Crohn’s disease and ulcerative colitis (UC) are considered the two most common classifications of inflammatory bowel diseases (IBD). These autoimmune diseases, such as pancreatitis, Fibromyalgia, Type 1 diabetes, transverse myelitis, Idiopathic pulmonary fibrosis and SpA (Spondyloarthritides) disorders cause our cells to attack the healthy immune system affecting vital functions of the digestive tract.
IBD is a group of disorders that create prolonged Inflammation of our digestive tracts, including the: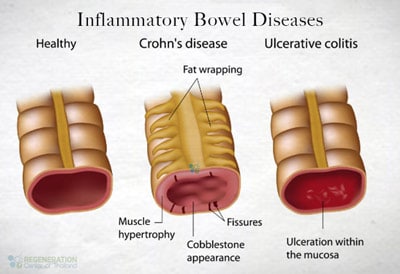
- Esophagus
- Stomach
- Mouth
- Small & large intestines
Ulcerative Colitis & Crohn’s Disease
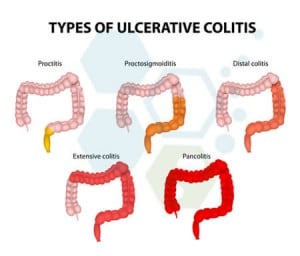 Our digestive tracts are designed to break down our foods to allow the natural extraction of nutrients while simultaneously removing all waste by-products. Prolonged Inflammation in our digestive tract severely disrupts this process, resulting in Diarrhea, Bleeding ulcers (hematochezia), severe pain, bloating, cramping, weight loss, multiple complications, higher risk of colon cancer, anemia, and, in some cases, death. If left untreated, the symptoms can spread to other parts of the body, resulting in joint pain, arthritis, eye inflammation, fevers, mouth sores, and skin disorders.
Our digestive tracts are designed to break down our foods to allow the natural extraction of nutrients while simultaneously removing all waste by-products. Prolonged Inflammation in our digestive tract severely disrupts this process, resulting in Diarrhea, Bleeding ulcers (hematochezia), severe pain, bloating, cramping, weight loss, multiple complications, higher risk of colon cancer, anemia, and, in some cases, death. If left untreated, the symptoms can spread to other parts of the body, resulting in joint pain, arthritis, eye inflammation, fevers, mouth sores, and skin disorders.
Possible complications associated with ulcerative colitis and Crohn’s include:[1]
- Fistulas ( ulcers in the bowel wall that create holes between and inside the digestive tract)
- Bowel obstruction
- Malnutrition
- Colon cancer
- Rectal Cancer
- Kidney Cancer
- Rupturing of the Intestines
- The shock from rapid blood loss during a sudden and extended amount of bloody diarrhea
Ulcerative Colitis & IBD Autoimmune Diseases?
The definitive causes and triggers of IBD are still in debate. Still, functional medical specialists believe that the IBD, Primary Sclerosing Cholangitis and SLE family has a specific genetic predisposition and can be directly linked
with over 165 particular genes in our bodies. Most doctors believe the culprit is a combination of environmental and hereditary conditions triggered by environmental factors, resulting in a sudden bacterial shift. These are examples of autoimmune diseases that can develop after an abnormal immune response. External factors like stress and dietary habits can significantly worsen the symptoms of IBD; however, they typically do not cause the disease.[2]
There are several tests available today that can quickly diagnose UC (ulcerative colitis) and Crohn’s disease. The most common method is a simple blood test to trace symptoms of Inflammation or anemia. Stool samples can also be used to find signs of infection in the digestive tract. Diagnosis can be confirmed using genetic testing and a sigmoidoscopy or colonoscopy test that uses long, thin tubes with lighted cameras to enter a patient’s intestine for visual inspection and to take tissue samples, i.e., “biopsy.” Other minimally invasive tests to verify intestinal issues include MRI Scans, CT (CAT) scans, Ultrasound Scans, or capsule endoscopies.
Treatments for Crohn’s Disease
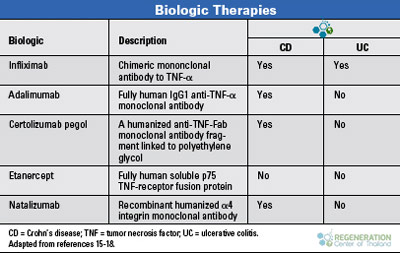
Traditional treatment for IBD typically requires a wide variety of pharmaceutical medications ranging from:
- Corticosteroids & Prednisone
- Biologic therapies
- Antibiotics
- Immunosuppressive medications
Patients with a chronic condition or a severe diagnosis may require surgery to remove the large intestine, resulting in a lifelong need for a colostomy bag, which is an eternal or internal plastic pouch for fecal and waste removal. A large number of Crohn’s disease patients often require strictureplasty surgery and or corrective surgery to repair fistulae and strictures to stop the bleeding in the intestines. A strict change in diet is also usually needed to promote proper cell signaling and help reduce stress and Inflammation. It is usually recommended that patients avoid eating greasy foods, processed meat products, spicy foods, cream sauces, or foods with high fiber.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Crohn’s Disease, Ulcerative Colitis, or other forms of Inflammatory Bowel Disease (IBD) with stem cells. Patients with severe intestinal damage, significant complications, or other critical health conditions might not be good candidates for treatment.Treating Ulcerative Colitis With Stem Cells
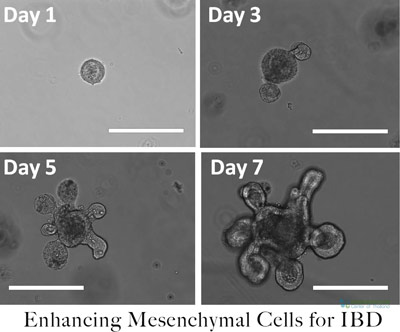 Our hospital for stem cells offers a safe, new, and permanent method of treating chronic inflammatory bowel diseases such as Crohn’s & ulcerative colitis. Stem cell therapy for Crohn’s helps to reset and repair the immune system using lab-enhanced/differentiated Hematopoietic mesenchymal stem cells that do not induce interferon-γ production, lymphocyte proliferation, or up-regulation of the activation markers. The infused UC-MSC+ cells help to improve the autoimmune disease by helping to promote a change in the production of pro-inflammatory cytokines to the beneficial anti-inflammatory cytokines at and near the site of injury. The Enhanced Mesenchymal cells are 100% histocompatible [3] to the recipient and safe, which helps to quickly restore red blood cell count and hemoglobin levels in most patients. The enriched cells act like a patch that covers any ulcer regions in the intestines, allowing them time to heal properly.[4]
Our hospital for stem cells offers a safe, new, and permanent method of treating chronic inflammatory bowel diseases such as Crohn’s & ulcerative colitis. Stem cell therapy for Crohn’s helps to reset and repair the immune system using lab-enhanced/differentiated Hematopoietic mesenchymal stem cells that do not induce interferon-γ production, lymphocyte proliferation, or up-regulation of the activation markers. The infused UC-MSC+ cells help to improve the autoimmune disease by helping to promote a change in the production of pro-inflammatory cytokines to the beneficial anti-inflammatory cytokines at and near the site of injury. The Enhanced Mesenchymal cells are 100% histocompatible [3] to the recipient and safe, which helps to quickly restore red blood cell count and hemoglobin levels in most patients. The enriched cells act like a patch that covers any ulcer regions in the intestines, allowing them time to heal properly.[4]
Transplantation of enhanced mesenchymal stem cells also helps to restore the patients’ natural immunocompetency while also stopping the degeneration of the autoimmune process from continuing. Patients of nonspecific ulcerative colitis will require a multi-stage approach over a period of two weeks at our outpatient stem cell clinic in Bangkok.
Benefits of Stem Cell Therapy for Crohn’s & IBD
Treat the source, not the symptoms. The regeneration center helps fight inflammatory bowel disorders such as Crohn’s disease on the cellular level using a safe and effective protocol that does not require general anesthesia or invasive surgery and can be used to successfully manage a wide variety of autoimmune diseases and inflammatory bowel diseases such as:
- Diversion colitis

- Behçet’s disease
- Collagenous colitis
- Indeterminate colitis
- Lymphocytic colitis
- Microscopic colitis
- Ischemic colitis
- Lymphocytic colitis [5]
- Digestive System Diseases
- Gastroenteritis
- Crohn’s Disease
- Intestinal Diseases
- Gastrointestinal Diseases
- Ulcerative Colitis
- Inflammatory Bowel Diseases
The treatment using stem cells offers tangible hope for patients looking to eliminate pain safely. However, please note that stem cells cannot treat a genetic disease; instead, they treat the condition on the cellular level.
The goals of using UC-MSC+ Cells for inflammatory bowel diseases are to:
- Relieve the pain and symptoms of Crohn’s disease
- Stop the development of the chronic autoimmune condition
- Decrease the system inflammation while treating the ulcers in the small and large intestines
- Restore the digestive system’s health and function
- Enhance the body-diverse microbiome
- Eliminate the bouts of rectal bleeding, abdominal cramps, constipation and diarrhea
- Restore the patients’ health and balance
UC-MSC+ Crohn’s Therapy Guidelines – 2025
Treatment Method: The number of Stem Cell Injections will vary based on patient needs. Multiple stages may be required for severe gastrointestinal (GI) tracts.
Types of Cell Infusion: Enhanced Mesenchymal Stem Cells ( UC-MSC+ Cells). The exact protocol for the patient will depend on various factors such as age and underlying condition. To qualify for treatment, a medical review will be required. Depending on the patient’s physical needs, the treatment cell infusions will be made via guided scanners (if/when necessary) or through a non-invasive and painless IV, “Intravenous Drips,” that will not require anesthesia or an overnight stay at a hospital. Direct injections or Sub Q injections may be required in some cases.
Cost of Treating UC & IBD With UC-MSC+ Stem Cells
The treatment for ulcerative colitis or Crohn’s will require 10-16 days in Bangkok. Due to the varying degrees of disease progression, our medical team will need to understand a potential patient’s needs better before a treatment prognosis can be provided. Upon completion of the evaluation, a detailed treatment plan shall be provided that will include all specifics relating to the patient’s needs, such as the exact number of nights required in Thailand and the total medical-related costs for the entire treatment. Please prepare your recent medical records and diagnostic test results and contact us today to begin your inquiry.
Rehab After Treatment: Physical rehabilitation for treatment is optional, depending on the patients’ travel/time constraints. Complete physical rehab programs can be provided for patients at a partner hospital for two to four hours per day and seven days per week. Medical visas for longer travel and extended stay apartments or hotel accommodations for the patient and family can also be requested.
Published Clinical Citations
[1] ^ Blanc, K Le, L Tammik, B Sundberg, S E Haynesworth, and O Ringdén. 2003. Mesenchymal stem cells inhibit and stimulate mixed lymphocyte cultures and mitogenic responses independently of the major histocompatibility complex. Scandinavian journal of immunology, no. 1. https://www.ncbi.nlm.nih.gov/pubmed/12542793
[2] ^ Ciccocioppo, Rachele, Alessandra Gallia, Adele Sgarella, Peter Kruzliak, Paolo G Gobbi, and Gino Roberto Corazza. 2015. Long-Term Follow-Up of Crohn’s Disease Fistulas After Local Injections of Bone Marrow-Derived Mesenchymal Stem Cells. Mayo Clinic Proceedings, no. 6. doi:10.1016/j.mayocp.2015.03.023. https://www.ncbi.nlm.nih.gov/pubmed/26046409
[3] ^ Martínez-Montiel, María Del Pilar, Gonzalo Jesús Gómez-Gómez, and Ana Isabel Flores. 2014. Therapy with stem cells in inflammatory bowel disease. World Journal of Gastroenterology, no. 5 ( 7). doi:10.3748/wjg.v20.i5.1211. https://www.ncbi.nlm.nih.gov/pubmed/24574796
[4] ^ Portilla, F de la, F Alba, D García-Olmo, J M Herrerías, F X González, and A Galindo. 2012. Expanded allogeneic adipose-derived stem cells (eASCs) for the treatment of complex perianal fistula in Crohn’s disease: results from a multicenter phase I/IIa clinical trial. International journal of colorectal disease, no. 3 (September 29). doi:10.1007/s00384-012-1581-9. https://www.ncbi.nlm.nih.gov/pubmed/23053677
[5] ^ Sánchez-Berná, Isabel, Carlos Santiago-Díaz, and Juan Jiménez-Alonso. 2014. [Immunomodulatory properties of stem mesenchymal cells in autoimmune diseases]. Medicina clinica, no. 2 (March 15). doi:10.1016/j.medcli.2014.01.014. https://www.ncbi.nlm.nih.gov/pubmed/24636281