Pulmonary fibrosis is the thickening and scarring of the lung tissue. The term idiopathic denotes the cause is unknown and occurred spontaneously. Though it is not completely understood what causes idiopathic pulmonary fibrosis and diffuse parenchymal lung failure, the disease process is well-explained in various medical literature and case history.[1]
Healthy vs. Diseased Lungs
Interstitial Pulmonary Fibrosis
Diffuse parenchymal lung disease (DPLD) & Interstitial lung disease (ILD) are a group of lung diseases that affect the tissue and spaces around the air sacs (interstitium) in the lungs (alveoli). This family of various lung disorders occurs an injury to the lungs that fails to heal properly for various reasons. Areas of the lungs that are prone to injuries include:
- Pulmonary capillary endothelium
- Basement membrane – a specialized form of extracellular matrix (ECM)
- Alveolar epithelium – functional & physical barrier of dangerous environmental agents
- Perilymphatic lung tissue
- Perivascular tissue
Managing Alveolar Fibrosis – Fibroid Lung Disease
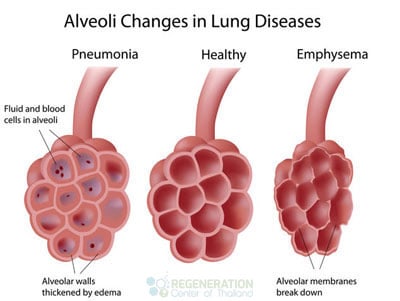
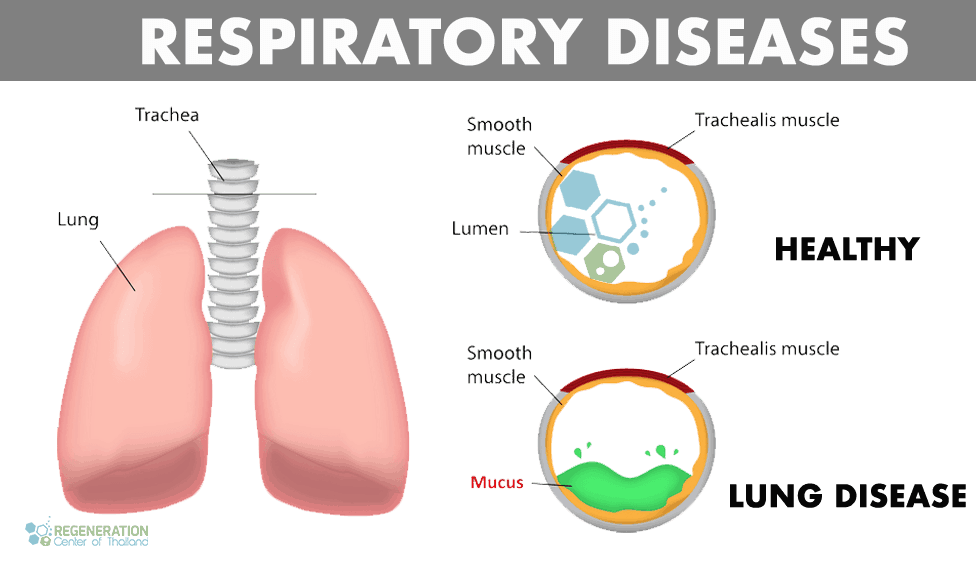
Under normal circumstances, the human body can initiate self-repair of the lungs using paracrine cell signaling but for some patients with interstitial lung disease, this normal lung repair process malfunctions resulting in the tissue around alveoli air sacs to thicken and become scarred. Thickened scarred lung tissue makes it difficult for oxygen to pass back into the bloodstream resulting in damage to both the entire cardiovascular system and lungs. The term Interstitial lung disease is used by pulmonologists to distinguish these types of lung diseases from others such as COPD and obstructive airways diseases. If left untreated, Interstitial lung disease results in fibrotic scarring of the lungs known as pulmonary fibrosis. Idiopathic pulmonary fibrosis usually gets diagnosed after radiographic lung scans start to show pleural-based fibrosis with honeycombing in the lungs and proliferating fibroblasts (fibroblastic foci.)
IPF and fibroid lung disease usually starts with a presence of inflammation in the alveoli. The alveoli are the tiny air sacs in the lungs where the exchange of carbon dioxide and oxygen happens. The fragile lining of the alveoli allows this gas exchange. Once these alveoli become inflamed and damaged in some way, the body’s reaction would be to activate the immune response and to heal the damaged alveoli.[2]
This causes scarring and thickening of the alveolar walls. Unfortunately, the thickened and scarred alveoli cannot perform efficiently during gas exchange. This ultimately leads to a lesser amount of oxygen that can be transported into the body and less carbon dioxide that can be expelled out.
Signs & Symptoms of Pulmonary Fibrosis
Some of the common signs and symptoms that are present in patients diagnosed with onset idiopathic pulmonary fibrosis are:
- Severe shortness of breath. This is caused by heart disease or the decreased amount of oxygen that the body gets due to the inefficient, affected alveoli. It gets worse with physical activity since the body is trying to get more oxygen.
- Constant Dry cough.
- Clubbing sensations of the finger and toenails. Clubbing is the swelling in the base of the finger and usually accompanied by cyanosis (bluish discoloration of the nails.) This is a sign of hypoxia or decreased level of oxygen in the tissue. This sign often manifests later on the disease progress and end-stage pulmonary fibrosis
- Aching muscles and joints
- Poor appetite and unexplained weight loss
- Reduction of lung capacity or airflow obstructions resulting in premature fatigue
- Frequent Chest Pain
- Constant tiredness and lingering fatigue
Causes of Lung Scarring – ILD & IPF
Since the underlying cause of Idiopathic lung fibrosis is often unknown, patients usually wonder how they get fibrotic scarring of the lungs. For most patients, the most common predisposing factors of developing interstitial pulmonary disease & alveolar fibrosis are:
- Cigarette smoking is a common cause of interstitial pulmonary fibrosis
- Genetic – Hereditary lung disease including fibrotic scarring of the lungs
- Exposure to various inorganic toxins, chemicals, and pollutants such as asbestos, beryllium (berylliosis), crystalline silica dust (silicosis)
- Exposure to organic compounds, dust, fungus or mold (hypersensitivity pneumonitis)
- Reaction to drugs or medications such as antibiotics, chemotherapy drugs & cardiac dysrhythmia medications (antiarrhythmic)
- Viral infections such as pneumocystis pneumonia (PCP), tuberculosis, atypical pneumonia, chlamydia trachomatis & syncytial virus
- GERD (Gastroesophageal reflux disease). This is when the stomach contents of a patient go back to the esophagus. There is a risk of aspiration of these stomach contents into the trachea, which can in turn cause lung infection.[3]
- Connective Tissue Disorders & autoimmune response due to conditions such as Lupus, rheumatoid arthritis, polymyositis, dermatomyositis, lymphangitic carcinomatosis, antisynthetase syndrome (inflammation) and systemic sclerosis
- Inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease
- Undifferentiated spondyloarthritis
- Idiopathic (non-identifiable)i.e. acute interstitial pneumonia (Hamman-Rich syndrome),Idiopathic pulmonary fibrosis & sarcoidosis
Diagnosing Pulmonary Fibrosis
The diagnosis of interstitial lung diseases and pulmonary fibrosis requires diagnostic tests and physical exams. A pulmonologist uses several diagnostic tools to understand the signs & better

Symptoms of patients with interstitial lung disease. Depending on the stage and severity of a patients condition lung specialists typically order the following tests:
- Pulmonary function tests for measuring decreased diffusion capacity (DLCO) to see if any restrictions exist
- Lung radiology scans using X-ray or High-Resolution Chest CT-Scans (HRCT) to check for patterns of opacities in lung tissue that are caused by the thickened and scarred lung tissues.
- An arterial blood test can be taken for examining the ability of the lungs to move oxygen into the tissues of the body.
- Lung biopsy: getting a sample of lung tissue and studying the sample to better identify areas of scarring or thickening or suggestive of any malignancy. Biopsies can include a trans-bronchial biopsy or the more invasive surgical lung biopsy.
- Genetic testing for pulmonary fibrosis and Cystic Fibrosis – May prevent the need for surgical lung biopsy
Screening for Mutations that may cause Familial Pulmonary Fibrosis
The Lung Regeneration center offers a comprehensive list of genetic screening tests for checking mutations in genes that lead to familial lung diseases. Tests for the following genes are currently available to screen for congenital autosomal recessive & autosomal dominant interstitial lung diseases:
ABCA3, FLCN, SFTPB, SFTPC,CSFR2A, CSFR2B, COPA,TSC1, TTF1, TSC2, DOCK8, STAT3, FoxF1, PGM3, SPINK5, METRS, MRS, MTRNS, CMT2U, ILFS2, ILLD, mENA, NISBD2, RTEL1, PIG61, ERBB, ERBB1, HER1, SPG70, TERC, TERT & PARN
Genetic screening tests are recommended for family members of patients who have already been diagnosed with. There are currently no available gene therapies to treat autosomal interstitial lung diseases, but there are several clinical trials underway with the hopes of one-day curing genetic lung diseases. To help reduce any risk of developing fibroid lung disease, ILD or Pulmonary fibrosis consider including pulmonary tests as part of your annual checkup, refraining from smoking and getting regular exercise to keep the lungs and heart as healthy as possible.
Traditional vs. Modern Treatments for ILD & Lung Fibrosis
In the past, there were traditionally minimal options for treating chronic progressive lung diseases such as COPD and idiopathic pulmonary fibrosis. Even today, there are several clinical trials for trying to cure interstitial lung diseases, familial pulmonary fibrosis and idiopathic lung sclerosis using modified gene therapies but as of today, there are no effective pharmaceutical medication based cures approved for treatments. In some cases, steroids are prescribed to help decrease the inflammation or mucomyst (Acetylcysteine) to reduce symptoms, but the effects are temporary and do nothing to the underlying cause of the disease. Lung transplants are another option for some but are considered very invasive, high-risk, and are usually only offered to advanced end-stage pulmonary fibrosis patients. Although it has its limitations, modified MSC+ lung stem cells offer a natural alternative to lung transplants for pulmonary fibrosis and anti-fibrotic medications.[4]
Treatment for Lung Fibrosis with Stem Cells in 2024
Stop Hardening of Lung Disease & Alveolar Fibrosis Naturally
Your Stem cells are essentially the bodies pharmacy. Stem cells are are the building blocks of your entire body. These types of potent cells are called “totipotent” cells as they can change/differentiate into any cell, tissue, or bone in the human body. When used properly, MSC+ Stem Cells can help with the loss of lung capacity/reduced lung function by focusing on the destroyed or limited linings of the alveoli that are at the root of the disease. [5] For various reasons (Cigarette smoking, Viral infections, genetics) the bodies natural ability to regenerate is being blocked causing the types of complications that manifest themselves as fibrosis and lung hardening disease.
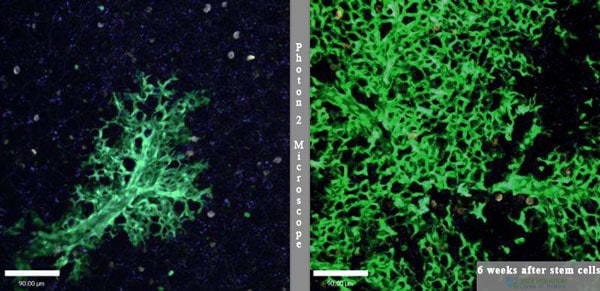
The Regen Center treatment for IPF lung sclerosis uses isolated & enhanced lung stem cells seeks to re-promote natural healing of the previously damaged alveoli cells, fibrotic scarring in interstitium lining of the lungs and scar tissue in lungs from pneumonia. The goal of the enhanced MSC+ stem cell treatment for pulmonary fibrosis and lung hardening disease is to assist the body in bypassing fibrotic scarring by regenerating new healthy tissues and blood vessels through a process called angiogenesis. The new lung regeneration treatment offers a safe, natural alternative to lung transplants by regeneration of lung tissue affected by fibrotic scarring and honeycombing through increased levels of myofibroblasts.
TREATMENT PRECAUTIONS & RISKS
Please Note That Stem Cell Treatments for IPF and Chronic Lung Diseases are not appropriate for all patients. Those with multiple conditions, late stage, or travel restrictions due to the need for constant Oxygen tanks may not qualify for the 2-3 week treatment protocol. Please contact us for details.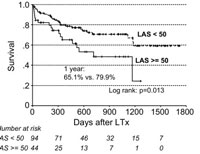
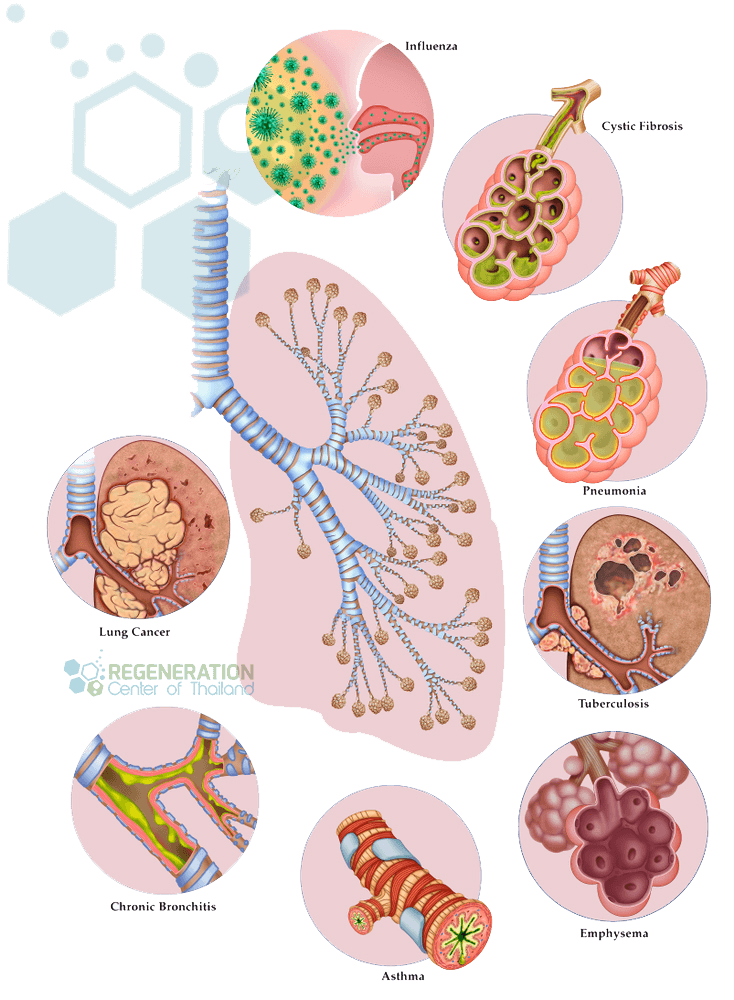
Multi-Stage Lung Cell Delivery for Respiratory Diseases
Interstitial lung diseases & progressive pulmonary fibrosis pose a significant challenge for pulmonologists and lung bioengineering. Diseases such as asthma, popcorn lungs “Bronchiolitis obliterans,” Idiopathic pulmonary fibrosis, lung cancer treatment, COPD, idiopathic interstitial pneumonia, Cystic fibrosis, emphysema & hyaline membrane disease are just some of the diseases that can be managed effectively via lung stem cell therapies. Due to the complexity and locations of the diseased regions, it can be challenging to effectively deliver cell therapeutic agents to the needed regions of the diseased lungs. The Lung Regeneration Center offers stem cells for lung disease patients using combination of MSC+ cells to stop rapid lung capacity decline. Our unique cell delivery methods targets the diseases from multiple vectors including guided radiography (when necessary), Intravenous, direct injection, Intrathecally and now for the first time via Intranasal inhalation for a painless and effective delivery of endogenous lung progenitor cells, lung epithelial stem cells to both the airway and vascular system of the lungs.
Stem Cell Treatment for Bronchiectasis
Bronchiectasis and bronchial fibrosis are often the leading cause of respiratory morbidity and mortality. As a medical diagnosis bronchiectasis severity is based on what the damage to the patients airways looks like. Some patients have cylindrical/ tubular fibrosis, while others have cystic or varicose. Tubular and Cylindrical bronchiectasis are usually the most common and most treated forms of bronchiectasis while cases of cystic bronchiectasis are more challenging and sometimes untreatable do to the irreversible destruction of lung bronchi and alveoli.
Stem cell treatment for bronchiectasis and bronchial fibrosis using a combination protocol of isolated mesenchymal stem cells (MSC+), bronchiolar epithelium and airway basal cells.
Guidelines for Treating Chronic Pulmonary Fibrosis
Total of MSC+ Stem Cell infusions will depend on the severity of restrictive lung disease, and multiple stages may be necessary for patients with scarring in interstitium of lung or diffuse parenchymal diagnosis. For optimal results, multiple methods of cell delivery will be required. Due to the progressively degenerative nature of restrictive lung diseases, most patients will require enhanced cell transplants derived from immune-compatible cells. For patients with multiple simultaneous issues, extensive honeycombing or severe respiratory failure, multiple treatments may be required. The isolated and expanded MSC+ lung cells used are pre-screened for infectious diseases, sterility, and potency. For patients with severe respiratory failure, aggressive combination treatment may be required.
Lung Regeneration Requirements & Lung Rehabilitation
Post-Treatment Lung Rehabilitation: Pulmonary rehabilitation services are optional but is highly recommended after any treatment. For local patients we can offer a complete integrative rehabilitation program in partnership with local hospitals in Bangkok. Pulmonary rehabilitation is also beneficial for patients who are experiencing severe difficulty in breathing or severe hardening of the lungs. Smoking is also much discouraged for patients with this condition, and active smokers will not qualify for our treatment. The rehab packages are available to all candidates as needed (2-5 hours per day, six days per week) . Medical treatment visas and hotel accommodations for long term stays can also be provided upon request.
Due to varying degrees of respiratory diseases, our pulmonary specialists will need to understand better the patients needs to qualify any potential candidates. Our initial review can be done online and takes around 7-8 business days for the medical assessment. Suitable candidates looking to reverse lung scarring naturally using Stem Cells will require a minimum of 2-3 weeks in Thailand. To begin the qualification process, please prepare your recent pulmonary tests such as spirometry exams, lung function tests, and radiology scans from MRI or (HRCT) High-Resolution chest CT scans and contacts us today.
Published Clinical Citations
[1] ^ Pongrakhananon, Varisa, Sudjit Luanpitpong, Todd A Stueckle, Liying Wang, Ubonthip Nimmannit, and Yon Rojanasakul. 2014. Carbon nanotubes induce apoptosis resistance of human lung epithelial cells through FLICE-inhibitory protein. Toxicological sciences : an official journal of Thailand Society of Toxicology, no. 2 (November 19). doi:10.1093/toxsci/kfu251. https://www.ncbi.nlm.nih.gov/pubmed/25412619
[2] ^ Liu, Ming, Dunqiang Ren, Dong Wu, Jian Zheng, and Wenwei Tu. 2015. Stem Cell and Idiopathic Pulmonary Fibrosis: Mechanisms and Treatment. Current stem cell research & therapy, no. 6. https://www.ncbi.nlm.nih.gov/pubmed/25986617
[3] ^ Ghadiri, Maliheh, Paul M Young, and Daniela Traini. 2015. Cell-based therapies for the treatment of idiopathic pulmonary fibrosis (IPF) disease. Expert opinion on biological therapy, no. 3 (December 15). doi:10.1517/14712598.2016.1124085. https://www.ncbi.nlm.nih.gov/pubmed/26593230
[4] ^ Chambers, Daniel C, Debra Enever, Nina Ilic, Lisa Sparks, Kylie Whitelaw, John Ayres, Stephanie T Yerkovich, Dalia Khalil, Kerry M Atkinson, and Peter M A Hopkins. 2014. A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology (Carlton, Vic.), no. 7 (July 9). doi:10.1111/resp.12343. https://www.ncbi.nlm.nih.gov/pubmed/25039426
[5] ^ Barczyk, Marek, Matthias Schmidt, and Sabrina Mattoli. 2015. Stem Cell-Based Therapy in Idiopathic Pulmonary Fibrosis. Stem cell reviews and reports, no. 4. doi:10.1007/s12015-015-9587-7. https://www.ncbi.nlm.nih.gov/pubmed/25896401