Lyme borreliosis, better known as Lyme disease, is caused by the Borrelia bacterium (Borrelia burgdorferi) and is often spread by ticks. B. burgdorferi can also be transmitted by bites from infected ticks who got infected after feeding on infected birds, deer, or mice.
What is Lyme Disease?
Most people with Lyme disease have no recollection of tick bites, even though a tick must be present on the skin for 1 or 2 days to transmit the infection. The transmittable disease was first diagnosed in Old Lyme, Connecticut, in 1975. Since then, it has become the most commonly diagnosed tickborne disease in Europe and North America. People living with domesticated animals have a higher risk of acquiring Lyme disease. Still, people who like the outdoors or spend time in wooded areas also have a higher risk of getting this illness.
Symptoms of Lyme Disease
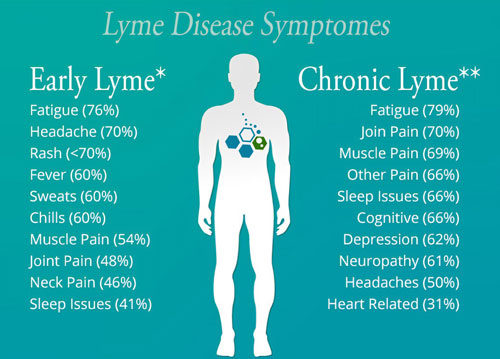
For many parts of the North America and Eastern Europe, Lyme disease season is coming to a close. But for some people who spent time in woodlands, parks, or working in their gardens during the summer and autumn, symptoms of chronic Lyme disease have just begun to present themselves. The New England Journal of Medicine reports that 10% and 20% of patients undergoing antibiotic treatment will develop persistent Lyme disease. Chronic Lyme disease symptoms include:
- Fatigue
- Joint pain
- Muscle aches
- Cognitive dysfunction and Brain Fog
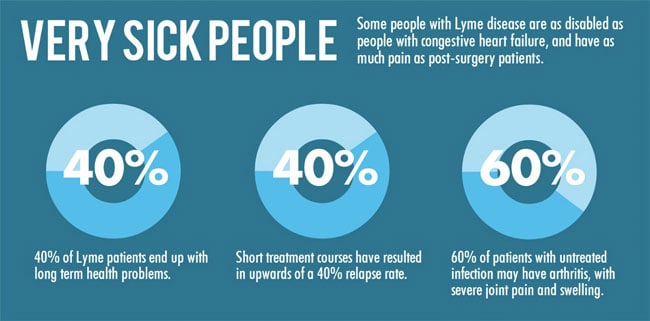
These can persist for as much as six months and, in some cases, even longer. They can become severe enough to impede the patient’s ability to perform everyday activities and cause considerable emotional distress. While most people do recover from chronic Lyme disease within a year, there are cases where treatment for chronic Lyme disease must continue beyond this time frame.[1]
Chronic Lyme disease
Lyme disease becomes chronic when it resists antibiotic treatment. It can also develop when someone doesn’t realize they’ve been bitten by a tick until months later when the more serious symptoms emerge. This phase is also known as persistent Lyme disease or post-treatment Lyme disease. When the disease resists antibiotics, Chronic Lyme disease treatment may need to shift to more advanced methods.
Why some people develop chronic Lyme disease while others do not is still unknown; equally unclear is what triggers the particular symptoms of persistent Lyme. What is understood is that treatment for chronic Lyme disease needs to be highly personalized, according to the patient’s specific history and the combination of symptoms that are present.
How is Lyme Disease Contracted?
Lyme disease is primarily contracted through tick bites, specifically from the black-legged tick, commonly referred to as the deer tick (Ixodes scapularis in the northeastern, mid-Atlantic, and north-central United States, and Ixodes pacificus in the western United States). These ticks are vectors for the bacteria Borrelia burgdorferi, the primary cause of Lyme disease. While tick bites are the most prevalent transmission mode, some medical experts suggest that other biting insects, such as mosquitoes or fleas, might occasionally carry the bacteria. However, these cases are sporadic and not widely documented [2].
It’s important to note that not all ticks carry Borrelia burgdorferi. For Lyme disease to be transmitted, a tick must first become infected by feeding on an animal already carrying the bacteria. Shared hosts include small mammals like mice, particularly white-footed mice, and larger animals like deer. A tick’s lifecycle involves multiple stages—larva, nymph, and adult—and they can pick up the bacteria at any stage by feeding on an infected host.
Once infected, a tick can transmit the bacteria to a human or animal during its next feeding. The transmission process typically requires the tick to be attached and fed for 36 to 48 hours or more. During feeding, the bacteria in the tick’s gut migrate to the tick’s salivary glands, from where they can be passed into the host’s bloodstream. This makes early detection and removal of ticks crucial in preventing Lyme disease.
Lyme disease is most prevalent in certain regions, particularly in the northeastern, mid-Atlantic, and north-central United States, where black-legged ticks are commonly found. In these areas, individuals who spend a lot of time outdoors in wooded or grassy areas are at a higher risk of encountering infected ticks. However, the risk of contracting Lyme disease can be significantly reduced with proper precautions, such as wearing protective clothing, using tick repellents, and conducting regular tick checks.
How Lyme Disease Develops into Chronic Lyme Disease
The exact reason why chronic Lyme disease develops is not yet understood. Some medical experts believe it may be due to Borrelia burgdorferi not being entirely eradicated in some people during the antibiotic regimen. Others think the damage to the immune system and the body’s tissues caused by the disease persists even after the bacteria have been eliminated. They believe chronic Lyme disease is the immune system continuing to respond to the damage as if the infection is still present.
Risk Factors for Acquiring Lyme Disease
Of course, risk factors for developing chronic Lyme disease begin with the bite of an infected tick. So, your first best defense against the disease becoming chronic is to thoroughly check yourself, your loved ones, and your pets for ticks after spending time outdoors.
Not receiving the recommended antibiotics for Lyme treatment may also increase your risk. With that in mind, however, there is a percentage of patients who will develop chronic Lyme disease even with the proper antibiotic regimen. Generally speaking, symptoms of chronic Lyme disease are very similar to those of the earlier stages. The main difference is the persistent nature of chronic Lyme disease symptoms.[3] These include:
- Fatigue
- Restlessness during sleep
- Body pain
- Achy joints or muscles
- Painful and swollen connective joints, such as knee, shoulder, or hips.
Chronic Lyme disease symptoms may progress to include:
- A decrease in short-term memory
- Difficulty in concentration
- Trouble with speech
- Mobility problems
Chronic Lyme disease can result in symptoms that become debilitating and cause extreme changes to the patient’s lifestyle.
Diagnosis of Chronic Lyme Disease
To plan the proper treatment for chronic Lyme disease, the patient undergoes a test to check antibody levels in the blood. Antibodies are what the body produces when confronted with disease-causing bacteria. The two most commonly used blood tests are the enzyme-linked immunosorbent assay (ELISA) and Western blot tests.
Additionally, your physician may order certain tests and exams addressing the specific symptoms of chronic Lyme disease. These may include:
- Electrocardiogram or echocardiogram to determine heart function (patients with heart disease or previous heart attack)
- Spinal tap to inspect cerebrospinal fluid (CSF)
- Magnetic resonance imaging (MRI) to observe neurological conditions
Important points
- Most tests for Lyme disease are only designed to detect antibodies made by our body in response to an infection.
- Antibodies in a patient commonly persist in the bloodstream for months or sometimes years after the initial infection is gone.
- Antibodies can also take several weeks to develop slowly, so some patients might test negative if recently infected.
- Some Lyme disease tests give results for two kinds of antibodies, IgG and IgM. A positive IgM result should be disregarded if the patient has been sick for over 30 days.
- Infections with other diseases, including some types of tickborne diseases or viral, autoimmune diseases such as MG with anti-MuSK antibodies or bacterial-related disease, can result in a false positive test result or be misdiagnosed.
Treatment of Chronic Lyme Disease
 As mentioned above, early intervention is the best weapon against Lyme disease, which means catching it in its early stages before it becomes persistent.
As mentioned above, early intervention is the best weapon against Lyme disease, which means catching it in its early stages before it becomes persistent.
Can Lyme disease be cured?
For most patients, this early intervention requires a 2 to 3-week course of oral antibiotics. The three antibiotics generally used are amoxicillin, doxycycline, and cefuroxime axetil. However, treatment will depend on each person’s health and the symptoms experienced [4].
Lyme Disease Breakthrough
Stem cell therapy has quickly emerged as one of the most advanced treatments for persistent Lyme disease. Since chronic Lyme disease exhibits many symptoms similar to autoimmune conditions, it is believed that stem cell therapy works by repairing and rejuvenating damaged cells, nerves, and tissues. Stem cell research has also increased popularity among physicians because it is a non-pharmaceutical-based natural therapy, as prolonged prescription medications and antibiotics can cause other complications.
What is CVID Syndrome?
Common variable immunodeficiency, or CVID, is considered a primary immune deficiency disease characterized by deficient levels of protecting antibodies, which increase the risk of infection. The disease is usually diagnosed in adults but can also occur in children. Patients with CVID often have chronic ear infections, sinus infections, and respiratory infections that can lead to COPD or pulmonary fibrosis.
How MSC+ Stem Cells Can Reduce the Neurological Effects of Lyme Disease
If left undiagnosed for too long, the neurological effects of Lyme disease can be challenging to treat with conventional medicine. But the real tragedy is the life-altering difficulties these symptoms can cause those afflicted and their loved ones. However, regenerative medical techniques like stem cell therapy are opening up promising possibilities for those suffering from neurological Lyme disease symptoms.
Stem cells are a natural product of the body. Among their functions, stem cells are what the body uses to help heal tissue and organ damage. For example, when you experience a cut to the skin, stem cells are the cellular “EMS” and “medical crews” that help heal tissue and blood vessels. They also promote the healing of muscles and stimulate cell re-growth. Stem cells have also been shown to be highly effective in the treatment of neurological conditions such as brain injuries, ALS, MND, and multiple sclerosis.
Benefits of Stem Cells for Lyme Disease
The long-term effects of Lyme disease are complex to address and just as challenging to live with, which is why stem cell therapy for Lyme disease offers such a promising solution for immunomodulatory and reversal of immunosuppressive effects. Borrelia bacteria’s impact on an adaptive immune is mainly due to its ability to evade our immune system checkpoints by hiding in protected niches in the body such as intracellular compartments and biofilms.
Lyme disease also destroys circulating lymphocytes and immunodeficiency syndromes because humoral immunity and immunoglobulin production have been suppressed after a Borrelia burgdorferi infection. Other infections like Mycoplasma and Bartonella (bartonellosis) are also frequently associated with immunological dysfunctions. Mycoplasmas are also often found to interact with B cells in the body and affect the production of antibodies.[5]
Circulating stem cells help the body heal from injury, disease, or infections by targeting antibody deficiency. If you cut yourself, the body releases chemical signals to recruit stem cells to help the skin, tissues, blood vessels, and muscles heal and regrow, completing the regenerative cycle. Stem cell therapy involves using autologous stem cells in the body or allogeneic mesenchymal stem cells for cord tissue or placenta. These stem cells and tissue-specific growth factors are then delivered back to the body in areas that need healing. This regenerative process is used to help speed recovery following surgery or medical therapies or to speed healing from a sports injury or other illnesses or injuries the body has sustained.
Stem cells Lyme disease therapy is focused on new applications for these powerhouse cells that can help all the patients who have suffered advanced cases and are now left with life-altering effects. Stem cells being used in testing for Lyme disease cell therapy can be taken from the patient’s own body or matched to the patient, so there is little to no risk of adverse side effects of the treatment.
The Outlook of Living with Chronic Lyme Disease
Most patients diagnosed with chronic Lyme disease will eventually recover from their symptoms. It is not unusual for people to experience them for months and sometimes years—however, advancements in regenerative medicine methods like stem cell therapy point to speedier recoveries for many people.
Preventing Lyme Disease
Following practices that lower your risk of tick bites is always your first and best defense against chronic Lyme disease. Below are several recommendations for Lyme disease prevention:
- Use pest control for your lawn areas.
- Use insect repellent while spending time in woody or grassy areas. The repellent should be applied to both clothing and exposed skin.
- When hiking trails, stay in the center to avoid brushing against shrubs, trees, and grass.
- Immediately change your clothes after spending time outdoors. Take the clothes to the laundry room, wash them, and expose them to high dryer heat.
- Do a thorough exam of your skin and scalp for ticks.
- Examine all pets for ticks.
- Use permethrin to treat clothes and footwear. This is an insect repellant that stays active through several washings.
If You Suspect Exposure From a Tick
If you find an attached tick or think an insect bite may be from one, notify your doctor of possible infection. Your doctor will likely advise you to be alert for symptoms for 30 days. Symptoms of early Lyme disease include:
- A rash at the site of the bite. It sometimes resembles a bull’s-eye.
- Fatigue
- Chills or general feeling of illness similar to the flu
- Itching
- Headaches
- Dizziness or feeling faint
- Aching muscles or joints
- Swollen joints
- Neck stiffness
- Enlarged lymph nodes
The Regeneration Center offers minimally invasive procedures via UC-MSC+ stem cells. Our methods are safe and have a low risk of side effects. Using isolated and enhanced stem cells and cell-specific growth factors, the Regen Center protocol offers a concentrated amount of exceptionally potent and abundant mesenchymal stem cells.
Stem cell therapy for Lyme disease is still in its early days. Still, stem cell researchers and our clinical applications have already benefitted from the potential of using stem cells and growth factors to help manage chronic symptoms or repair tissue damage caused by Lyme disease. The most commonly considered type of stem cells for this purpose are mesenchymal stem cells (MSCs), derived from bone marrow, adipose tissue, umbilical cord blood, or Wharton’s jelly. MSCs are known for their anti-inflammatory properties, ability to differentiate into various cell types, and potential to modulate the immune response, which could be beneficial in reducing inflammation and repairing tissues damaged by Lyme disease. Hematopoietic stem cells (HSCs), typically sourced from bone marrow, peripheral blood, or umbilical cord blood, are less commonly used in this context. However, they have been considered for their potential to reset the immune system in severe cases.
In addition to stem cells, various growth factors are used in our treatment to support stem cell therapy or enhance tissue repair. These include platelet-derived growth factor (PDGF), which stimulates cell proliferation and tissue repair; transforming growth factor-beta (TGF-β), which modulates immune responses and promotes wound healing; vascular endothelial growth factor (VEGF), which encourages blood vessel formation; and basic fibroblast growth factor (bFGF), known for promoting angiogenesis, wound healing, and tissue repair.
Effective management of Lyme disease in 2024
For nearly two decades, the Regeneration Center has successfully treated similar neurological conditions such as FMS, Strokes, ataxia, and Parkinson’s. Our stem cell therapy for patients with Lyme disease is ideal for those with advanced neurological symptoms. Our treatment aims to heal the body from the neurological damage caused by Lyme disease and Borrelia burgdorferi bacterial infections.
Our results have been encouraging. Patients report far better energy, a far-reaching decrease in severe symptoms, a reduction in symptoms (Antibiotic‐refractory Lyme arthritis), and impressive improvement in their general health. Most Regeneration Center patients report improvement a few days after therapy begins and get verified using updated immunoglobulin level tests. Treatment recommendations are based on patient needs and might require multiple treatment stages over approximately two weeks. In general, our unique protocol has shown to be the most effective in reaching the therapy’s full potential.
Published Clinical Citations
[1] ^ Ross Russell, A. L., Dryden, M. S., Pinto, A. A., & Lovett, J. K. (2018). Lyme disease: diagnosis and management. Practical neurology, 18(6), 455–464. https://doi.org/10.1136/practneurol-2018-001998
[2] ^ Ji, Z., Jian, M., Yue, P., Cao, W., Xu, X., Zhang, Y., Pan, Y., Yang, J., Chen, J., Liu, M., Fan, Y., Su, X., Wen, S., Kong, J., Li, B., Dong, Y., Zhou, G., Liu, A., & Bao, F. (2022). Prevalence of Borrelia burgdorferi in Ixodidae Tick around Asia: A Systematic Review and Meta-Analysis. Pathogens (Basel, Switzerland), 11(2), 143. https://doi.org/10.3390/pathogens11020143
[3] ^ Zhao, H., Liu, A., Shen, L., Xu, C., Zhu, Z., Yang, J., Han, X., Bao, F., & Yang, W. (2017). Isoforskolin downregulates proinflammatory responses induced by Borrelia burgdorferi basic membrane protein A. Experimental and therapeutic medicine, 14(6), 5974–5980. https://doi.org/10.3892/etm.2017.5300
[4] ^Horowitz R, Freeman PR. Improvement of common variable immunodeficiency using embryonic stem cell therapy in a patient with lyme disease: a clinical case report. Clin Case Rep. 2018 May 2;6(6):1166-1171. doi: 10.1002/ccr3.1556. PMID: 29881587; PMCID: PMC5986024.
[5] ^Krause, P. J., Telford, S. R., 3rd, Spielman, A., Sikand, V., Ryan, R., Christianson, D., Burke, G., Brassard, P., Pollack, R., Peck, J., & Persing, D. H. (1996). Concurrent Lyme disease and babesiosis. Evidence for increased severity and duration of illness. JAMA, 275(21), 1657–1660.