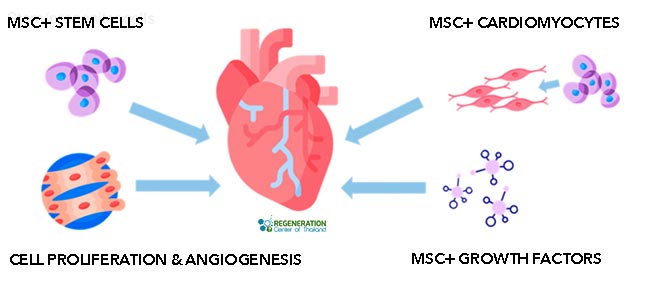
Cardiovascular diseases are one of the major causes of fatality in the world. Over the years, the rate of deaths caused by cardiovascular diseases has decreased in some countries while dramatically increasing in others. The percentage of premature deaths from cardiovascular illness ranges from a low of 3% in nations with a high GDP of up to 49% in low-GDP nations. More than 250 million individuals across the world lost their lives due to coronary heart disease and cardiovascular diseases in 2021. According to cardiac research, each year, heart illness kills significantly more humans than cancer. In recent years, Cardiometabolic and cardiovascular dangers in women have been growing at a fast rate and have killed a higher percentage of women than breast cancer has. Therapeutic cardiomyocyte regeneration using hematopoietic mesenchymal stem cells. Replace dead cardiomyocytes with functionally integrated cardiac and vascular endothelial cells (cardiogenesis.) Decrease inflammation and Angiogenesis to increase blood vessel wall growth in the heart.
Causes of Coronary Artery Disease
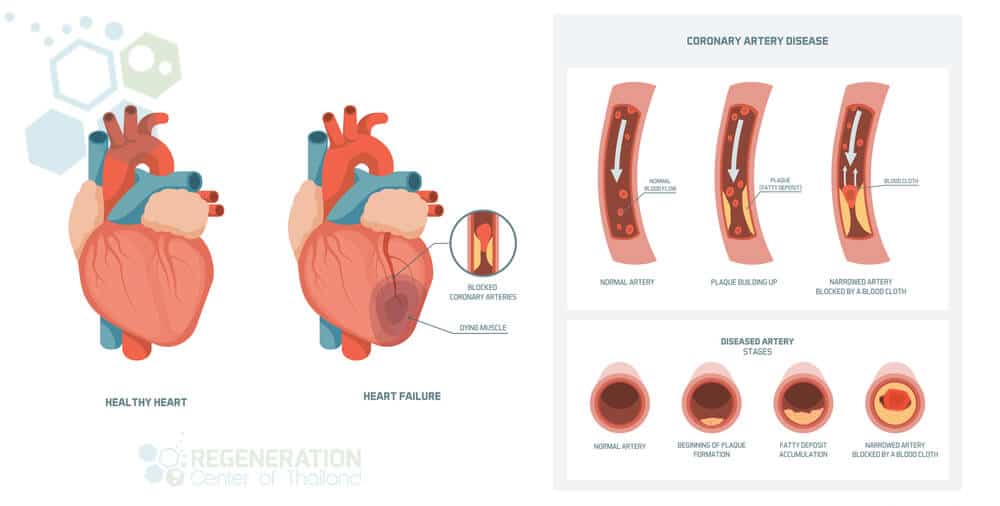
Coronary Heart Disease, or CHD, is also known as coronary artery disease, or CAD. CAD or CHD is when the coronary arteries are weakened due to plaque buildup in the blood circulatory system. The arteries are primarily responsible for providing blood and oxygen to the heart. Adult stem cell therapy for artery blockage can be a good choice for those seeking a safe, non-surgical alternative cell therapy for heart failure and many cardiac diseases, including Chronic Ischemic Arteries and Heart Failure.
Acute Coronary Syndromes – Coronary Thrombosis
- Unstable acute angina (chest pain) occurs when the heart lacks oxygen or blood flow. Symptoms vary, but most patients start occurring more frequently during periods of rest. Over time, the angina pain starts to last longer and feels more severe. Traditional treatments such as nitroglycerin may be used, but if left untreated, the issue can result in worsening heart failure.
- NSTEMI or Non-ST segment elevation myocardial infarction is a type of heart attack that may not register on an electrocardiogram (ECG). There are, however, markers in blood tests that can be used to screen for events or damage to the heart muscle. For most NSTEMI patients, the artery blockage may be temporary or partial.
- STEMI or ST-segment elevation myocardial infarction is the other type of heart attack caused by a blockage in the blood supply. STEMI events affect large areas of cardiac tissue and can be measured by an ECG test or blood panel screening for specific enzymatic activity and chemical markers. These biochemical markers in blood tests are cardiac risk markers of inflammation. The tests were developed from the earliest diagnostic markers of troponins (troponin complex) & Creatine kinase-MB (CK-MB)
Signs of Atherosclerosis & Coronary Plaque
Symptoms for patients with atherosclerosis vary for all patients. Still, new blood tests and genetic testing for hereditary heart disease can be used as an early warning sign of acute coronary syndrome.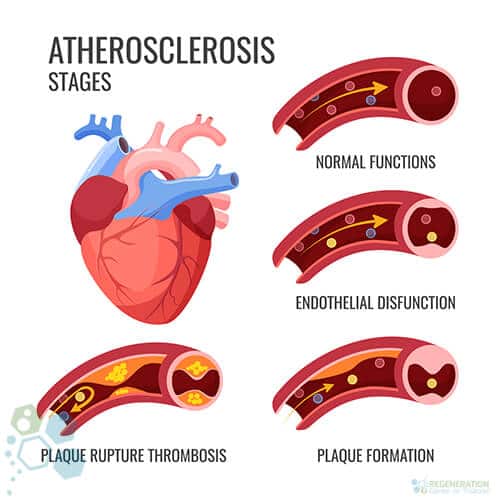
Plaque is produced because of the cholesterol, calcium, fat, and other substances found in the blood. When the plaque starts to build up in your arteries, you get diagnosed with a disease called atherosclerosis. The building up of the plaque and the inability of the heart to regenerate takes place over many years. As time passes by, the plaque narrows your arteries and thus hardens. This is the cause of the limited oxygen-rich blood in the heart.
The plague-infested region can also rupture or break open. This forms a blood clot on the surface of the plaque. When this worsens, and the blood clot becomes more prominent, this disturbs the blood flow in the main artery (coronary atherosclerosis.) Moreover, an angina heart attack or stroke might happen if your heart does not receive a regular flow of blood and fresh oxygen. Angina is a severe discomfort in the chest. It might feel like there is pressure or squeezing inside your chest. The pain might also be inside your neck, shoulders, arms, back, or jaw. Angina discomfort might even really feel like indigestion.
A heart attack happens when the regular flow of blood rich in oxygen to the section of the heart is disrupted or blocked. If this flow is not remedied immediately, the particular part of the heart will not function. Without immediate treatment, a heart attack and stroke can occur, and this may lead to death. With time, CHD will make the heart weaker, and this could result in peripheral neuropathy, arrhythmia, muscular atrophy, and often heart failure.
Heart disease is when the heart cannot pump sufficient blood required by the body. Arrhythmia has something to do with the abnormal rhythm and rate of the heartbeat.[1]
Warning signs & symptoms of heart failure
CAD, CHD, and IHD Cardiomyopathy can happen due to many reasons, including environmental conditions, lifestyle, and genes. Some common risk factors for chronic ischemic heart failure include:
- Lung diseases, COPD & Pulmonary Fibrosis
- Diabetes
- Kidney diseases PKD or Diabetic Nephropathy
- Obesity
- Viral Infections
- Hypertension
- Ischemic Strokes
- Abuse of alcohol or drugs
- Connective tissue disorders, i.e., Lupus
- Reaction to medications
- Exposure to industrial chemicals or toxins such as lead
Is Coronary Artery Disease Hereditary?
It is estimated that over 40% of all CAD cases might have some hereditary influence, and the most commonly diagnosed genetic heart diseases include:[2] 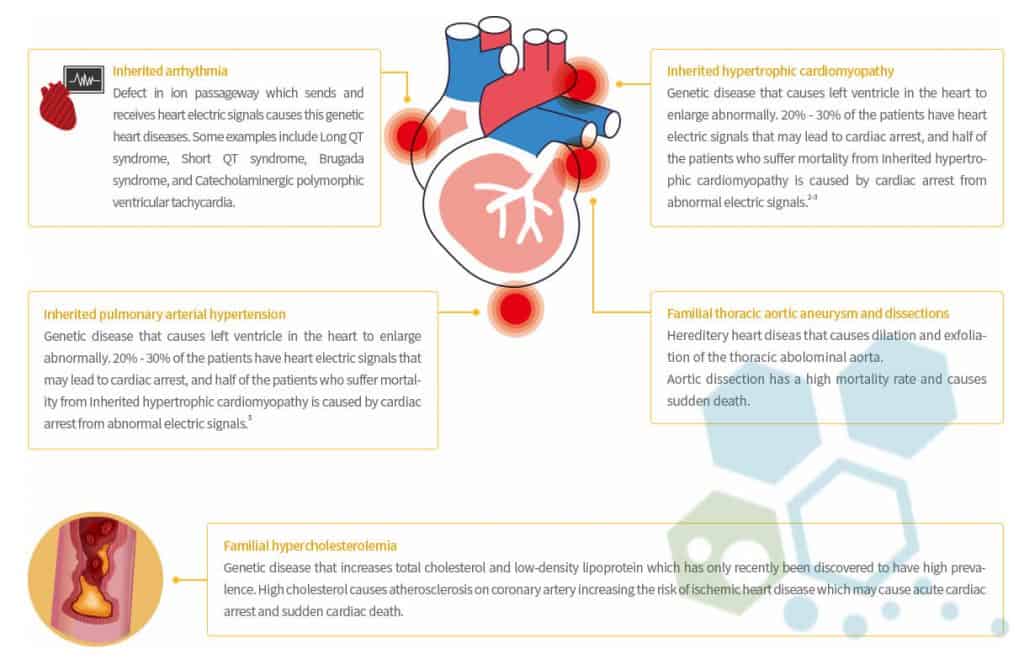
- Genetic Arrhythmia
- Hypercholesterolemia
- Pulmonary arterial hypertension
- Connective tissue disorders
- Aortopathy
- Hypertrophic Cardiomyopathy
- Hemorrhagic telangiectasia
- Congenital heart disease
- Brugada Syndrome
- Catecholaminergic polymorphic ventricular tachycardia
- Short QT Syndrome
- Long QT Syndrome
Diagnosis of Heart Disease
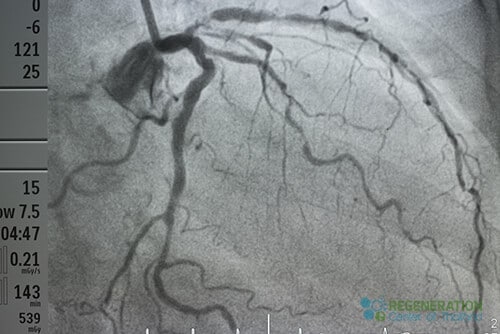
The clinical diagnosis of heart disease requires diagnostic tests and physical exams. A cardiologist uses several tests to determine the severity, including Echocardiogram, Electrocardiogram (ECG), angiograms, CT coronary angiogram, heart Stress tests (nuclear stress test), Cardiac catheterization, and blood tests. The regeneration center offers a comprehensive list of genetic panels to screen for mutations in genes that lead to hereditary heart diseases using the following panels: TNNC1, TNNI3, JUP, DOLK, TAZ, CAV3, CRYAB, CSRP3, DES, VCL, RBM20, RYR2, SCN5A, SGCD, TCAP, TMEM43, LAMP2, LMNA, MYBPC3, PKP2, PLN, PRKAG2, RAF1, EYA4, ABCC9, DSC2, DSG2, DSP, EMD, MYH7, MYL2, MYL3, ACTC1, ACTN2, GAA, GLA, HCN4, AGL, BAG3, TNNT2, TPM1, FHL1, FKRP, FKTN, FLNC, TTN, TTR, SLC22A5, CACNA1C, ANKRD1, DMD, CTNNA3, LDB3 and PDLIM3.
DNA screening tests are recommended for family members of patients who had sudden cardiac death or with low heart function. Early intervention is often crucial in managing the disease, so if the direct relatives of the deceased think they might carry an inherited disorder/gene mutation, then screening would be advised. We do not offer gene therapies to treat heart disease, but there are several clinical trials underway to cure genetic heart failure. To help reduce any risk of developing artery disease and ischemic heart disease, consider making dietary changes and getting regular exercise.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating heart disease, atherosclerosis, coronary artery disease (CAD), or ischemic heart disease (IHD) with stem cells. Patients with advanced heart failure, severe arterial blockages, recent artery bypass graft surgery, severe scarring, significant cardiovascular complications, or other major health conditions might not be good candidates for treatment.New Treatment Options for Cardiovascular Diseases
There are several methods to treat heart failure, depending on the stage, severity, and underlying cause. The first line of defense for patients with chronic heart failure and coronary atherosclerosis requires immediate lifestyle changes, medications, surgical procedures, or cardiac stem cell therapy to manage the disease. Some common medications and non-surgical treatments for coronary artery disease (CAD), CAD & IHD include:
- Antiplatelet medications (Clopidogrel)
- Beta-blockers
- Nitroglycerin
- Cholesterol-lowering medications (statins)
- Calcium channel blockers
- Percutaneous Coronary Revascularization
- Stem cell therapy for heart and cardiac cell infusions
Cardiac regeneration using mesenchymal stem cells
Stem cell therapy for heart disease is not appropriate or effective for all cases. Patients who do not respond well to medications or have reached a severe stage of cardiac disease might also require surgery or combination therapy. Depending on the severity, coronary artery disease treatments using cardiopoietic stem cells might also be an option. Cells can be delivered to the heart to restore and improve blood flow. Standard surgical procedures include:
- Open-heart surgery
- Angioplasty
- Heart transplant
- Bypass Graft surgery
- CABG: coronary artery bypass graft
- A balloon to widen an artery or deliver cells to the heart
- Artery stent
Treating Heart Disease with Stem Cells
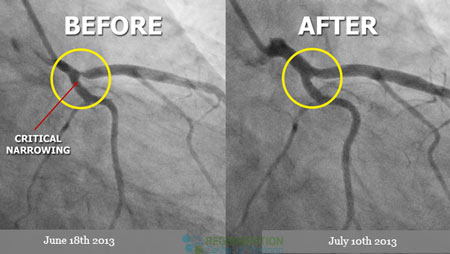
Repairing the heart using stem cells offers patients a new alternative,non-surgical treatment option to improve cardiac function and blood flow to help reverse heart disease. [3] The impact of enhanced stem cell therapies is better understood now than ever, and The Heart Regeneration Center offers a unique and effective cardiac regeneration protocol depending on patients’ needs. Cardiac stem cells can differentiate with stem cell-derived cardiomyocytes and use targeted paracrine signaling to help rebuild a patient’s heart tissue by building on top of existing stem cell research and clinical-grade hematopoietic mesenchymal stem cells. For most elderly patients or those with severe physical limitations, a combination of therapy with allogeneic cellswill be recommended. This option is only available for patients whose own cells are not sufficient or impotent due to age or other diseases.
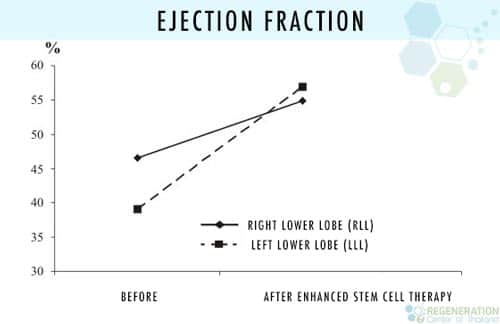
Stem cell treatment for low ejection fraction
The stem cells are immune-system compatible and expanded from cardio-sphere-derived stem cells to help assist in replenishing/replacing damaged heart cells and reverse symptoms of atherosclerosis and heart disease. [4] Cell therapy for Heart disease requires isolated cell types (differentiation of stem cells) that are cultured in our lab and then placed back into the heart generally via a process known as cell homing using multiple-stage delivery to begin reducing inflammation in the heart gradually over two weeks. Using a catheter and stem cell injections for the heart can improve heart function by targeting damaged heart tissue therapy. Umbilical cord tissue mesenchymal stem cells (UC-MSC) and bone marrow-derived mesenchymal stem cells have the potential to regenerate damaged heart tissue.
1 Year After Stem Cell Therapy for Heart Failure
The benefits and effectiveness of stem cell therapy to treat patients with advanced heart failure include: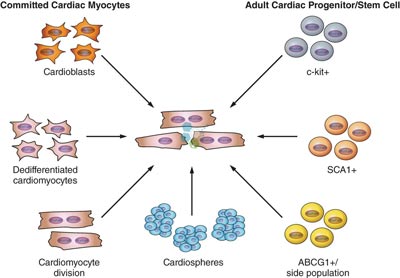
- Reduction in the infarct size / Reduction in heart muscle scar [5]
- Improved regulation of O2 (Oxygen) Intake and Use [6]
- Heart failure patients with reduced ejection fraction reported a reduction in Angina [7]
- Stem cell therapy may reduce symptoms and repair or replace damaged heart function to improve the patient’s overall well-being and quality of life.
- Long-term benefits of stem cell therapy (≥12 months) with measurable improvement in well-being & physical endurance.
- Reduction in heart muscle scar size and infarct size with reduction of cardiogenic shock via cultured heart muscle cells
- Stem cell therapy for ischemic heart may improve blood flow to the heart and reverse coronary artery calcification.
- Therapy for ischemic heart failure can help with the improvement of Left ventricular ejection fraction (LVEF), resulting in no need for re-hospitalization
Treating Cardiovascular Diseases with Cardiopoietic Cells in 2025
- Chronic Heart disease
- Artery disease treatment – CAD heart
- Congestive Heart failure
- Angina
- Thrombosis in vessel walls
- Stem Cell Therapy for Atherosclerosis & Artery atherosclerosis
- Cardiomyopathy
- Ischemic heart disease (IHD)
- MI – Heart Attack
Types of stem cells needed for cardiac regeneration
Total Number of Cardiac Stem Cell Infusions: 2-8 Infusions of Endogenous Mesenchymal Cardiomyocyte Cells & Exosome Growth Factors (per Treatment stage requirement). Multiple Stages or stem cells delivered by trans-endocardial injections may be required for severe conditions. Cell retention, engraftment, survival, and rejection risks will vary depending on the route of administration and existing patient comorbidities.
Challenges & Limitations of Heart Regeneration Therapy
Cardiac Rehabilitation Post Treatment: Cardiac Rehabilitation therapy in Bangkok is optional and can be provided for a minimum of 2 hours per day and five days per week. Medical visas and accommodations for the patient and family/friends at an extended stay service apartment or hotel can also be included upon request.
Total Time Required for CAD heart disease treatment: Estimated around two weeks in total (depending on the patient’s medical needs and total infusion of stem cells) to begin to improve heart function in patients
Stem Cell Treatment for Heart Disease
Our heart regeneration treatment protocols for artery atherosclerosis offer chronic heart failure patients a comprehensive treatment with mesenchymal stem cells and need to be performed in multiple stages to reverse coronary heart disease. For most patients, this will require the ability to travel to Thailand for the 2-3 week adjuvant therapy. Stem cell therapy in the heart is not appropriate for all patients, and due to the varying degrees/severity and other underlying medical factors, the efficacy of stem cell therapy and overall improvement in heart function will vary. Our medical team must evaluate all potential patients before providing a prognosis. Upon completion of a medical evaluation, a detailed treatment plan will be provided to the patient, including the specifics of the recommended medical protocol, the total length of stay required, and a fixed price for all related medical costs. To begin the qualification process for the Regeneration Center Heart Disease treatment, please prepare all recent medical records such as an Echocardiogram, EKG, Tilt Table Heart CT Scan, or SPECT exam (Single-photon emission computed tomography) and contact us today.
Published Clinical Citations
[1] ^ Arom, Kitipan V, Permyos Ruengsakulrach, and Vibul Jotisakulratana. 2008. Intramyocardial angiogenic cell precursor injection for cardiomyopathy in Thailand. Asian cardiovascular & thoracic annals, no. 2. https://www.ncbi.nlm.nih.gov/pubmed/18381874
[2] ^ Hou, Jingying, Lingyun Wang, Jieyu Jiang, Changqing Zhou, Tianzhu Guo, Shaoxin Zheng, and Tong Wang. 2013. Cardiac stem cells and their roles in myocardial infarction. Stem cell reviews and reports, no. 3. doi:10.1007/s12015-012-9421-4. https://www.ncbi.nlm.nih.gov/pubmed/23238707
[3] ^ Martinez, Paula F, and Marina P Okoshi. 2018. Genetic Risk in Artery Disease. Arquivos brasileiros de cardiologia, no. 1 (July 0). doi:S0066-782X2018000700062. https://www.ncbi.nlm.nih.gov/pubmed/30110045
[4] ^ Nartprayut, Kuneerat, Yaowalak U-Pratya, Pakpoom Kheolamai, Sirikul Manochantr, Methichit Chayosumrit, Surapol Issaragrisil, and Aungkura Supokawej. 2013. Cardiomyocyte differentiation of perinatally‑derived mesenchymal stem cells. Molecular medicine reports, no. 5 (March 4). doi:10.3892/mmr.2013.1356. https://www.ncbi.nlm.nih.gov/pubmed/23467912.
[5] ^ Pratumvinit, Busadee, Kanit Reesukumal, Kajohnkiart Janebodin, Nicholas Ieronimakis, and Morayma Reyes. 2013. Isolation, characterization, and transplantation of cardiac endothelial cells. BioMed research international (October 27). doi:10.1155/2013/359412. https://www.ncbi.nlm.nih.gov/pubmed/24282814
[6] ^ Varga, E, C Nemes, R P Davis, O Ujhelly, N Klincumhom, Z Polgar, S Muenthaisong, M K Pirity, and A Dinnyes. 2014. Generation of transgene-free pluripotent stem cells using an excisable lentiviral system. Experimental cell research, no. 2 (February 18). doi:10.1016/j.yexcr.2014.02.006. https://www.ncbi.nlm.nih.gov/pubmed/24560743
[7] ^ Windmolders, Severina, Astrid De Boeck, Remco Koninckx, Annick Daniëls, Olivier De Wever, Marc Bracke, Marc Hendrikx, Karen Hensen, and Jean-Luc Rummens. 2013. Mesenchymal stem cell secreted platelet derived growth factor exerts a pro-migratory effect on resident Cardiac Atrial appendage Stem Cells. Journal of molecular and cellular cardiology (December 8). doi:10.1016/j.yjmcc.2013.11.016. https://www.ncbi.nlm.nih.gov/pubmed/24326234