Cell Immunotherapy for Prostate cancer is a promising new approach to treating cancers that otherwise did not respond well to traditional treatments, surgeries, or chemotherapy. The basic goal of all immunotherapies, checkpoint inhibitors, and cancer vaccines is to program the body’s own immune system to recognize and destroy only cancer cells as the enemy.
Modified Immune Cells to Fight Prostate Cancer
What is Prostate Cancer?
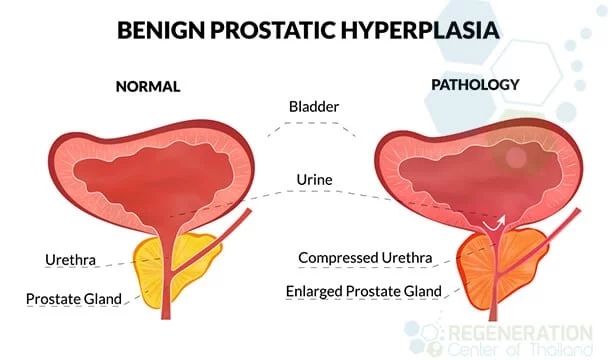
The prostate is a tubuloalveolar exocrine gland the size of a ping-pong ball (when healthy). This reproductive gland’s purpose is to produce and store semen. A prostate is located in front of the rectum and below the bladder around the upper urethra tube that empties urine produced by the bladder. Because of its location, diseases of the prostate affect both sexual function and bladder control. Prostate diseases can be cancerous or noncancerous and can affect blood vessels and peripheral nerves that control erectile function, leading to ED. Prostate cancer (PC) is a medical diagnosis of abnormal cell growth/division (malignancy) in the prostate gland. If left untreated, cancer of the prostate can spread (metastasize) to other areas in the body, including:
- Lymph nodes
- Secondary Liver Cancer
- Lungs
- Bladder
- Lower urethra
- Pleural mesothelioma
- Bones
- Kidney Cancer
- Pancreas
- Rectal cancer
Metastasized prostate cancer is considered an advanced form of cancer and can even travel to the brain; however, this is very rare.
Stem Cell therapy for Prostate Cancer
What is Prostate Cancer?
The prostate is a tubuloalveolar exocrine gland the size of a ping-pong ball (when healthy). This reproductive gland’s purpose is to produce and store semen. A prostate is located in front of the rectum and below the bladder around the upper urethra tube that empties urine produced by the bladder. Because of its location, diseases of the prostate affect both sexual function and bladder control. Prostate diseases can be cancerous or noncancerous and can affect blood vessels and peripheral nerves that control erectile function, leading to ED. Prostate cancer (PC) is a medical diagnosis of abnormal cell growth/division (malignancy) in the prostate gland. If left untreated, cancer of the prostate can spread (metastasize) to other areas in the body, including:
- Lymph nodes
- Secondary Liver Cancer
- Lungs
- Bladder
- Lower urethra
- Pleural mesothelioma
- Bones
- Kidney Cancer
- Pancreas
- Rectal cancer
Metastasized prostate cancer is considered an advanced form of cancer and can even travel to the brain; however, this is very rare.
Stem Cell therapy for Prostate Cancer
Global Prostate Cancer Statistics
Prostate cancer is currently the #1 most common type of cancer in men (after skin cancer), and statistics show that 1 in 9 men will be diagnosed with prostate cancer during their lifetime. Generally speaking, Prostate cancer is much more common in men over the age of 50 and is typically quite rarely diagnosed in men less than 40 years old. Prostate Cancer is currently the 2nd leading cause of cancer-related deaths in the world (behind pulmonary cancer), and it is estimated that 1 in 40 men will die from having prostate cancer.[1]
Recent Epidemiological studies have shown some distinct geographical and racial distribution for men with prostate cancer and that this disease is more prevalent in Western societies than Asian ones, such as Thailand, where prostate cancer is the 6th leading type of cancer [2] The highest rates of prostate cancers were found in Western and Northern European nations such as France and Norway and also in New Zealand, Australia, and North America.
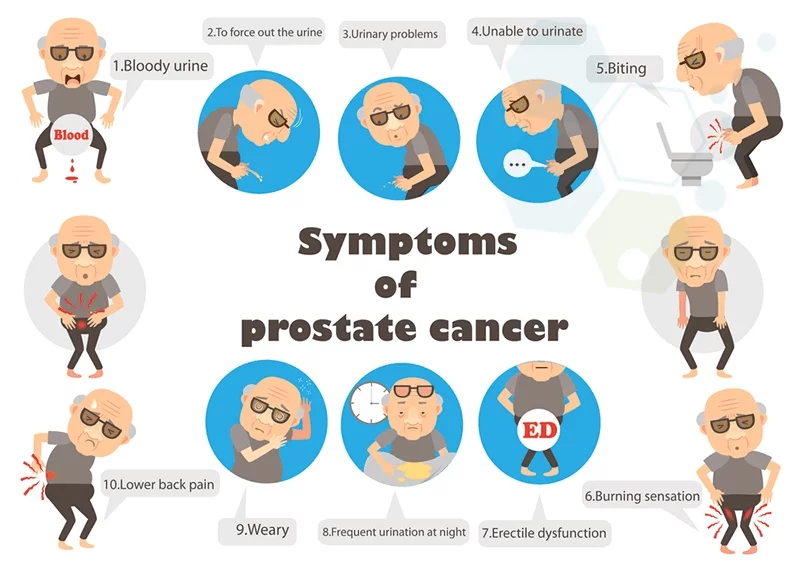
Signs and Symptoms of Prostate Cancer
Early intervention and detection are the key to dealing with Prostate cancer, as the symptoms do not usually show themselves in the very early stages of the disease. PC symptoms are different for every man; sometimes, these early symptoms may be caused by other conditions. It’s estimated that less than 5% percent of patients with prostate cancer show early warning symptoms in standard urine tests. For this reason, routine screenings focusing on early detection are essential. Prostate-specific androgen (PSA) and Digital rectal exams (DRE) are recommended for all men over 50 years old and possibly earlier if you have a family history of the disease. The symptoms of Prostate cancer often mimic those or other issues, so a small percentage of patients are not diagnosed with prostate cancer until it has metastasized to different areas in the body.
Early warning signs of Prostate Cancer include:
- Anemia: The patient blood does not have enough hemoglobin (healthy red blood cells) due to bone marrow infiltration by the cancerous cells, treatment-related toxic exposure, or androgen deprivation
- Severe Abdominal pain: Consistent pressure on organs surrounding the swollen prostate gland causes soreness and pain in the lower abdomen.
- Blood in Semen: Infection or inflammation of the prostate causes blood to appear in the semen
- Hematuria (Blood in urine): Cancer in the urinary tract can cause blood to appear in the urine. These symptoms can also occur in patients with kidney failure, kidney cysts, or infection in the urinary tract.
- Issues with incontinence or frequent need to urinate: Enlarged prostate glands due to a tumor near the urethra can cause bladder control issues, urine retention issues, incomplete or trouble starting urination, and a weak stream of urine.
- Inflammation in Legs: swelling in the Legs is caused if PC tumors metastasize in the bladder and block urine from the kidneys.
- Frequent Fatigue: This can be caused by traditional chemotherapy or medication-based treatments, depression, or stress that leads to a lack of appetite.
- Rapid Weight loss Can be caused by side effects of medical treatments that cause a lack of appetite, which leads to weight loss.
- Spinal compression or Pain in the Lower Lumbar Spine: Sometimes misdiagnosed as Degenerative Disc Disease, pain in the Lower lumbar or hips can occur when cancer spreads to the bone, causing the spinal cord to be compressed, leading to pain
Advanced Symptoms of Prostate Cancer
 Patients with late-stage prostate cancer have more complications that lead to much more severe symptoms, primarily when cancer metastasizes to other parts of the body. For example, If prostate cancer metastasizes to the bones, the patients can experience severe bone pain, pressure sensitivity, and fracture easily like patients who have osteoporosis. Other issues like Kidney Failure can also occur if cancer metastasizes to the ureter ducts that carry urine from the bladders. Each cancer patient has unique needs and circumstances that lead to advanced symptoms, including factors such as:
Patients with late-stage prostate cancer have more complications that lead to much more severe symptoms, primarily when cancer metastasizes to other parts of the body. For example, If prostate cancer metastasizes to the bones, the patients can experience severe bone pain, pressure sensitivity, and fracture easily like patients who have osteoporosis. Other issues like Kidney Failure can also occur if cancer metastasizes to the ureter ducts that carry urine from the bladders. Each cancer patient has unique needs and circumstances that lead to advanced symptoms, including factors such as:
- Patient’s overall health
- Patient age
- Family history
- Stage of the cancer
- Spread of cancer (metastasized) to other areas
Stages of Prostate Cancer
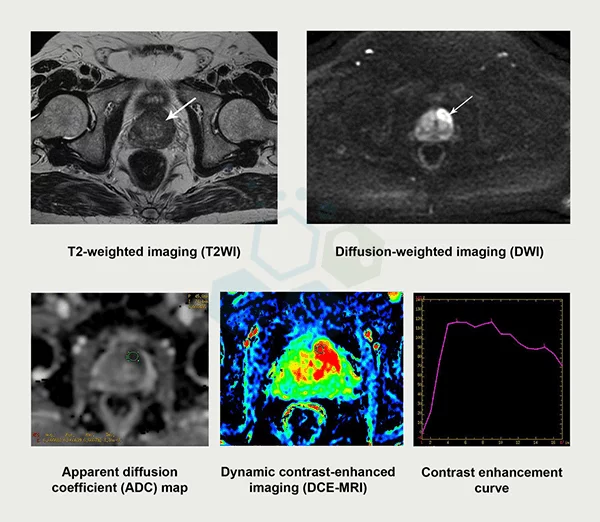
Most urologists describe the spread and growth of prostate cancer in one of 4 stages. Urologists and treatment providers often use the stage of cancer as a guide when offering a prognosis or choosing treatment options. The four stages of Prostate cancer are based on a variety of factors, including screening tests such as:
- DRE (digital rectal exam)
- Prostate-specific antigen (PSA)
- Prostate Biopsies
- Imaging tests from MRI scan, CT scan, bone scan, or transrectal ultrasound
To determine the stage of prostate cancer, most urologists around the world start with the “TNM staging system,” which helps define the different aspects of prostate cancer growth.
- T – the T component is used to measure the size & extent of the Tumor
- N – the N component is used to measure if and how far the prostate cancer has spread to Bone or Lymph Nodes
- M – the M component is used to measure if the prostate cancer has spread to any other organs (Metastasized)
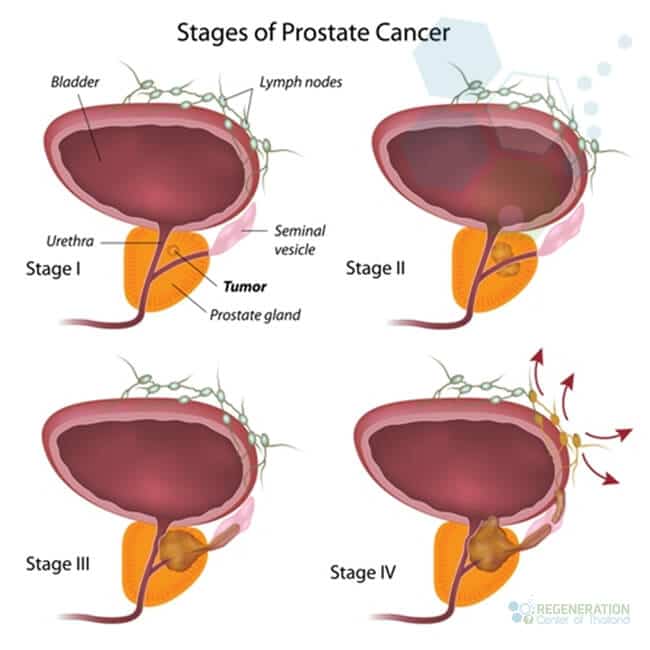
After a urologist calculates the TNM components, it will often be combined with the Gleason grading system to determine which stage of prostate cancer the patient is currently in. Prostate cancer survival rates are often based on the actual stage and timing of the diagnosis.[3]
- Stage 1 (I) Prostate Cancer
In stage 1, a tumor is usually not detectable by radiology tests or physical exams and has not metastasized outside of the prostate gland. Early discovery of prostate cancer is the key to long-term survival as the 5-year survival rate for patients with Stage 1 is nearly 100% after five years. Most patients choose to have an external beam brachytherapy ( radiation therapy ) or radical prostatectomy to treat the condition. - Stage 2 ( IIA and IIB) Prostate Cancer
In Stage 2, a prostate cancer tumor may or may not be detected through radiology scans or a physical examination but still has not metastasized outside of the prostate gland. However, Stage 2 cancer cells can grow significantly quicker and must be treated immediately. Treatment options for stage 2 can include Radical prostatectomy with the removal of lymph nodes, external beam radiation therapy, Brachytherapy, or prostate cancer immunotherapy. - Stage 3 (III) – Prostate Cancer
In Stage 3, the prostate cancer has usually metastasized beyond the prostate gland but has not yet reached the rectum or bladder but is more likely to return than the earlier stages 1 and 2. Treatment options for Stage 3 include hormone therapy with External beam radiation, external beam plus brachytherapy, Radical prostatectomy, or Immunotherapy for prostate cancer. - Stage 4 (IV) – Prostate Cancer
Stage 4 prostate cancer is the last stage and describes a tumor that has metastasized to other parts of the patient’s body, including the lungs, bones, lymph nodes, liver, or bladder. Generally speaking, the 5-year survival rate for patients with Stage 4 prostate cancer is 27%. Treatment options for Stage 4 prostate cancer include chemotherapy, hormone therapy with External beam radiation, external beam plus brachytherapy, Transurethral resection of the prostate (TURP), Laparoscopic radical prostatectomy, robotic prostatectomy or Immunotherapy for prostate cancer.
Traditional Treatment Options for Prostate Cancer
Currently, the most widely used traditional treatment options for men with prostate cancer are:
- Radiation Treatment
- Prostate Cancer Surgery
- Brachytherapy – Low-dose-rate seed implants and high-dose-rate seed implants
- Cryotherapy
- Chemotherapy ( metastasized )
- Androgen deprivation therapy (ADT) uses hormone blockers such as Casodex (Bicalutamide), Eulexin (Flutamide), Nilandron (Nilutamide), or Lupron.
For patients with slow-growing prostate cancers that are detected early, active surveillance is used to monitor the tumor for any significant (negative) signs. For others, prostate cancer surgeries are usually recommended. Some common laparoscopic or open surgeries include radical prostatectomy or salvage radical prostatectomy for recurrent cases and can be done by themselves or combined with other treatments such as radiation therapy (Radiotherapy.)
Some common types of Radiotherapy include:
- Stereotactic high-precision radiosurgery (like CyberKnife)
- Intensity-modulated radiation therapy (IG-IMRT)
- Stereotactic hypofractionated accelerated radiation therapy (SHARP)
For patients with small, localized (non-metastasized) prostate tumors, non-invasive techniques like partial gland ablation, Cryotherapy, focal therapy, and Brachytherapy can be used to target small areas of the prostate. Still, the recurrence rates are pretty high and may not be the ideal solution to get rid of cancer.
For patients with aggressive prostate cancers, combined treatments are often recommended that include a mix of radiation, brachytherapy, hormone therapy, or external beam therapy to try to reduce the overall adverse effects of radiation exposure.
For high-risk patients or patients where cancer has spread outside the prostate, the traditional approach is to use chemotherapy, systemic therapies, hormonal therapy, biologics, or bone-targeted therapy with mixed results.
Risks of Prostate Surgery
The Side effects and risks of prostate surgery like radical prostatectomy can be high and in line with any major surgery. Problems and risks of surgery can include:
- Excessive Bleeding from the surgery
- Adverse Reactions to anesthesia
- Damage to surrounding organs
- Blood clots in the lungs or legs
- Infections near the area of surgery.
Common Side effects of having Prostate Surgery
The significant side effects of having radical prostatectomy surgery include:
- Urinary incontinence – total loss of bladder control
- Erectile dysfunction, Loss of fertility, and permanent impotence
- Lymphedema – swelling caused by a buildup of lymph fluid
- An inguinal hernia – retropubic radical prostatectomy (RRP)
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Prostate Cancer with stem cells, immunotherapy, or targeted therapies. Patients with advanced metastatic disease, significant prostate enlargement, or other major health complications might not be good candidates for the estimated 3-5 week treatment.Alternative Treatment Option for Prostate Cancer
At the Regeneration Center, our team of experts seeks to provide a well-rounded integrative approach to the treatment of prostate cancer. Our goal is for Long-Term Remission of prostate cancer and Therapy-Resistant Cancers that traditional therapies are unable to solve.[4] Our safe and effective Biological treatment plans are individualized to the patient’s needs without the excessive risks of radiation or surgical treatment approaches. Our holistic approach is built on the power of functional medicine. It combines research-based alternative medicines and regenerative medicine with conventional treatments for prostate cancer, offering patients the optimal chances for success.
Immunotherapy for Prostate Cancer
Our modern and non-toxic immunotherapy protocols, such as Transurethral Prostate Hyperthermia (TUH), are specifically designed to help restore the body’s defense mechanisms and immune system, only to recognize and destroy cancer cells. The patient’s immune cells are first collected in leukapheresis and then cultured with specific proteins that activate themselves after being reintroduced to the patient’s body and immune system.[5]
CAR-T cell therapy for Prostate Cancer
This targeted Immunotherapy for cancer of the prostate has very little to no adverse effects and is often combined with other forms of modern Biological therapies such as:
- Anti-angiogenic treatments – to stop the VEGF receptors in the body from sending growth signals to the blood cells
- Oncolytic virus therapy (OVT Therapy)—This Viral Immunotherapy uses genetically modified viruses to target and kill cancer cells. It is also known as Rigvir Viral Therapy.
- Chimeric antigen receptor-engineered T cells ( Car-T Cells) – Uses patient’s immune cells enhanced in our lab. The CAR T cells are then reintroduced to the patient to target specific proteins and fight prostate cancer.
- Dendritic Immunotherapy
- Cancer Stem cells
- NK Cells – Natural Killer Cell Therapy
Safe Non-Toxic Treatment For Prostate Cancer Stage I-IV
The Regeneration Center Immunotherapy for Cancer focuses on many factors, including the tumor microenvironment, as it is pivotal in the remission or progression of cancer. This integrative functional medical strategy has been proven to help improve overall outcomes of many cancer types in all stages. Browse our website or contact one of our support team directly to learn more about our cancer immunotherapy protocols and how they can be used effectively to achieve long-term prostate cancer remission for years, possibly decades.
Our Prostate cancer treatment and research center continues to probe further than ever before. With discoveries, clinical trials for prostate cancer, and emerging methods of diagnosing using genetic screening before treating prostate cancers, we firmly believe that we are well on our way to managing an otherwise fatal to allow our patients to live a cancer-free life without constant fear of relapse.
Stem Cell Treatment for Prostate Cancer in 2025
To determine eligibility and get exact prices along with a day-by-day treatment outline, our oncologists will need to better understand the patient’s existing needs via recent histological results, Biopsies, blood tests, x-rays, or radiology scans from your primary care urologist or oncologist.
If you or a loved one has been diagnosed with prostate cancer, be aware of alternative medical solutions to fight cancer using HSC+-modified immune cells. Take the first step toward treatment by allowing your care to be handled by our team of experts in our advanced facility. We are here to help. To learn more about the safe and effective alternative treatment for Prostate Cancer, please contact us today.
Published Clinical Citations
[1] ^ Lojanapiwat, Bannakij, Choosak Pripatnanont, Vorapot Choonhaklai, Surithorn Soontornpun, Supon Sriplakich, Sunai Leewansangtong, Apirak Santi-Ngamkun, et al. 2017. Management of metastatic castration-resistant prostate cancer: Insights from urology experts in Thailand. Prostate international, no. 1 (January 11). doi:10.1016/j.prnil.2017.01.002. https://www.ncbi.nlm.nih.gov/pubmed/28352616
[2] ^ Janiczek, Marlena, Łukasz Szylberg, Anna Kasperska, Adam Kowalewski, Martyna Parol, Paulina Antosik, Barbara Radecka, and Andrzej Marszałek. 2017. Immunotherapy as a Promising Treatment for Prostate Cancer: A Systematic Review. Journal of immunology research (October 3). doi:10.1155/2017/4861570. https://www.ncbi.nlm.nih.gov/pubmed/29109964
[3] ^ Bilusic, Marijo, Ravi A Madan, and James L Gulley. 2017. Immunotherapy of Prostate Cancer: Facts and Hopes. Clinical cancer research : an official journal of the American Association for Cancer Research, no. 22 (June 29). doi:10.1158/1078-0432.CCR-17-0019. https://www.ncbi.nlm.nih.gov/pubmed/28663235
[4] ^ Lojanapiwat, Bannakij. 2015. Urologic cancer in Thailand. Japanese journal of clinical oncology, no. 11 (September 9). doi:10.1093/jjco/hyv125. https://www.ncbi.nlm.nih.gov/pubmed/26355159
[5] ^ Pizzola, Christopher, Syed M Rizvi, and Monika Joshi. 2016. A New Era of Immunotherapy in Prostate Cancer. Current molecular pharmacology, no. 3. https://www.ncbi.nlm.nih.gov/pubmed/26177645