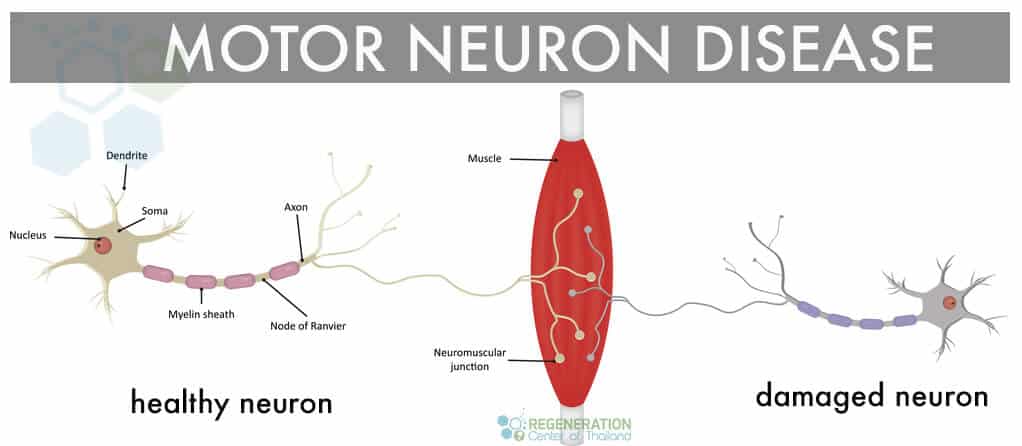
If a person’s motor neurons are not functioning well, they will experience significant problems with his or her movements, such as walking, standing up, turning, breathing, eating, speaking, and swallowing. The paracrine cell communication system is responsible for carrying out signals from your brain to your muscles. People can perform movements through a complex process involving neurons.
What is motor neurone disease?
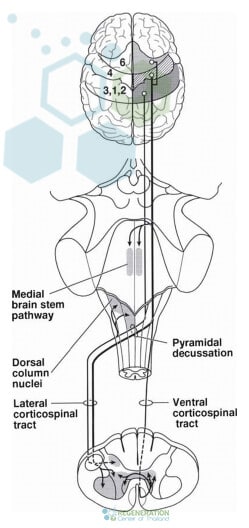
Motor neurons are mostly just nerve cells that are responsible for managing muscles in the body to move. Motor Neuron Disease or “MND” is a rapidly progressive neurological disease which damages motor neurons that are essential for us being able to control our movement. Nerve cells from the brain transmit messages to the nerve cells in the spinal cord, which are then distributed to different muscles in the body.
Types of MND
MND disorders are a family of conditions, and there are several classifications of motor neuron diseases depending on the patient symptoms and underlying causes, including:
- Amyotrophic lateral sclerosis (ALS) – ALS is the most well-known type of neurological disorder in the MND family. Famous cases of people with MND include Stephen Hawking, David Niven and Lou Gehrig who had Bulbar ALS. This is a very rare disease that affects the muscles of the legs, arms, respiratory system, and mouth. Incidence rates for ALS are higher in men and women ages 50 and up.
- Progressive muscular atrophy (PMA) is also a slow-moving variation of ALS and causes progressive muscle wasting in the legs, arms and mouth area
- Primary lateral sclerosis (PLS) is another form of upper & lower motor neuron disease that is not usually fatal but advances slightly slowly than ALS. PLS in children is known as juvenile primary lateral sclerosis
- Spinal muscular atrophy (SMA) is a genetic variant of MND that primarily affects children. There are three types of this disease and is caused by a mutation in the SMA1 gene and affects the legs and arms areas
- Progressive Bulbar Palsy (PBP) is a type of MND that affects the brain stem region. Patients diagnosed with ALS can also have progressive bulbar palsy (bulbar als,) and PBP symptoms include frequent choking, difficulty eating, speaking or swallowing
Signs & Symptoms of Motor Neuron Disease
Early symptoms of MND often affect specific areas in the body before it eventually spreads to other areas. Early diagnosis is critical to manage this condition and improve overall survival so essential to visit a neurologist after any early symptoms. There are typically three stages of MND including early, middle, and advanced (terminal MND)
Early stage symptoms of MND are often confused with other types of unrelated neurological disorders, and frequently, the diagnosis is changed after further testing. The initial signs and warning signals of MND depend upon where the disease manifests first. Typical symptoms for patients with onset MND are in the mouth ( bulbar) region, arms, legs, or lungs (respiratory system.)
Symptoms of Stage 1 MND include: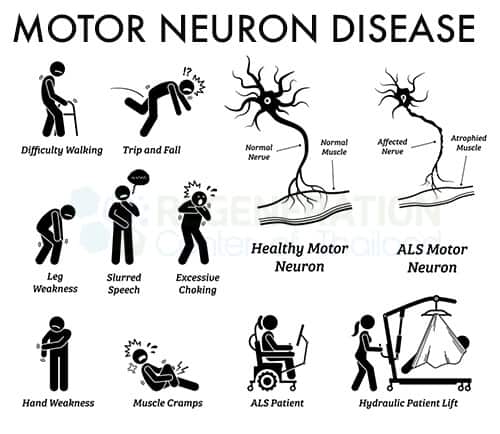
- Limb-onset disease resulting cramps, muscle pains and twitching
- Weakening hand grip or premature fatigue
- Weakness in the legs & arms
- Bulbar-onset disease resulting in garbled or slurred speech
- Difficulty with swallowing
- Increased incidents of clumsiness or stumbling
- Respiratory-onset disease which causes frequent shortness of breath
- Lack of oxygen causing poor sleep or waking up with a headache
As MND gets more advanced, the symptoms get more noticeable after several functions in the body are affected.
Symptoms of MND Stage 2 include:
- Progressively weaker limbs progressive muscular atrophy
- Increase in muscle related pain spasms and twinges
- Increase in Joint pain in the hips, knees or shoulders
- Muscle atrophy causing limb muscles to shrink or be abnormally stiff
- Reduction in rotation movements
- Inability to control saliva resulting in Drooling
- Frequent and uncontrollable bouts of yawning that can result in jaw pain
- Worsening of speech as muscles in the throat area and mouth become weak
- Frequent changes in emotional state or personality resulting in uncontrollable laughing or crying
- Reduction in brain function and memory
Some secondary symptoms of advancing MND can include depression, persistent anxiety, and insomnia.
Symptoms of Advanced Stage MND (End-stage) – As the neurodegenerative effect worsen eventually, the patients are unable to eat, move, or breathe without assistance. At this stage, options are minimal, and stem cell therapy is likely not an option once the attacks have researched a phase of increasing body paralysis where patients cannot function without supportive care. Respiratory failure is typically the most common complications of MND that leads to patient death while others become unconscious or fall into a deep sleep from which they can pass peacefully.
 Cause & Pathophysiology of MND
Cause & Pathophysiology of MND
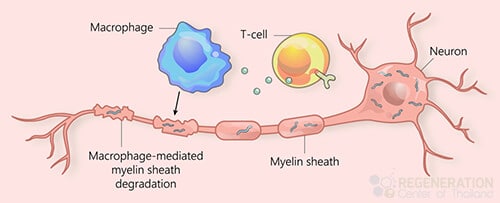
MND is diagnosed when the motor neurons (nerve cells) in the spine and brain lose their function. Although a lot of research has been the underlying cause of MND is still unknown bit is generally attributed to environmental (sporadic) factors or familial (hereditary/genetic) causes or a combination of the 2. In 90% of cases with MND, the patient does not have a family history; however, genetic testing was not prevalent in previous generations, so this hypothesis is likely to be changed. Most researchers studying MND believe that the cause of neural dysfunction and premature neuronal death is probably a combination of damaging environmental and genetic factors. As humans gradually age, we lose the ability to repair the damage resulting in irreversible neurodegeneration. Research on MND, Strokes, Mixed Non-Fluent Aphasia and Parkinson’s Disease are continuing, and it involves attacking the immune and genetic factors, toxins, viruses, nerve growth factors that affect the activity of motor neurons. Other factors that are somewhat related to the development of MND include an autoimmune pathogenesis, exposure to toxins via smoking, repeated head injuries as is with professional athletes in professional fighting, mixed martial arts, or the NFL. Residents of countries such as Japan, Guam, and New Guinea also have a much higher percentage chance of exposure to chemicals and radiation possibly due to current/previous military-industrial related activities.
Sporadic MND
Some causes for environmental/sporadic MND include:
- RNA processing & Aggregates of Proteins – Abnormal clumps of protein are known as aggregates. These dysfunctional clumps are found in all cases of MND and develop inside the neurons and disrupt the normal workings of the motor neurons. The most likely aggregate is the marker TDP-43, which is a vital protein responsible for processing RNA instructions inside the cell. These genetic instructions are essential in replicating/repairing cells and if damaged due to the protein clumping the nerve cell will be unable to function properly
- Mitochondria Dysfunction – The mitochondria provide energy for the cells allowing them to work normally. Patients with MND show damage to this system due to the accumulation of proteins inside the mitochondria, causing them to be unable to regulate energy production inside the cells.

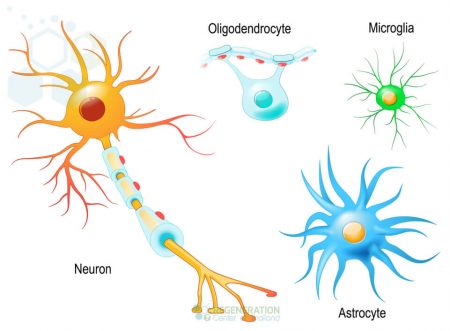
- Damage to Glial cells – Glial cells are the most common cell types in the central nervous system and provide support for neurons and help relay information between cells, provide nutrients and insulation between other supporting motor neuron cells.
- Cell Transport disruption occurs when cells are unable to dispose of toxic waste within the cells. The toxic waste within neurons is removed by antioxidants using containers of waste known as microvesicles. If this waste transportation system becomes disturbed, it can result in a buildup of toxic waste, causing abnormal cell activity. Some research has found links between MND and deficiencies in antioxidants. It is also not enough evidence to suggest that diet alone can be used to treat deficits in antioxidants.
- Glutamate Toxicity – Nerve cells use chemical messengers known as “Neurotransmitters” to send information between cells. There is evidence that for some patients an overproduction or hypersensitivity to glutamate occurs which causes over-excitation of the nerve cells resulting in apoptosis (cell death)
Environmental vs. Familial MND
It’s important to note that the symptoms for familial and sporadic MND are nearly identical and can only be differentiated on the genetic level. The causes of motor neuron disease and Multiple Sclerosis are still unknown. Various environmental factors have been identified to lead to neurodegenerative disease possibly and can include exposure to environmental toxins, heavy metals like lead, pesticides, DDT, dieldrin, chemical exposure, serum uric acid, toxaphene, and organochlorines.
Evidence is still inconclusive, but some other linked environmental factors for MND include:
- Severe traumatic brain injuries often misdiagnosed as ataxia or chronic traumatic encephalopathy (CTE)
- Repeat head injuries due to sports like MMA, Muay Thai boxing, and other contact sports
- Physical trauma due to accident
- Long term exposure to Electromagnetic fields
- Other triggers include cancers and environmental contaminants.
Genetic Screening for MND
Mutations in a human gene happen when the set of instructions (inside the cells) get damaged in some way. This results in the same error being replicated in new cells, which causes dysfunctions like MND. Familial MND is rare but can only be verified using proactively testing for mutated genes. The fact that MND can be passed on genetically suggests that single mutations inherited from the parents may sometimes have a play a much more significant role in developing the condition later on in life. Clinical diagnosis for Hereditary MND necessitates mutations in at least 2 (or more) genes due to oligogenic inheritance.
The Regeneration center does not offer gene therapies for MND but does provide DNA mutation test for MND with confirmed diagnosis to determine if they have one or more mutated genes associated with heredity MND. We offer DNA gene sequencing tests for over 40 variants linked to MND,hereditary motor neuropathy (HMN), neuronal ceroid lipofuscinoses (NCL) disorders and genetic prion disease including: C9ORF72, ALS2, TBK1, SOD1, PRNP, DCTN1, SPG11, HEXB, TARDBP, KIF5A, FUS, OPTN, PFN1, SETX, CHCHD10, CHMP2B, MATR3, UBQLN2, VAPB, TFG, VCP,BCKDHA, BCKDHB, DBT, PPM1K, SIGMAR1, ATP7B and SQSTM1.
Tests & Diagnosis for MND
It can often be challenging to diagnose MND in the early stages because of the symptoms if MND is often similar to other neurological conditions like Parkinson’s disease & multiple sclerosis (MS). 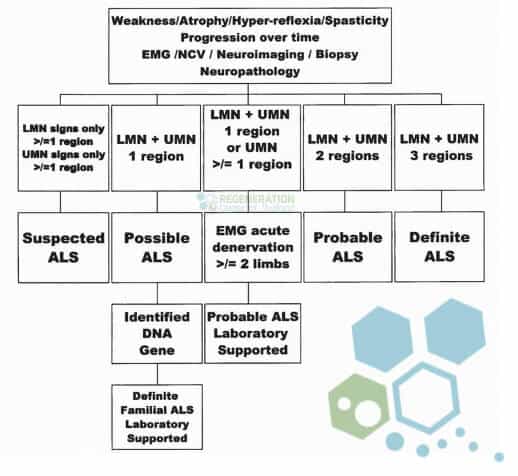 For most patients, a general physician will recommend that a neurologist review the patient symptoms and request any additional diagnostic tests to confirm a diagnosis. A neurologist starts with a review of the patients’ complete health history and physical symptoms of the neurologic disorder.
For most patients, a general physician will recommend that a neurologist review the patient symptoms and request any additional diagnostic tests to confirm a diagnosis. A neurologist starts with a review of the patients’ complete health history and physical symptoms of the neurologic disorder.
Tests that are used to confirm MND include:
- Blood and urine tests can be used to detect an increase in creatinine kinase (CK.) CK is an enzyme that is released with muscles break down and can be found in the brain, heart (especially after heart attacks,) skeletal system, and other tissues his is produced when muscle breaks down. Increase in the levels of creatinine kinase can be found in the blood tests of patients with neuronal diseases
- Radiology using MRI or CT scan might not be able to detect the actual presence of MND but is used in the diagnostic phase to eliminate other conditions that display similar symptoms, such as brain strokes, traumatic brain injury or cancerous brain tumors
- Nerve conduction test (NCT or NCS) along with Electromyography (EMG) tests are used to measure rates of electrical activity within muscles and to measure the actual speed of cell signals through the tissues.
- Lumbar Puncture aka “Spinal tap” is a medical procedure used to extract and evaluate cerebrospinal fluid (CSF.) CSF fluid surrounds and protects the brain, and spinal cord from trauma removes waste from cerebral metabolism and provides nutrients to the brain and nervous system
- Muscle biopsies can also be used as a diagnostic tool to test muscle tissue. A tiny piece of muscle tissue is surgically removed, then examined through a microscope. A biopsy can help identify issues in the connective tissue, vascular system, nervous system, and musculoskeletal system
- Genetic Tests are also used to screen for potential mutations found in patients with MND.
After the test is completed, a doctor can use inclusion criteria about the patient’s symptoms to determine if the patient has ALS. The most commonly used set of criteria doctors use to diagnose MND/ALS is the El Escorial criteria. [1]
The typical symptoms of upper motor neuron disease include frequent cramps, recent weight loss, the difficulty of swallowing, random muscle twitching, excessive muscle wasting or weakness, fatigue, slurred speech, and drastic emotional changes. Motor neuron disease cannot be reversed. The patient and his/her family have to make major adjustments to help cope with this disease. The average life expectancy of someone who is diagnosed with ALS or MND without any type of interventional treatment is 1 to 5 years. There are different types of MND, and many of them can be fatal if left untreated. Patients with neuronal disease can go through a plateau phase where symptoms remain stable for some time, but the condition will eventually worsen. Primary Lateral Sclerosis is a type of MND that is less fatal and progresses gradually. As the disease progresses, people with MND will develop generalized paralysis, the difficulty of swallowing, loss of speech, and full dependence to other people in performing day to day activity. People who care for MND patients should also adjust to the deteriorating condition of the patient.[2]
Stopping Progressive MND
Please note treatments for Motor Neuron Disease are much more effective in the earlier stages of the disease. New clinical trials and recent advances in neuro stem cell medicine using exosomes to bypass the blood-brain barrier has shown considerable promise in helping manage the progressive muscular atrophy much more effectively increasing both life expectancy and quality of life for patients with mild to moderate stage MND. [3]
Any success relies on proper and consistent management in relieving symptoms. Muscle relaxants and prescribed Pain relievers such as morphine are not a long term solution and only mask the underlying brain degeneration. Stem cell treatment for motor neuron disease focuses on the underlying issues leading to rapid muscle atrophy and nerve cell death using isolated and expanded neural stem cells along with progenitor cells and neurotrophic growth factors that lead help to secrete growth factors that lead to neurogenesis and the production of three types of nerve cells including oligodendrocytes, astrocytes, and neuron cells. Motor neuron replacement can be isolated in the ventral horn, bran and innervate striated muscle induce the proliferation for new cells to try to restore proper function. [4]
Motor Neuron Disease Treatment (MSC+)
Mesenchymal Stem cells are un-specialized cells in your body that can change into any tissue or cell (neuro) in the human body. Stem cells are especially unique as they can reproduce and divide indefinitely. The motor neuron disease treatment with stem cells is non-surgical and minimally invasive. We offer several Stem cells treatment protocols for many diseases and disorders, including:
- Motor Neuron Disorder
- Alzheimer’s
- ALS
- Cerebral Palsy
- Brain Injuries
- Spinal Injuries
- Treatment for Spinal Muscular Atrophy
- Autism
- Ataxia
- Idiopathic Pulmonary Fibrosis
- COPD
- Multiple Sclerosis
- and Kidney Disease
After Stem Cell Therapy for MND
To qualify for the treatment of nerve damage, upper motor neuron disease or lower motor neuron disease patients will be required to have an existing clinical diagnosis with tests to support the findings. A clinical diagnosis may take several months and include laboratory tests, such as MRI’s, Brain CT Scans, electromyography, nerve conduction tests, transcranial magnetic stimulation test (TMS), spinal taps, muscle biopsies, blood tests, and urinalysis. The Regeneration Center of Thailand offers functional medical treatments that focus primarily on repairing damaged or diseased tissues and replacement of the neural capacity through neural cells replacement therapy brought about by the rapidly degenerative disease. [5]
TREATMENT PRECAUTIONS & RISKS
Please Note that not all patients qualify for treatment of degenerative neurological conditions such as motor neuron disease. Patients with late stage, severe underlying conditions or travel restrictions may not qualify for the 2-3 week treatment protocol in BangkokNeural Cells for MND Overview
 The actual protocol used will depend on the patients’ needs and current physical condition. The total stay required for treatment in our Bangkok facility ranges from 2 – 4 weeks, depending on the severity and protocol needed. The total number of neural cell infusions also vary based on the scale and severity of the patient’s condition. Regeneration Center motor neuron protocol uses enhanced neural progenitor cells, somatic, and neuroprotective molecules. All treatment injections are administered via a combination of IV, Intrathecal, Nasal Nebulizer, or lumbar punctures as needed. Learn how to boost neural stem cells naturally.
The actual protocol used will depend on the patients’ needs and current physical condition. The total stay required for treatment in our Bangkok facility ranges from 2 – 4 weeks, depending on the severity and protocol needed. The total number of neural cell infusions also vary based on the scale and severity of the patient’s condition. Regeneration Center motor neuron protocol uses enhanced neural progenitor cells, somatic, and neuroprotective molecules. All treatment injections are administered via a combination of IV, Intrathecal, Nasal Nebulizer, or lumbar punctures as needed. Learn how to boost neural stem cells naturally.
Rehabilitation for “MND” Motor Neuron Disease: Rehabilitation therapy will be required after the treatment. Physical Rehabilitation can take place after MND treatment in Thailand or any country in the world able to offer physical and speech rehabilitation services. Post-Treatment rehab facilities options will be provided upon requests. Medical visas and accommodations for an extended stay can also be included as necessary.
2024 Guidelines for Treating MND
Due to varying degrees of severity, the total and exact cost for our stem cell therapy for motor neuron disease using neural stem cells will depend entirely on the patient’s actual medical needs. Our neurological stem cell team will need to better understand the patients’ needs before being able to offer a detailed treatment plan. Our neural regeneration protocol requires an initial medical review that can be done online or in person. To decide and provide an accurate and detailed treatment plan, our medical review team will require the patients’ recent medical records, including any diagnostic exams such as Brain MRI’s or CT Scans. (Test Results less than three months Old are needed to make a diagnosis)
To begin the pre-qualification process for our multi-stage MND treatment, please contact us today.
Published Clinical Citations
[1] ^ Agosta, Federica, Ammar Al-Chalabi, Massimo Filippi, Orla Hardiman, Ryuji Kaji, Vincent Meininger, Imaharu Nakano, et al. 2014. The El Escorial criteria: strengths and weaknesses. Amyotrophic lateral sclerosis & frontotemporal degeneration, no. 1-2 (December 8). doi:10.3109/21678421.2014.964258. https://www.ncbi.nlm.nih.gov/pubmed/25482030
[2] ^ Naujock, Maximilian, Nancy Stanslowsky, Peter Reinhardt, Jared Sterneckert, Alexandra Haase, Ulrich Martin, Kwang-Soo Kim, Reinhard Dengler, Florian Wegner, and Susanne Petri. 2014. Molecular and functional analyses of motor neurons generated from human cord-blood-derived induced pluripotent stem cells. Stem cells and development, no. 24 ( 15). doi:10.1089/scd.2014.0180. https://www.ncbi.nlm.nih.gov/pubmed/25007389
[3] ^ Phanthumchinda, K, O Supcharoen, and E Mitrabukdi. 1996. Madras pattern of motor neuron disease: case report from Thailand. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 6. https://www.ncbi.nlm.nih.gov/pubmed/8855616
[4] ^ Sarlak, Golmaryam, Anorut Jenwitheesuk, Banthit Chetsawang, and Piyarat Govitrapong. 2013. Effects of melatonin on nervous system aging: neurogenesis and neurodegeneration. Journal of pharmacological sciences, no. 1 (August 27). https://www.ncbi.nlm.nih.gov/pubmed/23985544
[5] ^ Terashima, Tomoya, Hideto Kojima, Hiroshi Urabe, Isamu Yamakawa, Nobuhiro Ogawa, Hiromichi Kawai, Lawrence Chan, and Hiroshi Maegawa. 2014. Stem cell factor-activated bone marrow ameliorates amyotrophic lateral sclerosis by promoting protective microglial migration. Journal of neuroscience research, no. 7. https://www.ncbi.nlm.nih.gov/pubmed/24936617

 Cause & Pathophysiology of MND
Cause & Pathophysiology of MND
