Each kidney in the human body consists of about 1 million nephrons, which are basically “filtering” units. Every nephron features a glomerulus, a cluster of tiny blood vessels. Inside a kidney, toxins in the blood may be removed through the glomerulus structure. High blood sugar often thickens and damages the blood vessels, triggering the Kidney Failure process.
Warning Signs of Kidney Disease
Kidney Failure tends to disproportionately affect patients with other underlying medical conditions such as cardiovascular disease, Polycystic Kidney Disease, polyneuropathy, pancreatitis, or Type 2 Diabetes Mellitus. Doctors believe that sustained uncontrolled high blood sugar (and also high blood pressure) is the leading cause of kidney failure for most people. Not all diabetic patients have to suffer from eventual failure requiring a transplant or emergency reversal of kidney disease with stem cells. The kidneys function by eliminating excess fluids from the blood through our urine. When kidneys start to fail, this function gets disrupted. More fluids start collecting in the body. Then, the swelling begins. Patients often report having swollen eyes and legs. After some time, the entire body might swell up.
Protein in Urine (Proteinuria)
Patients lose appetite when excess fluids and waste aren’t naturally removed from the body. They might even start frequently vomiting as the body struggles with the excess stored waste. As the kidney begins to lose functions, other symptoms, such as retaining essential proteins in the blood supply called proteinuria, take hold. Proteinuria can be easily discovered with a simple urine test. Kidney disease patients who also have Diabetes can find that their urine turns out to be a little foamy in appearance. Learn more about kidney-friendly diets.
Types of Renal Diseases
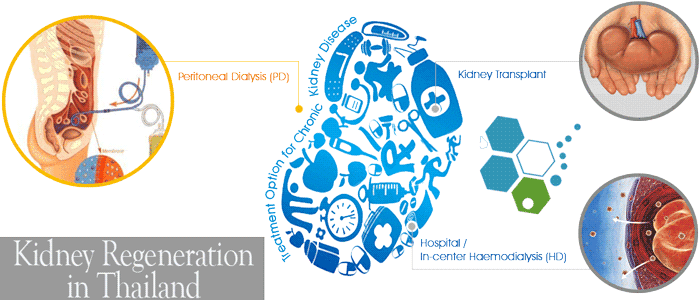
Chronic kidney disease (CKD)—As the name implies, CKD develops over a long period, and patients often track the reduction of kidney function over several years. Progressive CKD can lead to eventual kidney failure (end-stage kidney disease) and requires either a kidney transplant or kidney hemodialysis 1-3 times a week to stay alive. Dialysis or the Hemofiltration machine is needed to purify a patient’s blood of waste products such as urea or creatinine since the kidneys cannot work correctly.
There are many potential causes of chronic kidney disease, but the usual ones include:
- Glomerulonephritis – Attack on the kidney tissue by a disease, virus (kidney infection symptoms), or self-attack, i.e., Autoimmune responses such as Crohn’s & Goodpasture syndrome
- Polycystic kidney disease (PKD) which causes the growth of cysts on the kidneys
- IgA nephropathy autoimmune, or Berger’s disease, is diagnosed when immunoglobulin A (IgA antibody) builds kidney inflammation.
- Damage to blood vessels to either kidney due to diabetes (Diabetic Nephropathy) or high blood pressure, known as Renovascular hypertension (RVH), which can also lead to congestive heart failure
- Genetic or congenital abnormalities caused by mutations in the person’s DNA affecting the urinary tract or kidney
- Renal cell carcinoma (RCC) & Kidney Cancer
- Reflux nephropathy, which causes urine to flow back into the kidneys
- Long-term exposure to drugs or medications that are toxic to the kidneys
- Long-term exposure to Lead poisoning or heavy metals
- Renal artery stenosis (RAS) which causes narrowing of the renal arteries
Acute Renal Failure
Acute renal failure (ARF) or Acute kidney injuries (AKI) occur after a sudden or abrupt loss of kidney function. The dangerous event usually occurs over an extremely short period (2- 7 days) and can be numerous. Some common causes of Acute kidney failure include:
- Recurrent kidney stones
- “Anaemia” Low blood count from kidney disease
- SLE Lupus & refractory lupus nephritis
- Sudden Stoppage of Haemodialysis
- Frequent urinary tract infections
- Renal artery stenosis
- Stopping Peritoneal dialysis
- Toxicity due to chemotherapy agents
- Interstitial nephritis
- Acute kidney failure – Sudden
- Protein or Blood in the urine
- Chronic or long-term Dialysis at a Hospital
- Kidney damage due to high blood pressure
- Polycystic kidneys
- Electrolyte imbalance
- Chronic kidney disease (CKD)
There can be many other causes of chronic kidney disease, and sometimes the diagnosis is idiopathic or unknown, but it is more common among men with ankylosing spondylitis. Regardless of the underlying cause of CKD, the approaches to treatments to improve the glomerular filtration rate (GFR) are usually similar. Recent research also suggests that nephrotic syndrome & chronic kidney disease can increase the risk of getting Parkinson’s disease or secondary parkinsonism.
Five Stages of Kidney Disease
There are five stages of kidney damage for patients diagnosed with Chronic kidney disease (CKD). In nephrology, the stages vary from mild kidney damage in Stage 1 to total kidney failure in Stage 5. The stages of patient kidney disease are based on the Estimated Glomerular Filtration Rate (eGFR). eGFR score is used to gauge how well the kidneys filter waste and excess fluid out of the blood. In the early onset stage of renal disease, the kidneys are still functional and can filter out waste but are inefficient. As the disease progresses, it becomes harder and harder for the kidneys to filter waste, and eventually, it stops working altogether and requires artificial blood filtering using a dialysis machine.
Calculating Your GFR
Genetic Testing for Kidney Diseases
Knowing the underlying causes of renal failure and kidney disease is very important, not only for the patient but also for their family members who may be carrying the gene without knowing. The Regeneration Center offers genetic screenings for congenital kidney diseases and tests for several ciliopathies, nephronophthisis (NPH), Nephrolithiasis (renal calculi – -cysts), or a second opinion to confirm a diagnosis for hereditary kidney disease. Genes we can test for include:
ANKS6, AGXT, APRT,ADCY10, AHI1, ATP6V0A4, ATP6V1B1, CC2D2A,CA2, CASR, CLCN5,CEP164, CEP290,CLDN16, CLDN19, CEP83, CYP24A1, DCDC2,FAM20A, GPHN, GRHPR,GLIS2, IFT172, INVS, HOGA1, HPRT1, KCNJ1, IQCB1, NEK8, NPHP1, NPHP3,MOCOS, MOCS1,OCRL, PREPL, SLC12A1, SLC22A12, SLC26A1, SLC2A9,NPHP4, OFD1, PKHD1,SLC34A1, SLC34A3, SLC3A1,SLC4A1, SLC7A9,RPGRIP1L, SDCCAG8, TCTN1,RPGRIP1L, SDCCAG8, TCTN1,TMEM216, TTC21B, TMEM237, TMEM67,WDR19, XPNPEP3, XDH, SLC9A3R1, UMOD, VDR & ZNF423
The Regeneration Center does not have kidney transplant surgery or gene therapies for kidney diseases; DNA testing services are for current patients. Please contact us with any questions.
Clinical studies have shown that red blood cells carry oxygen from the lungs to provide the body’s requirements and energy for day-to-day activities. Nevertheless, a failing kidney cannot secrete sufficient erythropoietin, and lower erythropoietin levels do not stimulate the bone marrow to produce more red cells, resulting in anemia. Patients with anemia might notice pale skin or gums in the mouth.[1]
Can Kidney Disease be Reversed?
Stem Cell Kidney Regeneration
Stem cells are the human body’s repair mechanism. Stem cells can differentiate into any functional tissue cells. Kidney cell necrosis or  decreased kidney functions can be seen in abnormal creatinine levels. Stem cell Transplants for Renal Failure help to replenish the required kidney cells and thus promote a more normal, healthy kidney function. Two types of stem cell treatments may be utilized in our regenerative protocols for reversing Renal failure. One part of the treatment is focused on promoting optimal kidney function, and the other would be replenishing red blood cell amounts to help reverse the decline in HGB level. The enhanced mesenchymal cells are then transfused back into your body through targeted cell infusions that allow the circulating stem cells to reach the kidneys via normal blood circulation. This breakthrough treatment for renal failure can be done with and without dialysis and demands no surgical operation that requires extended hospital stays only at the Regeneration Center. The enhanced mesenchymal stem cells used for kidney disease are done in multiple stages, but each daily session takes about two hours each visit.[2]
decreased kidney functions can be seen in abnormal creatinine levels. Stem cell Transplants for Renal Failure help to replenish the required kidney cells and thus promote a more normal, healthy kidney function. Two types of stem cell treatments may be utilized in our regenerative protocols for reversing Renal failure. One part of the treatment is focused on promoting optimal kidney function, and the other would be replenishing red blood cell amounts to help reverse the decline in HGB level. The enhanced mesenchymal cells are then transfused back into your body through targeted cell infusions that allow the circulating stem cells to reach the kidneys via normal blood circulation. This breakthrough treatment for renal failure can be done with and without dialysis and demands no surgical operation that requires extended hospital stays only at the Regeneration Center. The enhanced mesenchymal stem cells used for kidney disease are done in multiple stages, but each daily session takes about two hours each visit.[2]
Stem Cells Therapy for Chronic Kidney Disease
For those suffering from moderate to late/terminal stage kidney failure, allogeneic cell therapy can help them by eliminating the need for dialysis or decreasing the frequency of dialysis. For patients with early-stage renal failure or kidney disease, stem cell therapy can reverse kidney damage and prevent further damage to renal function. Our functional regenerative medical treatments using enhanced renal stem cells assure the patients that they will continue living their normal lives without worrying about the worsening of their kidneys or spreading to cause other issues such as heart disease (heart attacks), pancreas failure (diabetic nephropathy), and other complications.[3]
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Kidney Disease, Chronic Kidney Disease (CKD), Acute Kidney Injury (AKI), or Renal Failure with stem cells. Patients with advanced kidney damage, severe comorbidities, or other significant health issues might not be good candidates for treatment.Avoid Dialysis or Kidney Transplant
Stem cell research has shown that to avoid dialysis or a kidney transplant after a diagnosis of chronic kidney disease (CKD), early detection and comprehensive management are crucial. Lifestyle modifications, such as maintaining a healthy diet low in sodium, potassium, and phosphorus, help reduce the kidney burden. It’s essential to control blood pressure and blood sugar levels, as hypertension and diabetes are leading causes of CKD progression. Medications like ACE inhibitors or ARBs may be prescribed to help protect kidney function. Staying well-hydrated, avoiding nephrotoxic medications (like NSAIDs), and addressing underlying health conditions that contribute to kidney damage are also important. Regular monitoring by a nephrologist, coupled with careful management of complications such as anemia and electrolyte imbalances, helps slow CKD progression. For patients with advanced disease, considering regenerative therapies or stem cell interventions may provide new opportunities for slowing or reversing damage, though these are still emerging areas of treatment. Finally, maintaining an active lifestyle and a healthy weight can significantly reduce the risk of worsening kidney function and help avoid the need for dialysis or transplant.
Stop Failing Kidneys with UC-MSC+ Renal Stem Cells
The protocol needed to treat kidney patients depends entirely on factors such as patient age, health, and stage of kidney damage. Candidates for treatment will require several stage infusions of enhanced UC-MSC+ Renal Stem cells derived from Cord tissue-derived stem cells along with renal system-specific growth factors, which are isolated and cultured in our lab. Due to varying degrees of kidney function and physical degeneration, our medical team must review the patient’s current medical test results. Once the review is complete, we can offer a detailed treatment plan that includes the complete treatment steps, the exact number of nights required, and the total and fixed medical-related costs.
Type of Stem Cell Delivery Methods Needed for Kidney Disease: The types and quantities of cells needed are based on the patient’s medical needs. The Regeneration Center offers both autologous (from patient) and allogeneic stem cells using clinical grade umbilical cord mesenchymal stem cells (UC-MSC+) delivered in a multi-stage treatment using a combination of Intravenous Injections (IV Drips), Intrarenal Injections, Intraperitoneal Injections with regenerative growth factors (for assisting with homing) or Intra-arterial Injections to improve delivery efficiency and allow for higher concentration of renal stem cells to reach the affected areas in the renal system, and helping to enhance the overall therapeutic effects. Renal cell transplants using allogeneic do not require dangerous surgeries or painful extraction methods. To achieve better results, The Regeneration Center has developed a mix of regenerative growth factors to enhance regenerative kidney treatments that could support kidney repair and improve outcomes. The growth factors we use are renal function-specific proteins that play crucial roles in retaining transplanted cells, promoting stem cell proliferation and cell differentiation, increasing cell survival, promoting tissue regeneration, and boosting paracrine cell signaling. [4]
Rehabilitation Options Post Treatment: Physical Rehabilitation therapy in Bangkok is typically not required unless there are other physical issues. Complete physical rehab services post-therapy can be provided upon request for 2-4 hours per day and up to 5 days per week. Medical travel visas and accommodations at a hotel or extended-stay apartment for the patient and family can also be provided upon request.
Total Treatment time needed: The protocol is estimated to take two weeks (depending on the severity and stage of diagnosis). Late-stage kidney patients or patients with frequent dialysis may not qualify for treatment or require multiple stages to be effective in cessation of dialysis and reversing kidney disease.

Kidney Disease Treatment Guidelines for 2025
Our non-surgical cell-based treatment for renal failure & kidney dysfunction will require a minimum of 14 nights in Bangkok. Due to the varying degrees of Kidney damage and the stage/severity of the underlying disease, our medical team and nephrologists will need to evaluate a patient’s needs before medical recommendations can be made and detailed treatment protocol can be provided. Upon approval and acceptance, a thorough treatment plan will be provided, including specifics and a daily calendar for the entire treatment plan, along with the fixed medical-related expenses (excluding accommodations or flights). To begin the qualification process for our multi-stage treatment protocol for CKD, Polycystic Kidney disease, or Kidney/Renal Failure, please prepare your recent medical records that include Radiology from CT Scan or Renal Ultrasound along with biopsy results (if available) and biochemistry results (blood tests) and contact us today.
Published Clinical Citations
[1] ^ Tangnararatchakit, Kanchana, Wiwat Tirapanich, Usanarat Anurathapan, Wiwat Tapaneya-Olarn, Samart Pakakasama, Saengsuree Jootar, Shimon Slavin, and Suradej Hongeng. Depletion of alloreactive T cells for tolerance induction in a recipient of kidney and hematopoietic stem cell transplantations in Thailand. Pediatric transplantation, no. 8 (May 4). doi:10.1111/j.1399-3046.2012.01701.x. https://www.ncbi.nlm.nih.gov/pubmed/22553996
[2] ^ Sumboonnanonda, Achra, Kleebsabai Sanpakit, and Nuntawan Piyaphanee. 2008. Renal tubule function in beta-thalassemia after hematopoietic stem cell transplantation. Pediatric nephrology (Berlin, Germany), no. 1 (August 8). doi:10.1007/s00467-008-0949-0. https://www.ncbi.nlm.nih.gov/pubmed/18688653
[3] ^ Tögel, Florian, Arthur Cohen, Ping Zhang, Ying Yang, Zhuma Hu, and Christof Westenfelder. 2009. Autologous and allogeneic marrow stromal cells are safe and effective for the treatment of acute kidney injury. Stem cells and development, no. 3. doi:10.1089/scd.2008.0092. https://www.ncbi.nlm.nih.gov/pubmed/18564903
[4] ^ Townamchai, N, K Praditpornsilpa, and S Eiam-Ong. 2010. Endothelial progenitor cells in Thai kidney transplant patients. Transplantation proceedings, no. 5. doi:10.1016/j.transproceed.2010.01.063. https://www.ncbi.nlm.nih.gov/pubmed/20620502