The Liver is the largest internal organ in the body and is located directly below the right lung. The Liver consists of the right lobe and left lobe, which comprise hepatocyte cells responsible for processing the nutrients from the blood. Hepatocytes help break down and store some nutrients and also help remove any waste from the body. The Liver also produces bile fluid that helps us break down drugs, alcohol, and other toxic waste in the blood, then passes from our body through stool and urine. A liver cancer diagnosis is often due to cancer metastasizing from a different area, such as in myeloma, and is therefore known as secondary liver cancer. The different types of cells in the Liver can result in many cancerous (malignant) and noncancerous (benign) tumors. These variations of tumors all have various causes and must be treated differently.
Global Liver Cancer Statistics
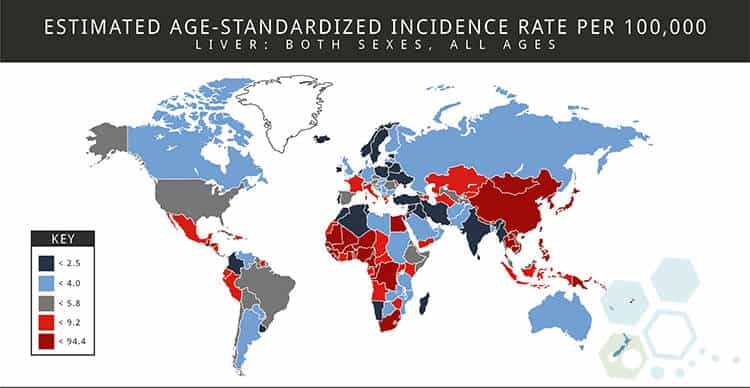
Based on recent statistics from 2019, Liver cancer is the fourth most commonly occurring cancer in men and the eighth-most common cancer type in women. The total number of patients with primary liver cancer has nearly tripled since the 1980s due to liver disease growth due to conditions such as hepatitis C. Primary liver cancer generally tends to be diagnosed in patients in their 50s and 60s and is more frequently found in men.[1]
Types of Liver Cancer
There are many liver cancer variations, and each type is quite different in the way it develops and mutates over time. Treatment options also vary depending on the diagnosis’s type, scale, and severity. The three most common types of liver cancer include:
Hepatocellular carcinoma (HCC) 
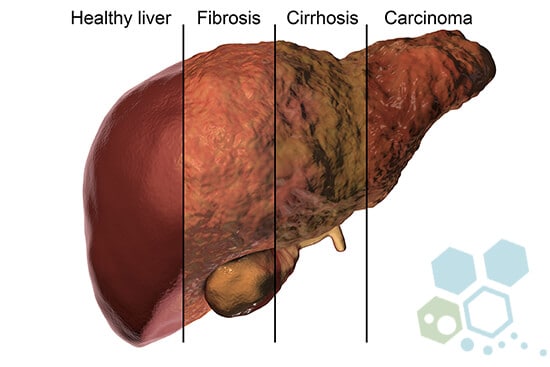
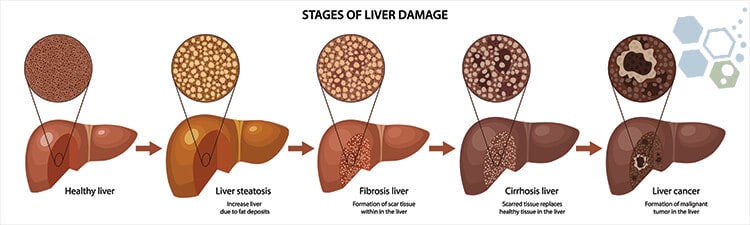
HCC is the most common form of primary liver cancer in the world. This type of cancer starts in the hepatocytes (liver cells), which process nutrients in the blood. HCC Cancer often develops as a single small tumor that spreads (metastasizes) to other organs and tissue in the body. Another type of HCC liver cancer starts as many tiny cancer nodules in the Liver (instead of a single tumor). This type of liver cancer is most often seen in patients with chronic hepatic tissue damage and liver cirrhosis. Many patients with hepatocellular carcinoma also have some other disease of the Liver that is causing inflammation and fibrotic scarring in the liver, including:
- Fatty liver disease, which can be attributed to excessive alcohol consumption and end-stage alcoholic liver disease
- Chronic hepatitis B or C virus
- Metabolic abnormalities, such as hemochromatosis (too much iron in the body) or nonalcoholic fatty liver disease.
Bile duct cancer – Intrahepatic Cholangiocarcinoma
Intrahepatic cholangiocarcinoma (cancer of the Bile ducts) is the second most diagnosed type of primary liver cancer. This type of liver cancer usually starts with bile duct cells (tube-like structures) that deliver bile; about 15% to 25% of cases of this type of cancer are intrahepatic cholangiocarcinomas. Many cholangiocarcinomas also start forming in the bile ducts outside the Liver.
Hemangiosarcoma and Angiosarcoma
These rare liver cancers usually form on the cell lining of blood vessels inside the Liver. Common causes of Angiosarcoma and Hemangiosarcoma include patients exposed to toxins such as thorium dioxide (Thorotrast) and vinyl chloride. Other known risk factors include environmental exposure to radium or arsenic, which can also be diagnosed due to mutations in the DNA, resulting in an inherited condition called hereditary hemochromatosis. In more than 40% of cases, the diagnosis is considered idiopathic, as no clear link can be identified. [2]
Tumors from Hemangiosarcoma and Angiosarcoma cancer increase and are often too widespread to be treated surgically by the time they are discovered. In some cases, radiation therapy (Chemotherapy) might help slow the disease, but these methods often fail as these particular types of cancers are challenging to treat.
Fibrolamellar-Hepatocellular Carcinoma (FLL-HCC)
Also called fibrolamellar carcinoma, this type of hepatocellular carcinoma is quite rare and is considered less aggressive than other known liver cancer types. FLL-HCC usually develops in young adults and is often misdiagnosed as a type of focal nodular hyperplasia, a noncancerous liver tumor.
Hepatoblastoma
This rare type of primary liver tumor usually develops in children less than five years old. When seen under a microscope, the hepatoblastoma cells look very similar to fetal liver cells, comprised of tissue resembling bile duct cells, fetal liver cells, or mature liver cells. Hepatoblastomas are curable with chemotherapy or surgery, but the tumors become much more challenging to treat if they spread outside the Liver.
Metastatic liver cancer – Secondary liver cancer
When liver cancer is found, it does not develop there. Still, it has metastasized (spread) from other organs in the body, including the colon, RCC Kidney Cancer, lung cancer, pancreas cancer, stomach, bowel cancer, prostate cancer, mesothelioma, or breast cancer. Since this type of cancer has spread from another (primary) site, it is referred to as secondary liver cancer. The tumors’ naming and treatment options are based on the original primary site where they started. For example, cancer that begins in the pancreas and spreads to the Liver is called Pancreatic cancer, and not liver cancer. It is also treated like pancreatic cancer. In Europe and North America, secondary (metastatic) liver tumors are more commonly diagnosed than primary liver cancer, but the opposite is true for many parts of Asia (Thailand) and Africa.
Benign Liver Tumors
Sometimes, the tumors found in the Liver are classified as noncancerous (benign). This type of cancer usually doesn’t cause any severe symptoms or discomfort. Benign liver tumors are often found by chance when a patient undergoes imaging tests for other health conditions. Common benign tumors in the Liver include:
- Cysts in the Liver
- Adenomas
- Focal nodular hyperplasias
- Hemangiomas
4 Stages of Liver Cancer
When a patient is clinically diagnosed with liver cancer, oncologists will first try to determine if the cancer tumors have spread and, if so, how far. This diagnosis process is called 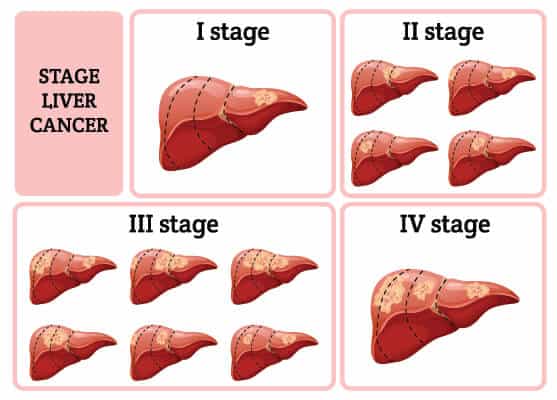 staging. The stages of cancer describe how severe the cancer is in the body. Staging helps doctors determine how severe the cancer is and what the best treatment option is. Oncologists also use a patient’s cancer stage to discuss realistic survival chances.[3]
staging. The stages of cancer describe how severe the cancer is in the body. Staging helps doctors determine how severe the cancer is and what the best treatment option is. Oncologists also use a patient’s cancer stage to discuss realistic survival chances.[3]
Stages for liver cancer can range from stage I (1) through IV (4). Generally speaking, the lower the stage number, the less cancer has spread. A higher stage (stage 4) means the liver cancer has spread more. Each patient’s cancer experience is unique, but cancers with similar stages generally have similar outlooks and are typically treated the same way. The staging systems vary around the world, but the most common systems include:
- AJCC (American Joint Committee on Cancer)
- The Okuda System
- Child-Pugh score
- The Cancer of the Liver -CLIP Italy
- The Barcelona Clinic Liver Cancer (BCLC) system
These different types of staging systems are usually not compared against each other, and usage depends a lot on where you reside. At this time, there is no universal staging system that all doctors use.
Classifications of Liver Cancer
Staging systems can often help oncologists determine outlook. Still, for treatment purposes, some doctors classify liver cancers much more simply, depending on whether they can be surgically cut out (resected). Resectable cancer means that the tumor can be removed via surgery (partial hepatectomy.) Other types of simple classifications include:
Unresectable liver cancer: Cancers that have not yet spread distant organs or lymph nodes but can’t be removed entirely via means of surgery are classified as unresectable cancers. These types of liver cancers include those that have spread through the entire liver organ or cannot be safely extracted due to proximity to sensitive areas around the Liver, including the veins, main arteries, or bile ducts.
Transplantable liver cancer (Potentially resectable) – If patients are healthy enough for surgical intervention, liver cancer can be removed entirely by either surgery or treated using immunotherapy or total liver transplant. This generally is an option for patients in stage 1 and some stage 2 cancers but requires that patients do not have liver cirrhosis or any other severe medical conditions. A minimal number of patients diagnosed with liver cancer have these types of tumors.
Inoperable liver cancer: If the liver cancer is small enough and in a safe place to be removed, but a patient is not healthy enough to have surgery, it will be classified as Inoperable. This usually occurs because a noncancerous part of the Liver might not be healthy enough (due to cirrhosis, etc.). If the cancer is removed surgically, there might not be enough healthy liver tissue remaining for a properly functioning liver. This classification is also reached if a patient has comorbidities that would make surgery dangerous.
Advanced (metastatic) liver cancer: Cancers that have already spread to the lymph nodes or other organs in the body are classified as advanced. Most advanced liver cancers cannot be treated with surgery alone.
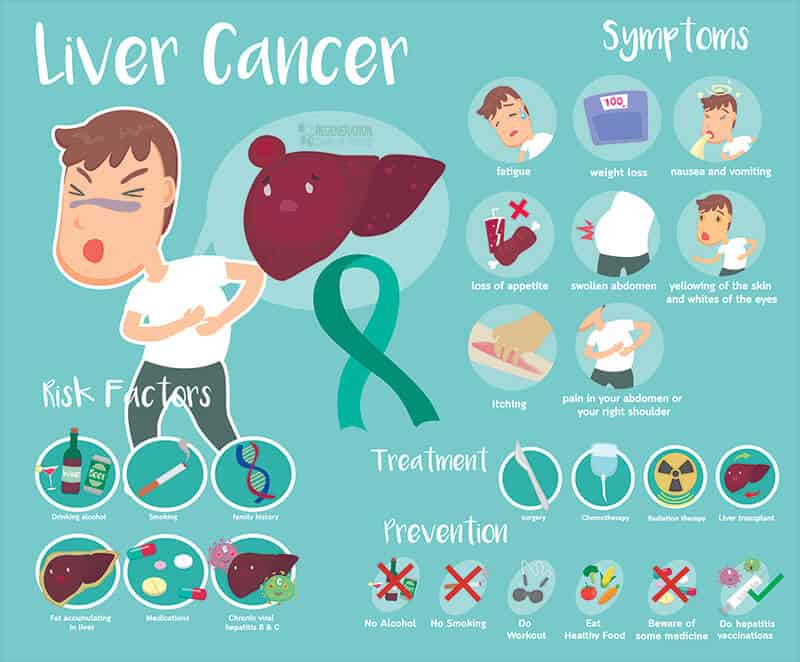
Symptoms of Liver Cancer
Common Symptoms associated with HCC & Liver Cancer include:
- Loss of appetite
- Pain in the right shoulder
- Feeling of weakness
- Weight Loss
- Jaundice
- Nausea
- Fever
- Abdomen pain/discomfort or swelling
- Elevated liver enzymes found on Liver Function Test
Liver Cancer Prevention & Risk Factors
Major Risk Factors associated with cancer in the Liver include:
- History of Liver Cirrhosis
- Reaction to foods containing aflatoxins, a family of toxins produced by some fungi (commonly found on maize, tree nuts, corn, peanuts, and cottonseed
- Smoking tobacco
- Alcohol abuse
- Obesity
- History of Diabetes
- History of the Hepatitis B and C Virus
- Men have a greater risk of developing liver cancer than women
- The average age at which patients develop liver cancer is about 55
- Exposure to environmental toxins
Hepatitis B or C infections or drinking too much alcohol are often contributors to scarring of the Liver—asymptomatic viral infections from HBV cause more than 75 percent of primary liver cancers worldwide. Primary liver cancer caused by viral infections and hepatitis develops slowly over decades and often goes undetected. Preventative medical screening for infections helps prevent them from becoming advanced and causing cancer. Chronic systemic infections of Hepatitis C virus (HCV) and Hepatitis B virus (HBV)are major risk factors for developing liver cancer.[4]
Diagnostic Tests for Detection of Cancer in the Liver
Several types of medical tests can be done to detect or eliminate the possibility of liver cancer tumors. Standard diagnostic tests include:
- Physical examination with a general physician or gastroenterologist to get information about your medical history to determine overall risk factors for developing liver cancer. Physical exams of the abdomen area, skin, and eyes (signs of jaundice). Depending on the initial physical exam findings, further tests may be required to determine the cause of symptoms.
- Radiology tests and imaging—As the name implies, Imaging results provide clear visual scans of internal body parts using X-rays, magnetic fields (MRI), or sound waves (Ultrasound). CT scans, bone scans, and angiography are some other standard tests done to evaluate liver cancer.
- Laparoscopy procedures use a thin tube with a camera inserted through the abdomen to better see the liver tissue and surrounding organs. Diagnostic laparoscopy is a low-risk, minimally invasive surgical procedure that requires microincisions. It can be performed to better determine the current stage of liver cancer, help create a customized stem cell treatment plan, or confirm an existing diagnosis.
- Liver Biopsy is a surgical procedure that can help detect cancer cells’ presence through a sample of patient liver tissue.
- Lab tests and blood panels are very inexpensive and effective means of determining whether the body and internal organs are functioning correctly, tracking treatment progress, searching for cancer markers, or detecting the recurrence of cancer.
- Genetic screening for Cancer—ctDNA (Circulating tumor DNA) analysis differs from traditional diagnostic tests that were available. Unlike invasive tissue biopsies, Cancer biomarker assessments like ctDNA Analysis require simple saliva samples or cheek swabs. Rapid screening is a prognostic marker detection that is consistently predictive. It can provide a very early assessment of potential metastatic disease, treatment monitoring, and determination of epigenetic and genetic alterations from primary cancers.
Immunotherapy Liver Cancer Treatment in 2025
Available Treatments for HCC and Liver Cancer
Most patients diagnosed with liver cancers are treated with combinations of radiation therapy, chemotherapy, or surgery. Radiation-based therapies are disadvantageous as the high-energy particle rays do not target the cancer cells and destroy healthy cells, causing severe side effects. The levels of radiation exposure in chemotherapeutic doses must be limited to avoid organ toxicity. Therefore, the 21st-century approach requires more precisely targeted therapies that kill cancer cells while ignoring the healthy cells. The combination of modern immunological cancer therapies and stem cells is much more targeted and less toxic while maintaining similar and often better results depending on the type, age, and diagnosis stage. Immune-boosting therapies are also more effective in achieving long-term tumor immunosurveillance while reducing the chance of relapse.
It is time to change how the world treats cancer
Immunological therapies can increase long-term disease-free survival and are prescribed as adjuvant therapy for patients with low white blood cell counts. Stem cell therapy for liver cancer helps boost a patient’s immune system with a naturally produced growth factor to enhance the cancer-fighting capacity.[5]
Immunotherapy for liver cancer is quickly becoming a standard-of-care treatment and, in some cases, a complete cure. Immunotherapies refer to manipulating or mobilizing the patient’s immune system to treat or cure liver cancer. Immunological therapies can also be performed via manipulation of genes using NK Cells, Dendritic cells (DCs), Monoclonal antibodies therapy, Immune modulators, adoptive cell transfer, an oncolytic virus therapy, which is a virus-based delivery system of modified genes where the payload uses the viruses as a host to carry past the patient’s immune system.
Immunotherapy for liver cancer

Patients diagnosed with HCC who initially might have responded well to medications that target PD-1 protein (checkpoint inhibitors) can, over a short time, develop resistance to these therapies, significantly if cancer has metastasized from its primary location to spawn additional liver tumors. In such cases, genes encoded with tumor-associated antigens (TAA) induce an adequate response from the immune system.
Earlier clinical trials on liver cancer focused on identifying the proliferating progenitor cells (CD34+) in human blood. These progenitor cells are stimulated by cytokines (GM-CSF and TNF-alpha) to differentiate into dendritic cells rapidly. In some cases, using a combination of IL-4 and GM-CSF helps generate significantly larger quantities of cancer-fighting dendritic cells from monocytes and macrophages.
Immunological therapy for liver cancer might soon be the gold standard in the treatment of liver tumors for these reasons:
- Targeted Liver cancer immunotherapy can target and debulk the tumor mass at the same time, kill cancer via inducing a normal cellular response and paracrine cell signaling
- Immunological therapies help save a copy of the memory responses (immunosurveillance). This significantly reduced the risk of relapses.
- Combining stem cells and immunotherapy growth factors helps reduce nearby lesions. It prevents metastases from forming on the cellular level, thus improving cytoreduction while avoiding the destruction of normal healthy cells.
- Liver Cancer stem cell therapies are non-toxic and may not require chemotherapy and its adverse side effects.
- Recent data indicate that adoptive T-cell therapy is successful in the treatment of liver cancer. This breakthrough therapy for HCC is essential as without having the treatment, the estimated five-year survival rate is just below 5%.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Liver Cancer, including Hepatocellular Carcinoma, with stem cells or immunotherapy. Patients with advanced liver failure, severe metastasis, or other critical health conditions might not be good candidates for treatment.CAR-T Cell Therapy for Liver Cancer
The Regeneration Center offers an alternative treatment for liver cancer using Chimeric Antigen Receptor T-Cell Therapy for cases with Metastatic Prostate Cancer that can treat or reverse symptoms depending on the patient’s stage and severity. The best defense from any cancer is first being informed about the disease to make an informed decision about current cancer treatment options using stem cells.
Role of Stem Cells in Treatment for Liver Cancer
Our stem cell treatments for liver cancer are explicitly customized to patient needs. The individualized protocol helps patients fight cancer using traditional cancer treatment and alternative natural cellular-based therapies. For over a decade, our approach to integrated healthcare has relied on research-based treatment plans that are comprehensive and specific to patient medical needs to ensure the highest chances of success. Our Cell Regeneration therapies offer a holistic approach to health care. We strive to fight cancer and alleviate underlying symptoms that can increase the patient’s quality of life. Our cancer stem cell treatment also focuses on long-term remission by addressing potential underlying causes of the disease.
Warning and Dangers of Herbal Therapies
Some herbal-based supplements might help treat some symptoms associated with liver cancer, but patients diagnosed with cancers need to be extra cautious before digesting any unknown herbal remedies. A compromised liver may have difficulty breaking down or metabolizing some substances. In particular, patients with lung cancer have a challenging time processing alcohol. Since many herbal preparations and extracts are alcohol-based, liver cancer patients should always double-check all the ingredients before taking any herbs. Furthermore, some herbal supplements for liver cancer might cause excessive bleeding and prevent blood from clotting properly.
Primary liver cancer can be defeated. Our goal is to heal patients for sustained long-term remission of liver cancer. Our hands-on approach to modern healthcare means that we will work with you and your primary care doctor to determine the best overall treatment options based on the stage and severity. Our medical evaluation requires the evaluation of current medical records. Our experienced cancer team has successfully treated hundreds of patients for nearly two decades. Immunotherapy is not appropriate for all cases, but patients who are not responding to traditional treatments or those for whom surgery is not a good option can benefit. Please contact us so our team can review current medical records Radiology scans (CT, ultrasound, or MRI) and lab tests to target the tumor(s) better and destroy them using minimally invasive techniques.
We provide our patients with access to the most innovative cancer treatment techniques and immunotherapies with minimal side effects. The Regeneration Center also offers its patients comprehensive follow-up care and survivorship programs (in Thailand only) for patients recovering from primary liver cancer.
The outlook for patients diagnosed with primary liver cancer has never been better. Thanks to modern medicine, many people survive the disease. The Regeneration Center has cared for cancer patients worldwide who were diagnosed with different types of primary liver tumors and some rare types, such as hepatoblastoma and angiosarcoma. To learn more about our stem cell treatment protocols for the treatment of liver cancer, please contact us today.
Published Clinical Citations
[1] ^ Wogan GN. Dietary factors and special epidemiological situations of liver cancer in Thailand. Cancer Res Nov;35(11 Pt. 2):3499-502. PMID: 1104156.
[2] ^ Sun, J. H., Luo, Q., Liu, L. L., & Song, G. B. (2016). Liver cancer stem cell markers: Progression and therapeutic implications. World journal of gastroenterology, 22(13), 3547–3557. https://doi.org/10.3748/wjg.v22.i13.3547
[3] ^ Xiao Y, Lin M, Jiang X, et al. The Recent Advances on Liver Cancer Stem Cells: Biomarkers, Separation, and Therapy. Anal Cell Pathol (Amst). 2017;2017:5108653. doi:10.1155/2017/5108653
[4] ^ Zhang, W., Mu, D., & Feng, K. (2017). Hierarchical potential differentiation of liver cancer stem cells. Advances in clinical and experimental medicine : official organ Medical University, 26(7), 1137–1141. https://doi.org/10.17219/acem/66343
[5] ^ Liu CY, Chen KF, Chen PJ. Treatment of Liver Cancer. Cold Spring Harb Perspect Med. 2015;5(9):a021535. Published 2015 Jul 17. doi:10.1101/cshperspect.a021535