Over the last 20 years, the term “stem cells” has become relatively popular on TV and the news and is often discussed extensively in the scientific community. Debates and heated discussions about the role of stem cells can be found everywhere; unfortunately, much of the reasoning is not based on science. Religious, political, or governmental policies about stem cell research often create more confusion about a subject that is usually quite misunderstood.
Introduction to Stem Cells
For most ordinary citizens, regenerative medicine and stem cells become confusing. The Cellular Regeneration Center would like to take this opportunity to discuss at length the what, where, when, and why of stem cells to better educate the public about the benefits and pitfalls of stem cell science and the relevance it can have on daily life, well-being, and ongoing health management.
History of Stem Cells
The phrase “stem cell” first appeared in the scientific literature around 1868, when a biologist from Germany, Ernst Haeckel, used it to describe the process of a fertilized egg becoming a living, breathing organism.
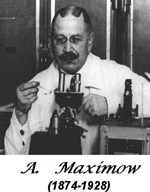 In 1908, Alexander A. Maximow, a Russian histologist, used the term to hypothesize the very existence of cells in our blood known as hematopoietic. In 1924, Dr. Maximow was the first to identify a single precursor cell within a type of tissue cluster known as mesenchyme. The mesenchyme cells were thought to differentiate into different types of blood cells. These cells were later revealed to be what is known today as mesenchymal stem cells.
In 1908, Alexander A. Maximow, a Russian histologist, used the term to hypothesize the very existence of cells in our blood known as hematopoietic. In 1924, Dr. Maximow was the first to identify a single precursor cell within a type of tissue cluster known as mesenchyme. The mesenchyme cells were thought to differentiate into different types of blood cells. These cells were later revealed to be what is known today as mesenchymal stem cells.
Who Discovered Stem Cells?
The first known bone marrow stem cell transplant was performed in 1959 by French oncologist Georges Mathé. The experimental procedure was performed on 5 Yugoslav nuclear plant workers whose marrows had been severely damaged in an accident. Dr. Mathé later pioneered stem cell therapy in bone marrow transplants to treat leukemia.
Bone marrow is the primary location in the human body that produces stem cells. Bone Marrow-derived stem cell therapy took off in the 1950s—1970s when Dr. E. Donnall Thomas at the Fred Hutchinson Cancer Research Center pioneered it. Dr. Thomas’ research proved that stem cells extracted from bone marrow could be infused intravenously to produce new blood cells.
The first use and research with stem cells in Thailand started around 1995 at the Faculty of Medicine at Siriraj Hospital, which is part of Mahidol University Medical School. The early pioneers of stem cell research in Thailand focused on understanding and treating thalassemia, a common type of blood disorder in Thailand.
What are Stem Cells?
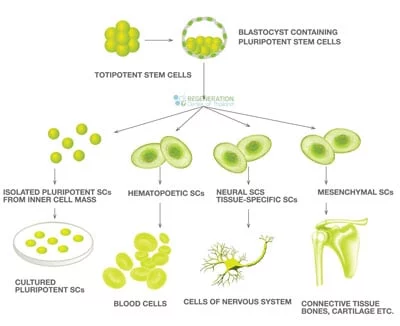
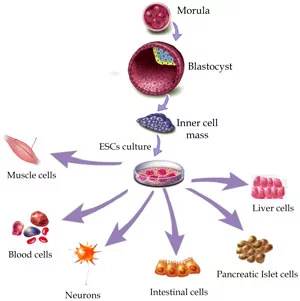
There are an estimated 100 trillion stem cells in the adult human body. A Stem cell is essentially a type of “seed,” “starter,” or “blank source” cell that has the unique ability to transform or differentiate into any adult human tissue.
Stem cells are often called “Adult Stem Cells,” but the colloquial term is slightly misleading. “Adult Stem Cells are found in infants, children, and adults. The opposite of Adult Stem cells is known as Embryonic stem cells. Adult stem cells are sometimes also called somatic stem cells.
Global Stem Cell Therapies (Since 2004)
Stem Cell Facts
These potent and “undifferentiated cells” are found in all multicellular organisms on earth and can replicate/copy themselves indefinitely into more healthy cells of the same type. This process is known as cell differentiation.
Stem cells are also sometimes referred to as progenitor cells because they can assume the role and function of another type of cell. The main difference between stem cells and progenitor cells is that they can only differentiate to form one or more kinds of cells, but they cannot divide and reproduce indefinitely as stem cells can.
cannot divide and reproduce indefinitely as stem cells can.
Two REQUIREMENTS for a Successful Stem Cell Treatment:
- The cells must possess the ability to self-renew. Self-renewal is described as the ability of a cell to go through multiple cycles of normal cell division while being able to maintain an undifferentiated state.
- The cells must be Potent: Potency is the ability to differentiate into three germ layers of endoderm ( endothelium cells,) mesoderm, or ectoderm.
What is Stem Cell Therapy?
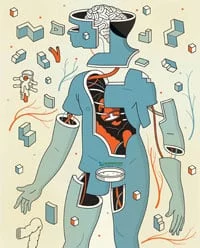
These potent “blank” cells are the foundation for every organ, cell, and tissue in the human body. They are essential because they are the only natural means to permanently repair or replace damaged tissues and organs. Through a targeted delivery protocol, the cells can reverse degenerative diseases or injuries. Recent research has also found that intermittent fasting triggers stem cell regeneration.
 Today, stem cell therapies and gene therapies are used to treat a variety of degenerative conditions, such as:
Today, stem cell therapies and gene therapies are used to treat a variety of degenerative conditions, such as:
- Blood Cancers
- Blood diseases – Thalassemia and Sickle cell anemia
- Diabetes – Pancreas & Diabetic Nephropathy
- Cardiovascular disease – Heart Attacks and “CHF” or Congestive Heart Failure
- Pulmonary Disease – COPD, Emphysema and Idiopathic Pulmonary Fibrosis
- Degenerative Neurological Disease – ALS, Motor Neuron Disease, Alzheimer’s and Parkinson’s
- Neurological and Spinal Injuries caused by Accidents or Strokes
- Sensory loss and peripheral neuropathy
- Autoimmune Diseases – Lupus
- Orthopedic Diseases or Injuries – Arthritis, Lower back injuries, Knee injuries, Degenerative Hips, Sports Injuries
Various types of motor nerves & somatic cells have been identified in the human body. They range from cells that can perform a single function to more specialized cells that form the foundation of human tissue or organs. [1]
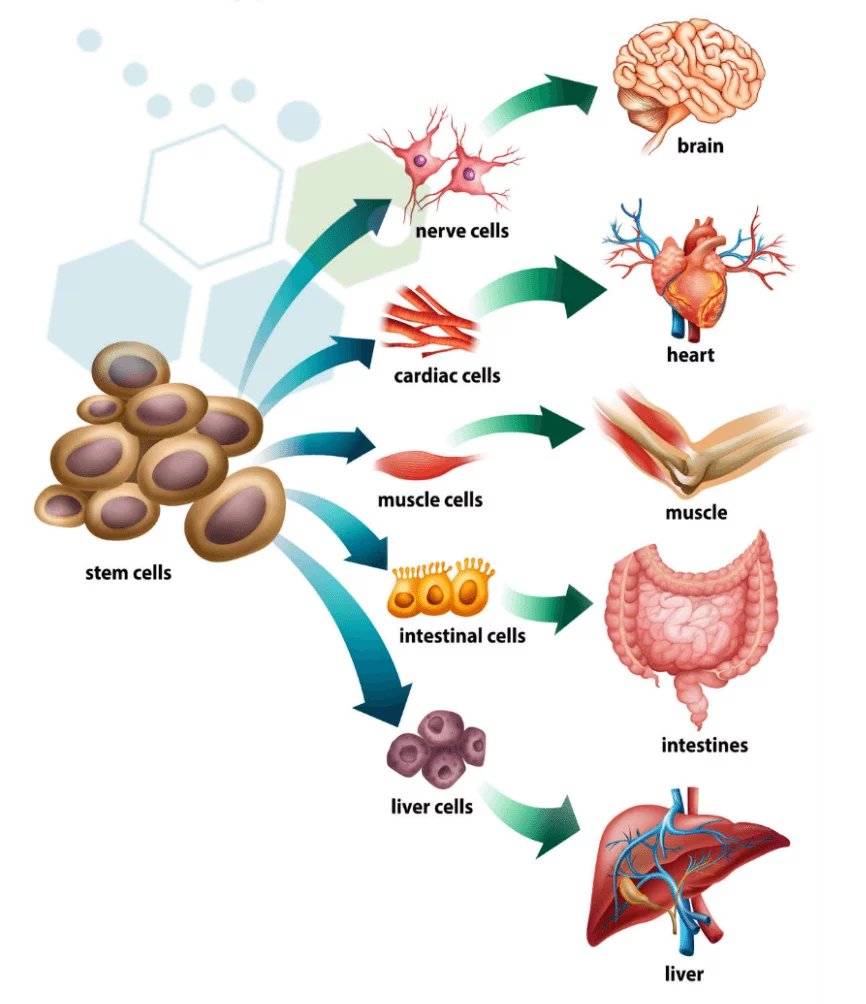
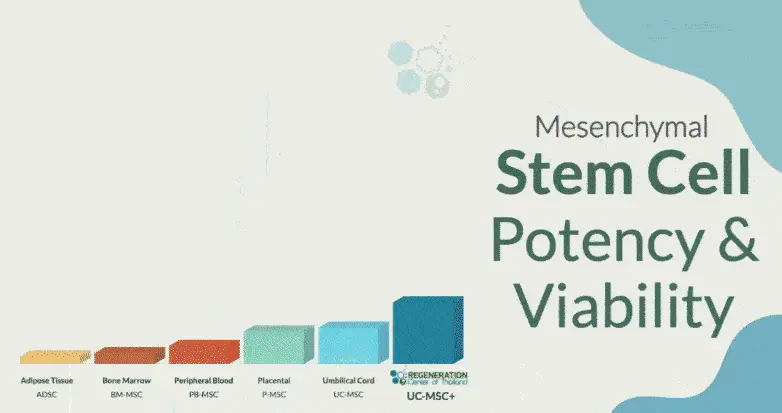
Mesenchymal stem cells, for example, are adult stem cells that can form cartilage, bone, tendon, ligaments, muscle cells, skin cells, and even nerve cells. In contrast, hematopoietic stem cell lines give rise to blood cells only (red cells, white cells, and platelets), while neural stem cells form only cells in the nervous system. are known for their ability to differentiate into multiple cell types, including osteoblasts (bone cells), chondrocytes (cartilage cells), adipocytes (fat cells), myocytes (muscle cells), and even neurons under specific conditions. MSCs have immunosuppressive properties, meaning they can modulate immune responses. This makes them valuable in treating autoimmune diseases and preventing graft-versus-host disease (GVHD) in transplantation. MSCs stem cells secrete a range of bioactive molecules, including cytokines and growth factors, that promote tissue repair and modulate the immune response. This secretome is thought to contribute significantly to their therapeutic effects. MSCs are relatively easy to isolate and expand in vitro, which is advantageous for therapeutic applications at the Regenereration Center.
Where are Stem Cells Found?
Two types of stem cells are used in research and therapies: autologous and Allogeneic cells. Autologous stem cells are from the patient’s body, while Allogeneic stem cells are donated from a person other than the recipient.
Autologous cells are found dispersed throughout our body and are typically named based on which particular phase of development or body part they are found in. The “birth” of a stem cell occurs in the bone marrow region, and they are then released into the bloodstream to allow proliferation through the entire body. Our blood circulation allows the transport of these cells throughout the body. After an injury or accident, the cells/tissue near the injury site releases a chemical known as cytokines, which act as a beacon of distress to help recruit new stem and progenitor cells to the area of damage in a migration process known as homing.
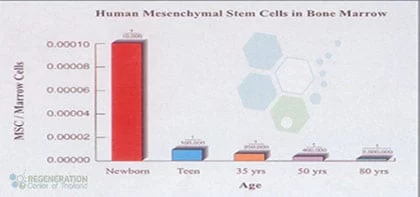
Natural reduction of Circulating Mesenchymal Cells in Humans as we age
Four Viable Sources of Autologous Stem Cells
- Human Bone Marrow – harvesting is very invasive and requires drilling into the femur bone or iliac crest
- Peripheral Blood – Blood stem cells are extracted from the patient through a process known as apheresis. Blood is drawn from the patient and filtered in a machine that extracts the patient’s stem cells and then returns a portion of the blood to the donor.
[2] - Dental Pulp – The dental pulp of young adolescents comprises soft living tissue. Scientists have found that dental pulp is a rich source of mesenchymal stem cells and does not require invasive extraction procedures.
- Adipose-derived or Fat stem cells – Acquired through mini-liposuction, Adipose stem cells are used primarily in cosmetic treatments such as stem cell facelifts or stem cell breast reconstruction after cancer.
For some applications and systemic autoimmune diseases, patients are not candidates for autologous stem cell therapy and require allogeneic-derived Stem cells. [3] These Allogeneic cells are not from the patient themselves and are primarily acquired from our stem cell bank with donated umbilical cord tissue, human placenta (Wharton’s jelly), or bone marrow of the patient’s immediate relatives. These cells are matched to the patient using HLA matching to minimize any risk of graft vs. host disease.
Stem Cell Scams & Warnings
In recent years, stem cell tourism has taken off in many parts of the world. The promise of functional regenerative medicine is being tarnished by ethically problematic and unproven therapies from untrustworthy sources. Many of these experimental treatments and therapies have never undergone proper clinical trials but are being marketed directly as therapies or, worse yet, “Cures.” These “same day” experimental stem cell therapies are not being carried out by licensed or professional medical staff and often do not comply with the framework of an approved treatment protocol that is used to ensure ethical standards and proper protocols are being met. Please use caution and correct judgment when contacting unscrupulous stem cell clinics globally who often over-promise but under-deliver. Other signs to watch out for are unlicensed doctors who promise treatments with “no risks” or treatments that offer no post-treatment care or assistance.
Some people may think/claim that stem cells are some “magic bullet” or “miracle cure” for everything.
This is NOT TRUE!
Cell-based therapeutic medicine is based on observable, evidential science and can help some patients but cannot help every person every time. The ability to treat degenerative or acquired diseases is still in the early stages of clinical application and is reserved for approved cases only. The only successful stem cell treatment with a proven/established regenerative medical procedure is hematopoietic stem cell transplantation.
Stem Cells in Asia
 Doctors and researchers in medical journals have been studying ways to make the clinical application of stem cells more consistent. In the lab, we have
Doctors and researchers in medical journals have been studying ways to make the clinical application of stem cells more consistent. In the lab, we have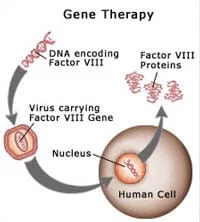 proven that stem cells can help repair or replace damaged tissue, organs, and cells in the body and can “grow” or differentiate into many types of cells. Outside the lab, the results are not as consistent.
proven that stem cells can help repair or replace damaged tissue, organs, and cells in the body and can “grow” or differentiate into many types of cells. Outside the lab, the results are not as consistent.
One of the most promising areas of regenerative medicine focuses on the ability to “reprogram” skin cells from any human and turn them into beneficial, pluripotent cells. This process and type of cells are induced pluripotent stem cells or iPS cells and were first discovered in 2006 by Dr. Shinya Yamanaka. The ability to reprogram adult/somatic cells into iPS cells has significantly affected stem cell biology and regenerative medical science.[4]
iPS cells are still in their infancy but have shown promising results in the laboratory environment, especially when combined with Gene Therapy. Human clinical trials of iPS cells are already on the way, but many obstacles still need to be resolved before we can take full advantage of iPS cells and iPS technology.
Advancements and breakthroughs are being achieved daily in hopes of taking these abundant cells and making them more clinically applicable.
To learn more, please contact us today.
Published Clinical Citations
[1] ^ Ungkanont, A, W Mongkonsritrakoon, S Jootar, and T Srichaikul. 2000. Allogeneic stem cell transplantation in a patient with refractory Burkitt’s lymphoma using non-myeloablative conditioning regimen. Bone marrow transplantation, no. 12. https://www.ncbi.nlm.nih.gov/pubmed/11223978
[2] ^ Panich, V, M Pornpatkul, and W Sriroongrueng. 1992. The problem of thalassemia in Thailand. The Southeast Asian journal of tropical medicine and public health. https://www.ncbi.nlm.nih.gov/pubmed/1298980
[3] ^ Velasco, Román Pérez, Usa Chaikledkaew, Chaw Yin Myint, Roongnapa Khampang, Sripen Tantivess, and Yot Teerawattananon. 2013. Advanced health biotechnologies in Thailand: redefining policy directions. Journal of translational medicine (January 2). doi:10.1186/1479-5876-11-1. https://www.ncbi.nlm.nih.gov/pubmed/23281771
[4] ^ Nielsen, B F. 1986. Haemorrhagic compression of the femoral nerve complicating anticoagulation therapy. Case report. Acta chirurgica Scandinavica. https://www.ncbi.nlm.nih.gov/pubmed/3564822