Cardiovascular disease, cardiometabolic syndromes, and coronary artery disease are the primary causes of morbidity and mortality worldwide. It is estimated that the annual number of human deaths related to cardiovascular disease is over 17.5 million worldwide, of which 80% of these deaths are due to strokes and heart attacks, and over 75% of these incidents occur in developing nations. A recent project by the World Health Organization monitored coronary heart disease across 37 ethnic populations in over 20 countries from all four continents. The study lasted over ten years and clearly shows that the annual heart-related/coronary events rate is 600/100,000 people. The most common issue was ventricular dysfunction, followed by myocardial infarction. A diagnosis of MI means that a patient’s heart muscle rapidly loses its blood supply. Without immediate treatment of the blockage, the event will lead to permanent damage in the affected areas of the heart. Ischemic heart disease is also referred to as coronary thrombosis, which occurs due to the formation of a blood clot inside the blood vessels of the heart.[1]
What Causes Heart Attacks?
The most common causes of MI (Myocardial Infarction) and congestive heart failure are thrombosis or blood clots. These clots usually come from inside one of the branches of the coronary artery. The clot restricts vital blood flow to the heart. This type of blood clotting doesn’t usually appear in healthy arteries unless there are existing atheromas within the arterial lining. Atheromas or plaque 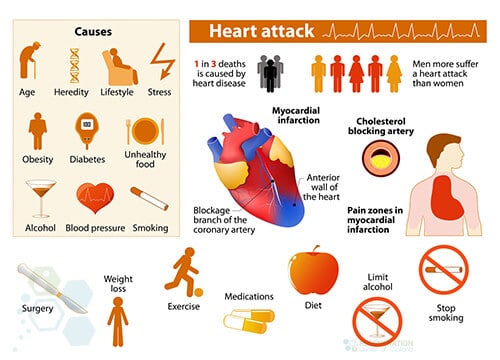 are fatty patches that develop in the linings of blood arteries. These plaque formations usually form over several years and manifest in more than one place inside the coronary arteries. Each Atheromas consists of an outer shell and soft inner core.[2]
are fatty patches that develop in the linings of blood arteries. These plaque formations usually form over several years and manifest in more than one place inside the coronary arteries. Each Atheromas consists of an outer shell and soft inner core.[2]
If a crack develops on the outer atheroma plaque shell, the event is known as a plaque rupture. This rupture exposes the inner core to circulating blood, which triggers the blood clotting mechanism, resulting in a blood clot. A buildup of plaque is usually the underlying issue that leads to the death of heart muscle cells and a heart attack. It’s worth noting that atheromas can develop in any part of the coronary arteries. If caught early enough, anti-clogging medications can safely break up the blood clot and eliminate the blockage before it is too late.
Other causes of blocked arteries and heart attack causes include:
- Chronic inflammation of the coronary arteries
- Complications from open heart surgeries
- Reduce infarct size & reduction in scarring of heart muscles caused by cardiogenic shock
- A clot forming elsewhere then travels to the coronary artery and causes blockage
- Drug abuse can also cause a coronary artery to go into spasm
- Failed surgeries leading to the death of cardiac muscle
Heart Attack vs. Cardiac Arrest: Understanding the Differences
While many people use the terms “heart attack” and “cardiac arrest” interchangeably, they are distinctly different cardiac events with unique characteristics, causes, and treatment approaches. A heart attack, medically known as myocardial infarction, occurs when blood flow to a part of the heart muscle is blocked, typically by a blood clot. This blockage prevents oxygen-rich blood from reaching that section of the heart, causing tissue damage or death in the affected area. Think of it as a “circulation” problem – like a clogged pipe in your heart’s plumbing system. During a heart attack, the heart usually continues beating, and the person typically remains conscious but experiences symptoms such as chest pain, shortness of breath, cold sweats, and pain radiating to the arms, neck, or jaw.
In contrast, cardiac arrest is an “electrical” problem where the heart suddenly stops beating altogether due to a malfunction in its electrical system. This causes an immediate cessation of blood flow throughout the body, leading to loss of consciousness and pulse within seconds. Without immediate intervention, cardiac arrest can result in death within minutes. While a heart attack can sometimes trigger cardiac arrest, they are separate conditions requiring different emergency responses. Heart attack victims usually remain conscious and require immediate transportation to a hospital for treatments like clot-busting medications or angioplasty. Cardiac arrest victims, however, need immediate CPR and defibrillation to restart the heart’s electrical system.
Survival rates and outcomes also differ significantly. Heart attacks, when treated promptly, often have better survival rates and recovery possibilities. In contrast, cardiac arrest has a lower survival rate due to the complete stoppage of heart function and the critical importance of immediate intervention. Understanding these differences is crucial for medical professionals and the general public, as recognizing the specific emergency can lead to more appropriate and timely responses, potentially saving lives.
Symptoms of a Pending Heart Attack – Heart MI

Cardiac Cell in a Dish
The body displays several warnings leading up to a heart attack. The most common symptom is severe chest pain, but pain can also travel to the jaw area, along with the right or left arm (or both). Patients also report heavy sweating and feeling faint or sick. The pain experienced by patients is very similar to angina, but it’s usually much more severe and persists for longer. While angina usually disappears after a few minutes, pain from a heart attack lasts anywhere from 10 minutes to several hours. Heart attack symptoms such as chest pain should be taken seriously and not ignored.[3]
A small/minor heart attack can occur with or without pain (relatively mild), leading the victim to think it’s just a lack of oxygen or heartburn. Significant or severe cardiac events can cause instant collapse, brain strokes, peripheral neuropathy, and result in sudden death. Many people recover without further complications if addressed early after the initial incident.
For some patients, an emergency angioplasty is required as an alternative to a ‘clot-busting’ medication. An angioplasty procedure uses tiny wires with a balloon attached to the end. The wire is guided into the large artery in the patient’s arm or groin area. The wire then travels up to the heart and directly into any blocked coronary artery using the assistance of radio guidance. When it reaches the area of blockage, the balloon is inflated, allowing the blocked artery to widen and thus breaking up any plaque formations.[4]
Dangers of Silent Ischemia
Diagnosis of Acute Myocardial Infarction
Severe chest pain is a symptom but not the only test for patients to be aware of any pending damage to cardiac function. Proper clinical diagnosis of heart attacks requires physical exams and diagnostic tests from a trained cardiologist. Some commonly used tests for MI include Electrocardiogram (ECG), Echocardiogram, angiograms, nuclear stress test (heart Stress tests), CT coronary angiogram scan, Cardiac catheterization, and blood tests. The Heart Regeneration Center also offers genetic screening to look for mutations in genes that might lead to heart disease or heart attacks using the following genetic markers:
TAZ,CAV3,CRYAB,CSRP3,TNNC1, TNNI3, JUP,DOLK, DES,VCL,MYL3, ACTC1, ACTN2,GAA, GLA,RBM20, RYR2, SCN5A, SGCD,TCAP, TMEM43, LAMP2,PRKAG2, RAF1,EYA4,ABCC9,DSC2 LMNA,MYBPC3,PKP2,PLN,DSG2, DSP,AGL,BAG3,TNNT2, TPM1,FHL1,EMD, MYH7, MYL2,HCN4,FKRP, FKTN, FLNC, TTN, TTR, SLC22A5,CTNNA3,LDB3,CACNA1C, ANKRD1, PDLIM3 and DMD.
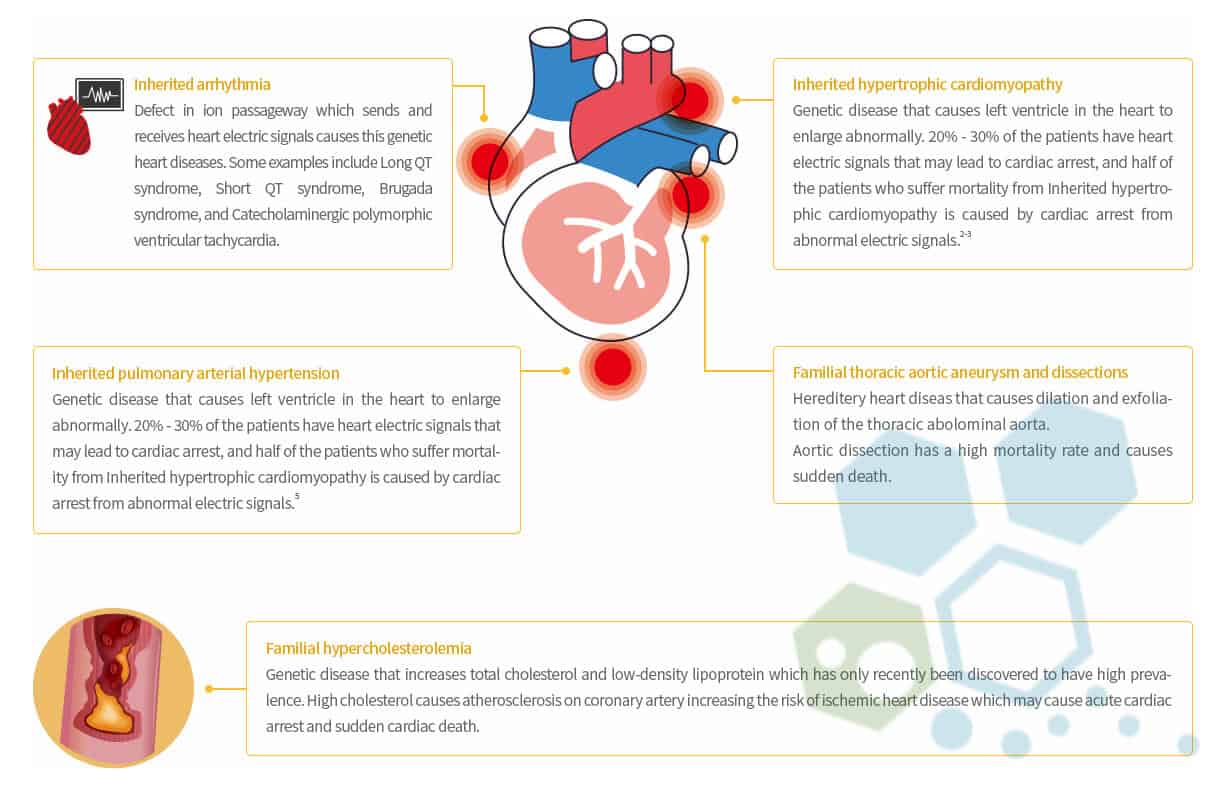
Proactive Genetic screenings are recommended for family members of patients who may have had sudden cardiac events in the past. Early intervention is vital in managing any condition so direct relatives can use non-invasive DNA tests to see if they carry any gene mutations. Please note the Regeneration Center does not offer gene therapies to treat congenital heart disease. Still, there are currently several clinical trials underway to potentially provide a cure for genetic heart diseases one day. To help reduce any risk of heart attacks, consider watching your weight, making dietary changes, and getting regular exercise to avoid osteoarthritis.
Stem Cells for Coronary Thrombosis
Cardiac Stem cell treatments (CSCs) are the only safe and non-surgical method to repair heart attack damage and improve ventricular muscle function after ischemic injury. Recent stem cell research has shown that cardiac stem cell repair works effectively by engrafting new cardiomyocytes, endothelial cells, progenitor cells, and cardiac pacemaker cells to the infarct zone (damaged area), which helps to replace the (necrotic) dead myocardial tissue, induce arteriogenesis, and help establish new blood microvessels through the process known as angiogenesis. Another issue that can occur due to heart attacks is Atrial fibrillation (AFib) or irregular heartbeats. AFib doesn’t directly cause a heart attack, and a heart attack causes atrial fibrillation or Nonvalvular atrial fibrillation (AF). Suppose the coronary artery is damaged after an acute myocardial infarction. In that case, the lack of consistent blood flow can damage the atrial tissue, resulting in tissue fibrosis, leading to heart murmurs and uncoordinated heartbeats. If the heart pumps less effectively due to damage/fibrosis, it leads to a higher risk of strokes, periods of rapid heart rates, angina & atrial fibrillation.
Cardiac Myopathy – Angina vs. Heart Attack
The Regen Centre Treatment for Heart Attacks uses cultured and differentiated UC-MSC+ stem cells to restore lung and cardiac function via revascularization. The enhanced hematopoietic stem cells used in treatments for Congestive Heart Failure and coronary heart disease yield significantly larger populations of cardiomyocytes, allowing for better long-term cardiovascular health and reducing the risk of another significant CV event and potential lung disease, COPD, IPF, liver cirrhosis, or kidney failure complications.
1 Year After Stem Cell Treatment for Heart
The heart regeneration protocol for damaged myocardium treatment also focuses on creating endothelial and vascular muscle cells that help increase the blood supply needed for myocardial repair and the paracrine effect. Cell development improves Paracrine signaling (cell-cell communication), which is critical in helping induce regenerative changes in surrounding progenitor cells and can be observed after cell infusions in (bFGF) fibroblast growth factors, (PDGF) platelet-derived growth factors, interleukin-1b & TGF-b and plays a vital immunomodulatory role in repairing heart tissue after heart attacks.[5]
Coronary Arteriogenesis & Cardiopoietic Stem cell Therapy
Methods of delivery of adult cardiac myocytes to the damaged myocardium can be done using both surgical and noninvasive methods, depending on the patient’s condition and needs. Minimally invasive means include catheter-based cell delivery, intracoronary transplantation, and Intracoronary or trans-endocardial injection; however, they carry more risk, resulting in the need for simultaneous open heart surgery. Through proper cell culturing, Cell Isolation, G-CSF, and cell differentiation techniques, non-invasive, non-surgical cell delivery can be achieved using the combination of intravenous and intramuscular cell infusions needed to circumvent dead heart muscle. Learn more about the basics of stem cells.[6]
Heart Regeneration Therapy Guidelines – 2025
The number of Cardiopoietic Stem cells needed will vary based on patient needs. Severe cases with multiple commodities may require a multiple-stage delivery using transvascular injections with direct injection Into the ventricular walls to ensure optimal results. Cardiopoietic stem cells represent a promising avenue for cardiac regeneration, as they are specifically directed to form heart tissue. These cells are developed by reprogramming mesenchymal stem cells into a lineage committed to heart repair, guided by a unique combination of growth factors. Growth factors, such as transforming growth factor-beta (TGF-β), bone morphogenetic proteins (BMPs), and vascular endothelial growth factor (VEGF), play a pivotal role in this process by promoting the differentiation, survival, and function of these stem cells within the damaged cardiac tissue. The synergy between cardiopoietic stem cells and growth factors enhances the regenerative potential, aiming to restore heart function and improve clinical outcomes in patients suffering from heart disease.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating heart attacks, CHF, atherosclerosis, coronary artery disease (CAD), or ischemic heart disease (IHD) with stem cells. Patients with multi-organ involvement, advanced heart failure, severe arterial blockages, recent artery bypass graft surgery, severe scarring, significant cardiovascular complications, or other major health conditions might not be good candidates for treatment.Repair Damaged Heart Muscles w/ Stem Cells
The ultimate goal of our cellular transplantation after heart attacks is first to stop the progression of the disease and the regeneration of any lost heart muscle. The overall success of any heart attack or heart valve regeneration treatment is measured 3-5 months after therapy using updated tests. The total number of cells needed for maximal efficacy will depend on several factors, including the patient’s current health and the age of the injury. Please note Cardiac regeneration therapy after heart attacks is not a 1-3 day treatment and requires multiple stages over two weeks. Due to varying severity, our medical team must review the patient’s current and historical condition before acceptance. For eligible patients, a complete treatment plan shall be provided with specifics of the protocol and the fixed medical costs of treating heart attacks with stem cells. To begin a medical evaluation, please prepare recent test results from an EKG, Tilt Table Heart CT Scan, Echocardiogram, or SPECT exam (Single-photon emission computed tomography) and contact us today.
Physical Rehabilitation Post MI Therapy: Rehabilitation therapy is optional based on the patient’s time constraints. Complete rehabilitation and nursing care can be provided 2-6 hours per day and up to 5 days per week
. Medical visas and accommodations for the patient and family/friends at an extended-stay hotel can also be included upon request.
Published Clinical Citations
[1] ^ Srimahachota, Suphot, Smonporn Boonyaratavej, Pairoj Rerkpattanapipat, Somjai Wangsupachart, Monravee Tumkosit, Udomsak Bunworasate, Thayapong Na Nakorn, et al. 2011. Intra-coronary bone marrow mononuclear cell transplantation in patients with ST-elevation myocardial infarction: a randomized controlled study. Journal of the Medical Association of Thailand Chotmaihet thangphaet, no. 6. https://www.ncbi.nlm.nih.gov/pubmed/21696072
[2] ^ Hou, Jingying, Lingyun Wang, Jieyu Jiang, Changqing Zhou, Tianzhu Guo, Shaoxin Zheng, and Tong Wang. 2013. Cardiac stem cells and their roles in MI. Stem cell reviews and reports, no. 3. doi:10.1007/s12015-012-9421-4. https://www.ncbi.nlm.nih.gov/pubmed/23238707
[3] ^ Limsuwan, Alisa, Pavit Pienvichit, Thosaphol Limpijankit, Pongsak Khowsathit, Suradej Hongeng, Ratanaporn Pornkul, Suvipaporn Siripornpitak, and Sarana Boonbaichaiyapruk. 2010. Transcoronary bone marrow-derived progenitor cells in a child with myocardial infarction: first pediatric experience. Thailand Clinical cardiology, no. 8. doi:10.1002/clc.20463. https://www.ncbi.nlm.nih.gov/pubmed/20632394
[4] ^ Carvalho, Edmund, Paul Verma, Kerry Hourigan, and Rinti Banerjee. 2015. Myocardial infarction: stem cell transplantation for cardiac regeneration. Regenerative medicine, no. 8 (November 13). doi:10.2217/rme.15.63. https://www.ncbi.nlm.nih.gov/pubmed/26563414
[5] ^ Boonbaichaiyapruck, Sarana, Pavit Pienvichit, Thosapol Limpijarnkij, Pairoj Rerkpattanapipat, Apichai Pongpatananurak, Ratchanee Saelee, Artit Ungkanont, and Suradej Hongeng. 2010. Transcoronary infusion of bone marrow derived multipotent stem cells to preserve left ventricular geometry and function after myocardial infarction. Clinical cardiology, no. 7. doi:10.1002/clc.20545. https://www.ncbi.nlm.nih.gov/pubmed/20552656
[6] ^ Nartprayut, Kuneerat, Yaowalak U-Pratya, Pakpoom Kheolamai, Sirikul Manochantr, Methichit Chayosumrit, Surapol Issaragrisil, and Aungkura Supokawej. 2013. Cardiomyocyte differentiation of perinatally‑derived mesenchymal stem cells. Molecular medicine reports Thailand, no. 5 (March 4). doi:10.3892/mmr.2013.1356. https://www.ncbi.nlm.nih.gov/pubmed/23467912