known markers of inflammation such as C-reactive protein, Erythrocyte sedimentation rate (ESR). Depending on the stage and severity of the diagnosis additional tests for antibodies (autoimmune conditions) and imaging tests from MRI or CT Scan maybe required. Please contact us for more information.Stem Cell Treatment for Inclusion Body Myositis
Inclusion Body Myositis involves both inflammatory and degenerative characteristics making it an ideal candiate for cellular therapy. Clinical trials for IBM have shown that satellite cells (SC) proliferation is normal for patietns with IBM patients and ususally their overall cell differentiation ability is impaired thus leading to muscle failure. In extremely resistant myositis cases, a combination treatment using myeloablative conditioning with cyclophosphamide. After treatment with cyclophosphamide and total body irradiation, followed by reinfusion of cord tissue stem cells and granulocyte colony stimulating factors help improved muscle strength, with no trace of myositis seen on a MRI 6 months after treatment. This outcome remained stable for over 3 years. Other patients with progressive IBM demonstrated significant improvements and sustained remission after modified stem cell treatment without the need for adding the toxic treatment requiremetns for patients with severe, resistant diagnosis.
Can stem cells cure myositis?
 Mesenchymal stem cells and the process of immunomodulation can help to suppress various immune cells’ activities and have minimal immunogenicity risk. The Regeneration Center offer both autologous and allogeneic mesenchymal stem-cell transplantation for patients with non-genetic sporadic cases of IBM.
Mesenchymal stem cells and the process of immunomodulation can help to suppress various immune cells’ activities and have minimal immunogenicity risk. The Regeneration Center offer both autologous and allogeneic mesenchymal stem-cell transplantation for patients with non-genetic sporadic cases of IBM.
The ability of stem cells to renew themselves throughout our lives is provent to be beneficial for many body tissues. However, it’s believed that skeletal muscles, which make up our body structure, only renew a few times under very specific conditions. As we age the body handles increased demands by growing bigger (hypertrophy), not by making more cells (hyperplasia). This could be a reason why muscle stem cells can’t renew themselves as much as other types of stem cells, like those in peripheral blood[4].
Using isolated MSC cells with cultured muscle stem cells and growth factors offers patients a targeted way to treat muscle diseases over a period of 2-3 weeks using multiple cycles to initiate the repair process. When muscle stem cells get used up, and the muscle is gradually replaced by fat and connective tissue. In some cases The Regeneration Center also uses fibro-adipogenic progenitors cells due to the vital role they play in muscle repair. The isolated progenitor cells and growth factros help activate satellite cells even though they end up producing fat and scar tissue. Dealing with scar tissue (fibrosis) is also a key part of any treatment strategy. From our research, we’ve learned that treatments need to start as early as possible, or they’re unlikely to be effective particularly in cases with significant fibrosis[5].
The Regeneration Center Difference
Total Number of MSC+ Cell Infusions: Total Endogenous Cell Count and range of growth factors will vary based on patient needs. Multi-stage delivery of cells can be done via a guided radiograph (when necessary) through an intravenous drip, direct injection, or Intrathecally.
Rehabilitation Post Treatment: Physical Rehabilitation in Bangkok is optional but highly recommended. Complete physical rehab services post-therapy can be provided upon request for 2-3 hours per day and up to 5 days per week.
Total Treatment Time Required: estimated around 2 weeks (depending on type and seriousness of condition). Medical and travel visas for extended stay accommodations at a hotel or extended stay apartment for the patient and family can also be provided upon request.
New IBM Disease Treatment Guidelines 2024
The cost for inclusion body myositis treatment will vary depending on degrees of severity. Our medical team will need to evaluate the patients using current medical records. Evaluations can be done in person or online (submitting documents online). After review, a detailed treatment plan will be provided that will include the specifics such as the exact total number of nights required and total medical costs for treatment connective tissue disease with stem cells. To begin the evaluation process, please prepare all current medical records and contact us today.
Published Clinical Citations
[1] ^Naddaf E, Barohn RJ, Dimachkie MM. Inclusion Body Myositis: Update on Pathogenesis and Treatment. Neurotherapeutics. 2018 Oct;15(4):995-1005. doi: 10.1007/s13311-018-0658-8. PMID: 30136253; PMCID: PMC6277289.
[2] ^ Sanmaneechai O, Swenson A, Gerke AK, Moore SA, Shy ME. Inclusion body myositis and sarcoid myopathy: coincidental occurrence or associated diseases. Neuromuscul Disord. 2015 Apr;25(4):297-300. doi: 10.1016/j.nmd.2014.12.005. Epub 2014 Dec 19. PMID: 25599912.
[3] ^ Schmidt K, Schmidt J. Inclusion body myositis: advancements in diagnosis, pathomechanisms, and treatment. Curr Opin Rheumatol. 2017 Nov;29(6):632-638. doi: 10.1097/BOR.0000000000000436. PMID: 28832349.
[4] ^ Lloyd TE. Novel therapeutic approaches for inclusion body myositis. Curr Opin Rheumatol. 2010 Nov;22(6):658-64. doi: 10.1097/BOR.0b013e32833f0f4a. PMID: 20827206; PMCID: PMC4365473.
[5] ^ Tedesco FS, Dellavalle A, Diaz-Manera J, Messina G, Cossu G. Repairing skeletal muscle: regenerative potential of skeletal muscle stem cells. J Clin Invest. 2010 Jan;120(1):11-9. doi: 10.1172/JCI40373. PMID: 20051632; PMCID: PMC2798695.


