For most patients suffering from blunt force trauma to the knee, debilitating knee damage, or osteoarthritis, traditional options to repair knee issues are limited. Currently, most conventional approaches look to mask the pain with cortisone steroid injections, risky joint replacement surgery, or simple physical therapy that does not target the root issue. The Regeneration Center offers a powerful non-surgical alternative to knee replacements using a combination of enhanced stem cells and exosome growth factors. Our unique protocol uses proprietary cell growth factors in the Ortho+ Knee Regeneration protocol to achieve better results via multiple endogenous UC-MSC+ cell infusions and tissue-specific growth factors. Stem cell therapy is ideal for degenerative hip and damaged kneecap-induced pain, for those looking for an effective alternative to knee replacement surgery, or for those with joint ligament, tendon, and bone injuries from playing sports. Get back to doing everything you love to do in life faster & without invasive surgeries.
Stem Cell Therapy For Knees
Meniscus Tears, Ligament & Tendon Tears
The human body consists of billions of very specialized cells that differentiate into specific purposed organs such as skin, muscle, brain, heart, ligaments, tendons, bones, and connective joints. These specialized cells continually circulate through the body as part of our natural regenerative process. Typically, when older cells die ( apoptosis ), new cells are created from our circulating adult stem cells that can create multiple cell lineages.[1] When cartilage or tissue in the human body is injured, the degenerative effects can exceed the capacity of our natural regenerative process, resulting in joint structures becoming weaker, less functional, and painful due to cartilage loss. This is especially true for middle-aged and older patients who get injuries in areas like the knees that are isolated from continuous blood circulation ( vehicle for regenerative medicine ).
There are hundreds of different types of stem cells in our body; however, only a few cell types are beneficial for musculoskeletal applications such as spinal stenosis, hip injuries, and shoulder repairs. Mesenchymal stem cell markers (UC-MSC+) offer the highest potential for articular cartilage regeneration. MSC cells used in therapies are isolated from a select group of cell-rich tissues and expanded to enhance their differentiation potential.[2]
Cellular Lines Used In Knee Regeneration Therapies
- The positive cell markers used in the isolation and expansion include STRO-1, CD146, CD73, CD166, CD105, and CD106.
- The negative MSC cell markers include CD45, CD11b, CD31, CD34, and CD117.
The bioactive factors secreted by enhanced UC-MSC+ stem cells can help inhibit tissue scarring, suppress the apoptosis phase, stimulate angiogenesis, and improve mitosis of the MSC+ progenitor cells. The Enhanced UC-MSC+ cell protocol and regenerative knee therapy we offer provide patients with the many practical advantages of engineered cartilage cells that can repair osteochondral lesions, inflammation, stiffness, and chondral lesions. Regenerative medicine for hand arthritis,shoulder arthritis, hip and knee arthritis can also initiate endogenous regenerative capacity and offer a meniscus surgery alternative via umbilical cord stem cell therapy for knee pain.
Effective Knee Regeneration Protocols

Targeting Medial Collateral Ligament (MCL) Injury
The Regen Center Orthopedic Stem Cells for knee problems offers a non-surgical treatment of knee osteoarthritis for injuries and regenerative therapy for conditions including:
- ACL (Anterior Cruciate Ligament) Non-Retracted sprain or tear – ACL injection therapy
- MCL (Medial Cruciate Ligament) sprain or tear
- PCL (Posterior Cruciate Ligament) sprain or tear
- Rheumatoid arthritis of the Knees
- Knee Tendonitis or Tendinopathy with pain and swelling
- Patellar Tendinosis or Tendonitis
- Bone on bone Osteoarthritis
- Runner’s Knee aka Chondromalacia
- Pes anserine Bursitis to repair damaged knees
- Patello femoral syndrome ( PFS )
- Iliotibial band syndrome ( ITBS )
- Osgood-Schlatter Disease ( OSD )
- Synovial plica syndrome & Medial plica syndrome
- Stem cell for torn meniscus & knee meniscus Injuries and tears
- Bursitis of the Knees
- Baker’s cysts
- Inflammatory arthritis ankylosing spondylitis
- Enthesopathy
Degenerative Osteoarthritis of the Knees
The Regen Center ACL protocol is a combination therapy using enhanced cells and osteogenic growth factors for autoimmune knee arthritis.UC-MSC+ cells are also used to heal partially torn Anterior cruciate ligaments and complete non-retracted ACL tears. Our safe, non-surgical alternative to ACL repair is a viable option for those considering surgical intervention because of a partial ACL tear or complete non-retracted tear.
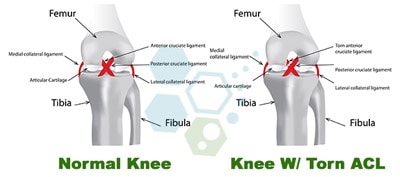
UC-MSC+ stem cell injections for knees can help you avoid extended downtime and the painful rehabilitation process that traditionally follows after anterior cruciate ligament surgery. For severe or complex injuries, our orthopedic team will need to target the injured zones using sophisticated image guidance to ensure optimal delivery of the cells for a successful minimally invasive procedure.
Stem Cells for Treating Meniscus Tears
Stem Cell therapy for meniscus tears is the most common type of knee injury we treat. Surgically repairing a meniscus tear should be considered the last option. Meniscus tear repairs work by surgically removing some (partial meniscectomy) or all of a critical structure in the knee. A minimally invasive combination of adult stem cells, PRP, and post-therapy physical rehabilitation is usually a safer and better option.[3]
Knee Replacement Alternatives
The meniscus is a crescent-shaped fibrocartilaginous structure that acts as a spacer between the femur and tibia while providing shock absorption capabilities for the knee joint. It can be an effective shock absorber by equally distributing blunt forces across the knee joints. A meniscus comprises living fibrocartilage tissue, and each knee has two menisci.
- A medial meniscus (closer to the inside)
- A lateral meniscus (closer to the outside)
For various biomechanical reasons, most injuries occur on the medial meniscus.
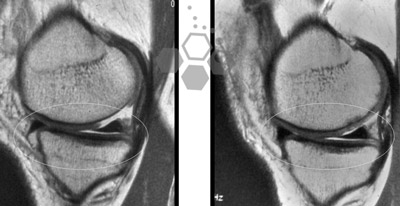
Knee Meniscus Tears & Cartilage Loss
The medial meniscus is usually the most injured part of a knee. Most acute traumatic meniscus tears we treat happen due to sudden and traumatic twisting of the knees. For some elderly patients, traumatic injuries and meniscus tears are caused by the gradual weakening of the meniscus as a result of degenerative or arthritic joints. Meniscus tears are usually described by the position/location of the damage (posterior or anterior) and which one of the two injured menisci (lateral or medial). Some examples of meniscus tears include:
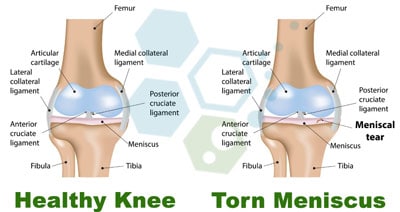
Meniscus Flap Tears or unstable meniscus tears: This type of meniscus injuries/flap tears occur in the inner rim and usually involve a small part of the meniscus. This type of damage cannot heal without intervention since the area in the knee does not have an adequate blood supply. Most traditional orthopedic surgeons like to “trim” or “shave” (remove) the meniscus, which leads to other long-term knee issues. Use caution if considering surgical intervention, as stem cells are a better alternative to repair the tear and stabilize the full range of motion.
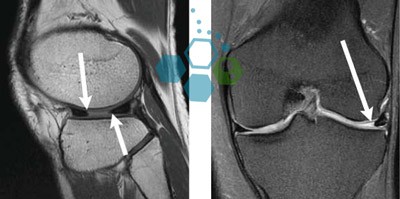
Bucket-Handle Meniscus Tear: Bucket-handle meniscus tears are usually more painful than other tears. When the inner rim of the medial meniscus is torn, it is called a “bucket-handle tear” because it looks like a handled bucket. These types of tears usually occur in an area with a good blood supply, and if caught early, they can be sutured back into place. Alternatively, enhanced stem cell infusions + paracrine signaling can accomplish the same repair without any risk and downtime associated with surgery.
Stem Cells for Treating Bucket Handle Tears
A medial meniscus Tear: The Medial menisci can be found in the inner side of our knee joints. The torn medial meniscus diagnosis usually describes the severity of a tear on the medial meniscus that is often caused by traumatic injury or sudden change of force or direction that occurs in sports such as skiing, basketball, football, soccer, and volleyball. This type of injury can also occur as a result of repetitive use injuries like long-distance running, track and field, and cycling, along with long-term degenerative knees in older patients. Stem cell therapies can treat medial meniscus tears and cartilage damage efficiently and without surgical intervention.[4]
Cartilage Regeneration Naturally?
Complex Degenerative Meniscus Tears: Degenerative meniscus tears are most commonly found in middle-aged or elderly patients due to decades of repetitive stresses that have severely weakened the meniscal tissue. Unlike acute traumatic tears, Degenerative meniscus tears are not sudden and are more symptomatic. Common symptoms of degenerative meniscus tears include:
- Pain along the joint line
- Catching and locking
- Swelling
Degenerative meniscal tears in the knees are sometimes associated with Lupus, osteoarthritis, osteoporosis, and degenerative joint diseases. These types of tears are commonly associated with osteoarthritis of the knees and cause the menisci to tear or fray in multiple directions. With that many tears, most surgeons do not try to repair surgically since it likely will cause more harm than good. If traumatic meniscus tears are left untreated, they can often lead to peripheral neuropathy and arthritis. The Regen Center offers a unique stem cell protocol for degenerative knee injuries to support cartilage regeneration with isolated stem cells and tissue-specific growth factors to heal the area and alleviate pain using our body’s natural repair mechanisms.
Recently published clinical trials have shown that meniscus removal surgeries are no more effective than not having surgery or just having physical therapy. Surgical meniscus removal creates much higher impact forces inside the knees, and it’s estimated that removing as little as 10% of the knee meniscus tissue can increase overall knee joint stress by about 65%. When more than half (50%) of the menisci is surgically removed through surgery, the stress levels increase exponentially, leading to more failure and more knee surgeries and ultimately left with the treatment option of a total knee replacement surgery, which generally lasts only 15-20 years before needing to be replaced yet again with another surgery.

Cell Regeneration for Knee Pain after Cartilage Loss
The Regeneration Center protocol for regenerating cartilage and restoring joint function will require proper isolation, expansion, and multi-stage delivery of stem cells to the damaged joint. It can take 10-14 days in total. Our cellular therapy does not require additional surgery or overnight hospital stays, and patients can return to normal activities following the procedure. A non-surgical approach to decreasing pain and developing new cartilage is also beneficial by avoiding the risk of lengthy and painful rehabilitation needed after invasive knee joint surgeries.
Benefits of Stem Cell Therapy for Knees
Cartilage stem cell injections and knee therapy can help promote naturally anti-inflammatory agents (for healthy cartilage), such as cytokines, and contain essential growth factors, which help stimulate tissue growth. Proper rehabilitation and anti-inflammatory foods are also recommended to eliminate pain medications to help restore the strength, range of motion, and mobility of the knee joints to pre-injury levels.[5]

How Stem Cell Infusions Can Help Repair a Torn Meniscus
Hematopoietic Mesenchymal Stem Cell Therapies have been used for over 45 years now and are a very safe, effective alternative therapy. Our medical team has already performed several thousand injections, and we have never had a single case report adverse side effects.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating knee pain,knee cartilage injury or knee arthritis with stem cells. Patients with severe osteoarthritis, extensive cartilage loss, significant joint deformities, or other underlying health conditions may not qualify for the recommended treatment protocol.Stem Cells for Knee Osteoarthritis & Knee Joint Repair
Locations for Stem cell knee injections: The total number of cells and infusion points depends on the severity of the knee problem and the age/severity of the injury.
Type of Cells Used and Injection Locations: The knee regeneration protocol requires Isolated and Expanded Mesenchymal cells (UC-MSC+) from the patient (Autologous). For multiple injuries or severe degeneration, we will recommend umbilical cord tissue-derived UC-MSC+ cells along with osteogenic and cartilage growth factors. The Regeneration Center therapy for knee joints does not require surgery and depends on the area of injury. The stem cells used in treatments are delivered through localized infusions, ultrasound-guided, fluoroscopy, or CT-guided, targeting the areas surrounding the damaged knee cartilage.
Rehabilitation Options Post Therapy: Physical Rehabilitation therapy after cells is highly recommended in Bangkok or upon return to your home. We have complete physical rehab packages available in Bangkok, Phuket, or Chiang Mai, depending on your travel/time constraints. Our rehabilitation program is available upon request for 2-3 hours per day and up to 5 days per week. Thai Medical visas or hotel accommodations for the patient and family can also be provided upon request.
Total Treatment Length needed to repair damaged cartilage: Estimated time for stem cell knee injuries is 10-14 days in Bangkok (depending on the severity of the underlying injury)
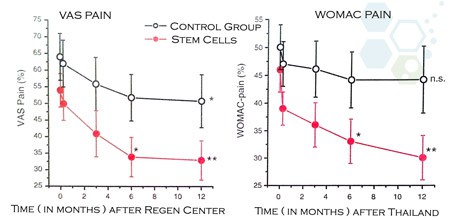
Results After Stem Cell Therapy for Knee
Cost to treat Knee osteoarthritis & Knee injuries
Due to the varying degrees of injuries, our orthopedic team must conduct a virtual consultation with all potential patients. This can be done online using the patient’s current medical records, such as recent Radiology tests (MRI scans or CT Scans) and reports from the patient’s primary care orthopedic doctors. Once the review is complete, we can know if the patient is a candidate and provide a detailed plan that will include the exact number of days required in Bangkok, along with fixed and total medical-related costs.
If you or a loved one is suffering from joint pain, degenerative knee conditions, knee injuries, difficulty standing up or walking stairs, or are considering stem cell therapy instead of knee replacement surgery, contact us for a second opinion. To learn more, please contact us today.
Published Clinical Citations
[1] ^ Davatchi, Fereydoun, Bahar Sadeghi Abdollahi, Mandana Mohyeddin, and Behrooz Nikbin. 2015. Mesenchymal stem cell therapy for knee osteoarthritis: 5 years follow-up of three patients. International journal of rheumatic diseases, no. 3 (May 20). doi:10.1111/1756-185X.12670. https://www.ncbi.nlm.nih.gov/pubmed/25990685
[2] ^ Kasemkijwattana, Channarong, Suradej Hongeng, Suraphol Kesprayura, Visit Rungsinaporn, Kanda Chaipinyo, and Kosum Chansiri. 2011. Autologous bone marrow mesenchymal stem cells implantation for cartilage defects: two cases report. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 3. https://www.ncbi.nlm.nih.gov/pubmed/21560849
[3] ^ Turajane, T, T Thitiset, S Honsawek, U Chaveewanakorn, J Aojanepong, and K I Papadopoulos. 2013. Assessment of chondrogenic differentiation potential of autologous activated peripheral blood stem cells on human early osteoarthritic cancellous tibial bone scaffold. Musculoskeletal surgery, no. 1 (November 1). doi:10.1007/s12306-013-0303-y. https://www.ncbi.nlm.nih.gov/pubmed/24178764
[4] ^ Turajane, Thana, Ukrit Chaweewannakorn, Viroj Larbpaiboonpong, Jongjate Aojanepong, Thakoon Thitiset, Sittisak Honsawek, Juthatip Fongsarun, and Konstantinos I Papadopoulos. 2013. Combination of intra-articular autologous activated peripheral blood stem cells with growth factor addition/ preservation and hyaluronic acid in conjunction with arthroscopic microdrilling mesenchymal cell stimulation Improves quality of life and regenerates articular cartilage in early osteoarthritic knee disease. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 5. https://www.ncbi.nlm.nih.gov/pubmed/23745314
[5] ^ Uth, Kristin, and Dimitar Trifonov. 2014. Stem cell application for osteoarthritis in the knee joint: A minireview. World journal of stem cells, no. 5 ( 26). doi:10.4252/wjsc.v6.i5.629. https://www.ncbi.nlm.nih.gov/pubmed/25426260