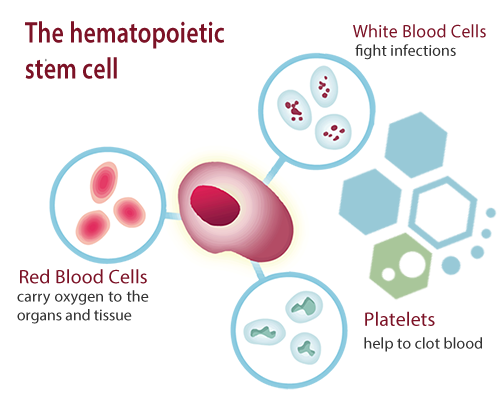
Peripheral blood stem cells (PBSCs) are hematopoietic stem cells (HSCs) that are found in the bloodstream. HSCs are a unique type of cell that can self-renew and differentiate into all kinds of blood cells, including platelets, red blood cells and white blood cells [1]. These hematopoietic blood-forming cells can be found in bone marrow (Bone marrow stem cells) or found in circulating (peripheral) blood. Bone marrow cells that released into the bloodstream under specific conditions and can be harvested for use in treatments via the process of stem cell mobilization.
The Importance of Peripheral Blood Stem Cells
PBSCs play a crucial role in our bodies, particularly in the immune system and regenerative medicine.
In the Immune System
Our immune system relies on a constant supply of blood cells to function correctly. Circulating PBSCs help maintain this supply by continuously producing blood cells, including white blood cells, essential for fighting infections and maintaining overall health. Without PBSCs, our immune system would get severely compromised fast.
In Regenerative Medicine
Peripheral blood mesenchymal stem cells (PBSCs) have shown immense potential in regenerative medicine due to their ability to differentiate into various blood cell types. They are often used in stem cell transplantation to treat multiple blood-related diseases and disorders.
How to harvest stem cells from peripheral blood
PBSC Collection Methods
The two main methods are used to collect PBSCs for transplantation: mobilization and apheresis.
- Peripheral Blood Stem Cell Mobilization is done by stimulating the bone marrow to release HSCs into the bloodstream. This is typically done using medications like granulocyte colony-stimulating factor (G-CSF) and, in some cases, chemotherapy. After several days of treatment, the number of HSCs in the bloodstream increases significantly, making the collection more accessible for use in therapies [2].
- Apheresis or Plasmapheresis is the actual collection process of PBSCs from the bloodstream. The donor’s blood is drawn through a needle and passed through a machine that separates the stem cells from other blood components. The remaining blood plasma is returned to the donor, and the collected stem cells are preserved for transplantation.
Peripheral Blood Stem Cells Transplants
Peripheral blood stem cell transplantation involves three main steps: conditioning, infusion, and engraftment.
 Conditioning
Conditioning
Conditioning the body before the cell transplant is done by a recipient who plans on having therapies. Conditioning in some cases of Multiple Sclerosis typically involves chemotherapy and/or radiation therapy to destroy the patient’s existing bone marrow and immune system, making room for the new immune stem cells to engraft and grow [3].
Stem Cell Infusions
After conditioning, the isolated and expanded PBSC stem cells can be infused into the recipient’s bloodstream via an IV drip or injected locally to sites in the body using guided injections. This process is similar to a blood transfusion and usually takes a few hours.
Stem Cell Engraftment
Engraftment is the critical stage where the transplanted PBSCs migrate to the recipient’s bone marrow and produce new blood and immune cells. This process can take time, during which a patient is closely monitored for complications or infections.
Comparing Peripheral Blood Stem Cells to Other Sources
Other sources of stem cells are used in transplantation, such as bone marrow and umbilical cord blood. Each source has its advantages and disadvantages.
Bone Marrow Stem Cells 
Bone marrow stem cells are the traditional source of HSCs used in transplantation, and they are collected directly from the donor’s bone marrow, usually from the hip bone. While bone marrow transplantation has successfully treated many conditions, it is a more invasive procedure than PBSC collection and may require general anaesthesia.
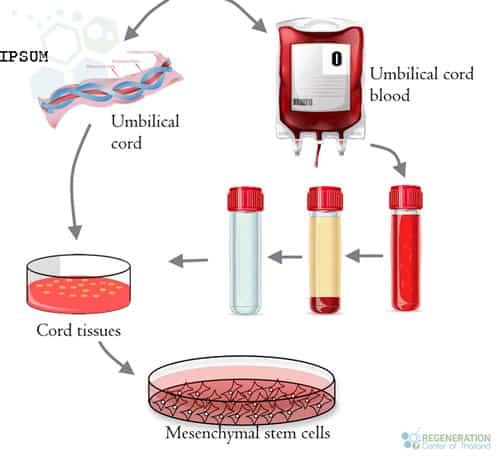
Umbilical Cord Blood Stem Cells
Umbilical cord blood is another rich source of HSCs; these types of cells are usually collected immediately after birth. Cord blood stem cells can be stored and used for future transplantation. Although cord blood has a lower risk of graft-versus-host disease (GVHD), it also has fewer stem cells than peripheral blood or bone marrow, leading to slower engraftment and an increased risk of complications [4].
Umbilical Cord Tissue Stem Cells
Cord tissue stem cells are a type of stem cell found in the umbilical cord tissue, specifically in Wharton’s jelly. This gelatinous substance surrounds the blood vessels within the umbilical cord. These stem cells have the capacity of self renewal and are classified as mesenchymal (MSCs) due to their unique regenerative properties.
Cord tissue stem cells can differentiate into various cell types, such as bone, cartilage, fat, and muscle cells. They also have immunomodulatory and anti-inflammatory properties, which make them an attractive candidate for research in regenerative medicine and potential treatments for various diseases and conditions, including autoimmune disorders, tissue injuries, and degenerative diseases.
Like bone marrow stem cells, cord tissue stem cells can be collected, stored, and used later in life for potential therapeutic purposes. The collection process is non-invasive and painless, as it takes place immediately after the birth of a baby, during which the umbilical cord is clamped, cut, and separated from the newborn. The cord tissue is then processed and stored cryogenically in our stem cell bank for future use.
Advantages and Disadvantages of PBSC
Compared to other sources, PBSCs have some distinct advantages. The collection is less invasive and generally has fewer side effects for the donor. Additionally, PBSC transplants typically results in faster engraftment, reducing the risk of complications. However, using allogeneic PBSCs may have a higher risk of GVHD, a post-transplant severe difficulty than adipose derived MSC cells or dental pulp stem cells.
Applications & Treatments Using Peripheral Blood Stem Cells
Peripheral blood stem cell transplantation has been used to treat various conditions, including blood disorders, autoimmune diseases, and cancer [5].
- Blood Disorders – PBSC transplantation can effectively treat various blood disorders, such as leukaemia, lymphoma, multiple myeloma, and aplastic anaemia. Transplanted stem cells can help regenerate the patient’s blood producing cells and immune system, improving their overall health.
- Autoimmune Diseases – In autoimmune diseases like systemic lupus erythematosus, spinal arthritis, connective tissue disease, type 1 diabetes, sjogren’s disease, rheumatoid arthritis and scleroderma, the patient’s immune system attacks healthy tissues. PBSC stem cells transplants act as immunomodulators to help reset the immune system and turning down some proteins while turning up others to manage the symptoms and improving quality of life.
- Cancer Treatments – High-dose chemotherapy and/or radiation therapy can destroy cancer cells for certain cancers in the liver, lung cancer, kidney cancers, colon cancer, mesothelioma, and pancreatic cancers. However, these chemotherapy comes with lost of side effects that can damage the bone marrow and immune system. PBSC stem cells can help regenerate the patient’s blood and immune system after these aggressive treatments. Learn how cancers are identified.
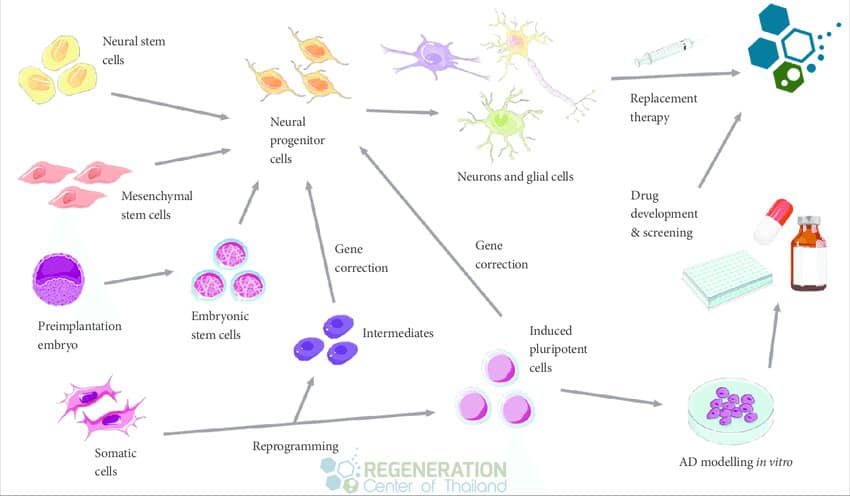
Future Directions, Applications and Challenges
As research continues, the potential applications of PBSC transplantation are expected to expand. However, there are still challenges and ethical considerations to address. Current stem cell research focuses on improving transplantation outcomes, reducing complications, and finding new applications for many types of stem cells including from Peripheral Blood. Innovations in gene editing, immunotherapies, NK Cell treatment and stem cell therapies for T2D will lead to more targeted and personalized treatments using the power of hematopoietic peripheral blood stem cells.
Ethical Considerations
As with any medical procedure, PBSC stem cells have raised ethical questions, such as donor consent, exploitation of vulnerable populations, and accessibility to treatment. These concerns are valid and always addressed at the Regeneration Center to ensure the ethical use of peripheral blood stem cells in functional health protocols.
The cost and accessibility of PB Stem cells can be significant barriers for many patients. Depending on scale and severity stem cell treatments can be expensive, and not all insurance plans may cover it. Finding a suitable donor can also be challenging, especially for some patients especially for this with unique bloodtypes or those from underrepresented ethnic backgrounds. Efforts to increase donor registries and promote diversity in stem cell donations around the world are vital to improving accessibility and providing life-saving treatments to more patients.
Peripheral blood stem cells have proven to be a valuable resource in treating various medical conditions, from blood disorders to autoimmune diseases and cancers. While there are challenges and ethical concerns to address, the potential applications of autologous peripheral stem cells will continue to expand, offering hope for improved treatment protocols with better patient outcomes.
Published Clinical Citations
[1] ^Hongeng S, Benjaponpitak S, Tardtong P, Varavithya W, Chuansumrit A, Chunharas A, Chaisiripoomkere W, Hathira P. Successful allogeneic peripheral blood stem cell transplantation in Wiskott-Aldrich Syndrome Patients: first report in Thailand. Asian Pac J Allergy Immunol. 2001 Sep;19(3):191-5. PMID: 11826914.
[2] ^Zhang Y, Huang B. Peripheral blood stem cells: phenotypic diversity and potential clinical applications. Stem Cell Rev Rep. 2012 Sep;8(3):917-25. doi: 10.1007/s12015-012-9361-z. PMID: 22451417.
[3] ^Ungkanont A, Jootar S, Ratanatharathorn V, Chiernsilp A. High dose chemotherapy and peripheral blood stem cell transplantation for high risk primary breast cancer: a single center experience in Thailand. Asian Pac J Allergy Immunol. 2000 Dec;18(4):215-20. PMID: 11316042.
[4] ^Tian M, Li X, Liu F, Xu D, Sun L, Li Q, Ling Y, Bai Y, Wu X, Liu Y, Qiao J. Efficacy of peripheral arterial access for peripheral blood stem cells collection. J Clin Apher. 2021 Dec;36(6):864-869. doi: 10.1002/jca.21940. Epub 2021 Sep 24. PMID: 34558738.
[5] ^Yuan S, Wang S. How do we mobilize and collect autologous peripheral blood stem cells? Transfusion. 2017 Jan;57(1):13-23. doi: 10.1111/trf.13868. Epub 2016 Oct 12. PMID: 27731496.


 Conditioning
Conditioning