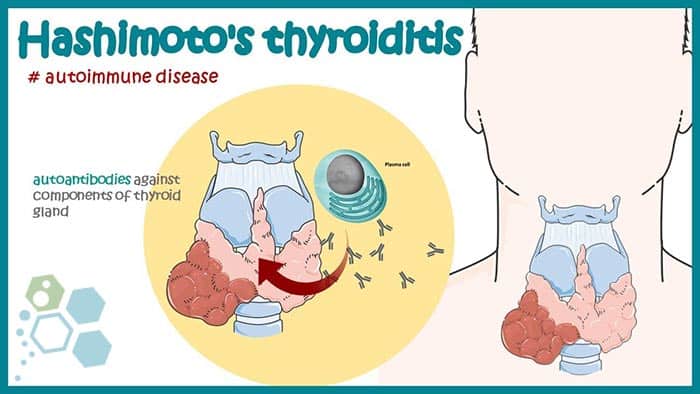
Hashimoto’s disease is an autoimmune condition that can cause an underactive thyroid, also known as hypothyroidism, or less commonly, an overactive thyroid, known as hyperthyroidism.
Hashimoto’s disease & Chronic thyroiditis
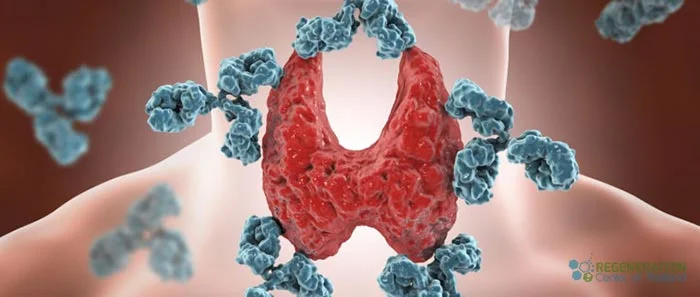
This disease affects the thyroid gland, which is a small gland found in the neck that produces thyroid hormones that control the body’s energy usage, influencing various organs, including the heart. Hashimoto’s disease produces antibodies that attack the thyroid gland, resulting in the accumulation of white blood cells in the gland and ultimately leading to its damage, which impairs its ability to produce enough thyroid hormones [1].
Hashimoto’s disease is also called:
- Hashimoto’s thyroiditis
- Autoimmune Thyroiditis
- Chronic lymphocytic thyroiditis
Current research shows that Hashimoto’s disease is four to ten times more common in women than men and is likely to develop more often in women aged 30-55. It can also hereditary, and individuals who have a family history of thyroid diseases or other autoimmune disorders such as Thymoma-associated myasthenia gravis, Type 1 diabetes, Ankylosing Spondylitis, Lupus, Connective Tissue Disease, Rheumatoid Arthritis, autoimmune pancreatitis, and Sjogren’s Syndrome are at a higher risk of developing it. Learn more about genetic testing for Autoimmune diseases.
What does Hashimoto’s disease do to a person?
Hashimoto’s disease may cause several health complications, including high cholesterol levels, high blood pressure, heart disease, heart attack, stroke and heart failure. Additionally, hypothyroidism can cause myxedema, a rare and life-threatening condition that slows down the body’s functions. Untreated hypothyroidism can also lead to pregnancy-related problems [2].
What are the symptoms of Hashimoto’s disease?
The symptoms of Hashimoto’s disease may not be apparent initially. However, as the condition progresses, the symptoms and complications from hypothyroidism may include:
- Fatigue

- Suddent weight gain
- Constipation
- Apnea (difficulty in breathing)
- Intolerance to cold temperature
- Irregular menstrual periods or fertility problems
- Menorrhagia (abnormal heavy bleeding during menstruation)
- Loss of libido resulting in ED
- Joint and muscle pain assosiated with osteoporosis & osteoarthritis
- Macroglossia (enlarged tongue)
- Liver inflammation, fibrosis, and necrosis
- Loss of memory and brain fog
- Blockage of Airway resulting in COPD and Lung Fibrosis
- Ataxia (difficulty in co-ordination, balance and speech)
- Depression
- Peripheral neuropathy
- Renal Disease & glomerulonephritis
- Hair thinning or dryness
- Bradycardia (Slowed heart rate)
The thyroid may become enlarged, leading to a swollen appearance in the neck called a goitre. Rarely, thyroid damage may cause too much thyroid hormone to be released into the bloodstream, resulting in hyperthyroidism.
What test are used to confirm Hashimoto’s disease?
Treatments for Hashimoto’s Thyroiditis
Once Hashimoto’s disease is diagnosed, treatment often involves thyroid hormone replacement therapy such as synthetic T3, T4 or desiccated thyroid extract. Hormone replacement threrapy involves taking a pill containing synthetic thyroid hormone, which helps replace the hormones your thyroid can no longer produce. Your doctor will monitor your hormone levels and adjust your medication to keep your levels within a healthy range. Some endocrinologist may also prescribe patients with a synthetic version of T3 & synthetic T4 for treating Hashimoto’s. This combination is sometimes used for patients who have persistent chronic hypothyroid symptoms but have normal TSH levels. In addition to medications, some lifestyle changes can help manage Hashimoto’s disease. A healthy, balanced diet rich in nutrients, particularly iodine and selenium, can help support thyroid function [3].
Regular exercise can also help manage symptoms, boosting energy levels and improving mood. Working closely with your doctor to manage Hashimoto’s disease is essential, as untreated hypothyroidism can lead to serious health complications. However, most people with non-complicated Hashimoto’s disease can live healthy, fulfilling lives with proper treatment and management.
Stem Cell Treatment for Hashimoto’s disease
Hashimoto’s thyroiditis is an autoimmune disease where lymphocytes destroy the thyroid gland. The current and traditional methods of treating the disease include surgery, hormone therapy, or immunomodulatory therapy, but they pose significant risks and side effects. This calls for finding new ways to treat the disease, including modified stem cells for Hashimoto’s disease. The Regeneration Center Stem Cell Clinic has found that ability transplanted MSC+ stem cells can help regulate Th17/Treg interactions in patients with Hashimoto’s thyroiditis. Our results and other clinical trials have shown that MSC+ stem cells can be a potentially beneficial and safe immunotherapy strategy for treating the disease [4].
Isolated and Expanded MSC+ cells have unique properties, such as being easily harvested from various stroma (autologous and allogeneic), carrying Major Histocompatibility Complex (MHC) antigens that are not frequently expressed and can be used to target injured organs or tissues. These properties make them promising for treating immune diseases, especially autoimmune disorders like Hashimoto’s.
New treatment for hashimoto’s thyroiditis
Autoimmune thyroid diseases (AITDs) target the functioning follicular cells, and many cytokines and immune cells are involved. Hashimoto’s thyroiditis is recognized as an AITD, characterized by lymph cell infiltration, fibrotic changes, and parenchymal atrophy. MSC+ isolated from a combination of umbilical cord tissue and Wharton’s jelly have therapeutic functions for patients with Hashimoto’s disease. The isolated MSC+ cells help reduce thyroid lesions through lymphoid infiltration by regulating Th17/Treg cell interactions. The isolated MSC+ cells are also given specific growth factors to help force the migration of newly transplanted cells to the inflammatory sites in the body.
Stem Cell Therapy for Thyroid Issues
The thyroid gland is a vital component of our endocrine system, responsible for secreting hormones that regulate cellular metabolism and development. Insufficient thyroid hormone levels can impair central nervous system function and cause low intelligence quotient and mental retardation. Hypothyroidism, a condition where the production of thyroxine is reduced, is often caused by autoimmune thyroid diseases such as fibrotic thyroiditis. Additionally, thyroid malignancies, including papillary thyroid cancer, follicular thyroid cancer, and anaplastic thyroid cancer, are a significant concern. Patients with advanced-stage carcinoma, particularly those with anaplastic thyroid cancer, often lose the chance for surgery once the diagnosis is confirmed, underscoring the urgent need for alternative functional medical treatments.
Role of stem cells in thyroid cell differentiation, thyroiditis & thyroid cancers
Stem cells are categorized based on their origins, including embryonic derived stem cells (ESCs), mesenchymal stem cells (MSCs), peripheral blood stem cells, organ resident stem cells (RSCs), cancer stem cells (CSCs), perinatal stem cells, and induced pluripotent stem cells (iPSs). The isolated and expanded MSC+ stem cells used by The Regeneration Center originate from the stroma surrounding organs and other tissues such as the umbilical cord and/or placental tissue [5]. Some organs, such as the brain, liver, and thyroid, have their own stem cells. Stem cells are also categorized based on their differentiation potency, ranging from totipotent, multipotent & unipotent cells that can be used in stem cell treatment for inclusion body myositis.
The potential applications of stem cells in regenerative medicine have been widely studied and have shown the capacity to develop into organs or tissues such as livers, hearts, skeletal muscles, and kidneys, as well as aiding in the development of the nervous system for patients with neurodegenerative diseases such as ALS, MND, Alzheimer, Parkinson’s disease, brain injuries,multiple sclerosis, strokes and spinal cord injuries. The challenge with stem cell therapy is imitating the complex microenvironments required for organ differentiation. Generated organs or tissues from stem cells without the proper types of cytokines, proteins and growth factors will lead to poor results as the transplanted cells will lack the necessarily affiliated cells and will not be able to function as natural ones.
Stem cell treatment for rheumatoid arthritis represents a promising new treatment option that will revolutionize the management of this chronic and debilitating disease. Although we are still in the early stages of stem cell science, the results so far are encouraging, and will only continue getting better results over time.
Cost for Treatment of Hashimoto’s with Stem Cells
MSC+ Stem Cell treatment for Hashimoto’s & Chronic Thyroiditis will require minimum of 12-14 days in total. Due to the varying degrees of severity, our medical team will need to evaluate all potential patients so that an appropriate protocol can be established. Upon approval, a detailed treatment plan will be provided that will include the specifics such as exact total number nights required along with the total medical related costs. To begin the evaluation process for our multi-stage rheumatoid arthritis treatment using stem cells please prepare your recent medical records such as radiology scans w/ blood test results and contact us today.
Published Clinical Citations
[1] ^Tempark T, Deekajorndech T, Chatproedprai S, Supornsilchai V, Wananukul S. Late sequelae of drug reaction with eosinophilia and systemic symptoms (DRESS) cause thyroid dysfunction and thyroiditis in Thailand: review of literature. J Pediatr Endocrinol Metab. 2022 Feb 4;35(5):567-575. doi: 10.1515/jpem-2021-0685. PMID: 35119800.
[2] ^ Rajatanavin R. Postpartum thyroid dysfunction: a viewpoint from Thailand. Ann Acad Med Singap. 1993 Jul;22(4):587-92. PMID: 8257065.
[3] ^Coppola A, Tomasello L, Pitrone M, Cillino S, Richiusa P, Pizzolanti G, Giordano C. Human limbal fibroblast-like stem cells induce immune-tolerance in autoreactive T lymphocytes from female patients with Hashimoto’s thyroiditis. Stem Cell Res Ther. 2017 Jul 3;8(1):154. doi: 10.1186/s13287-017-0611-5. PMID: 28673339; PMCID: PMC5496215.
[4] ^Al-Suhaimi EA, Al-Khater K. Functions of stem cells of thyroid glands in health and disease. Rev Endocr Metab Disord. 2019 Jun;20(2):187-195. doi: 10.1007/s11154-019-09496-x. PMID: 31025266.
[5] ^ Giolito MV, Plateroti M. Thyroid hormone signaling in the intestinal stem cells and their niche. Cell Mol Life Sci. 2022 Aug 10;79(9):476. doi: 10.1007/s00018-022-04503-y. PMID: 35947210.