A recent report titled The Global Burden of Disease Study by the World Health Organization reported over 250 million new cases of COPD, and nearly 5% of all deaths around the world each year are due to this family of airway obstruction diseases. Chronic obstructive pulmonary disease (COPD) & Emphysema result in the rapid loss of lung tissue and airway obstruction due to chronic airway inflammation, resulting in progressive destruction of lung parenchyma, alveolar ducts, alveoli, and respiratory bronchioles. Using lung stem cells offers a new regenerative therapy to address the biological damage caused by chronic lower respiratory diseases. The two most common types of COPD are Pulmonary Emphysema & recurring bronchitis disease.
What is COPD?
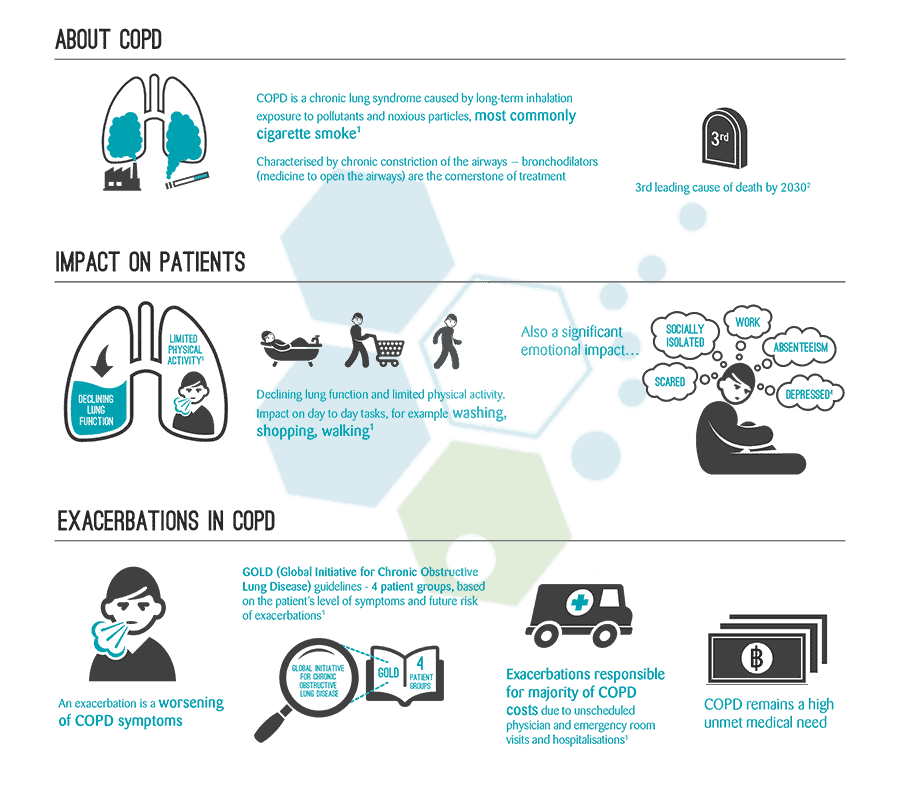
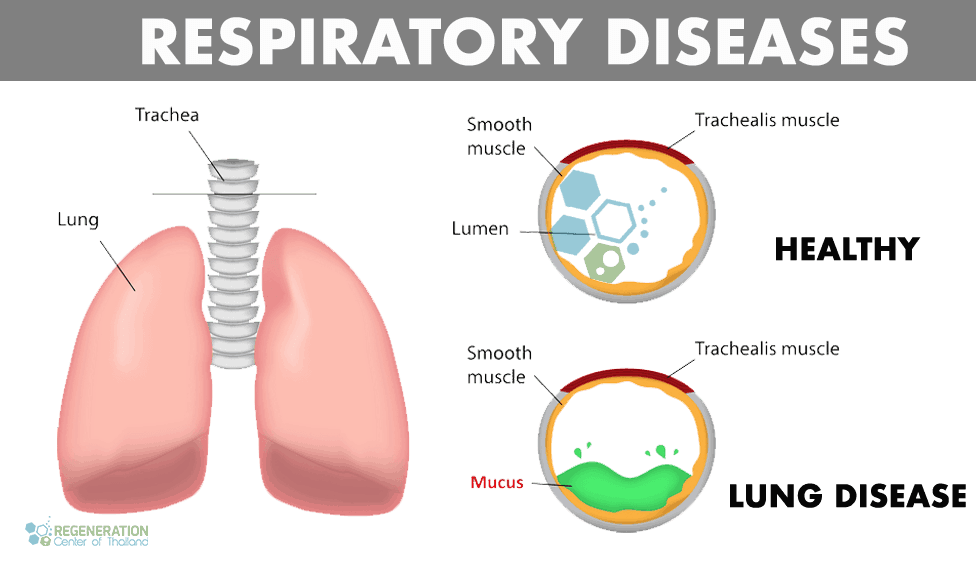
COPD is short for Chronic Obstructive Pulmonary Disease. COPD is a progressive illness that makes it very difficult to breathe correctly. “Progressive” means that the disease gets worse with time. One of the most common symptoms of this condition is heavy coughing. Coughing produces a lot of mucus (a slimy substance produced by the body), causing chest tightness, wheezing, and labored breathing. Cigarette smoking is generally regarded as one of the primary triggers for the onset of pleural mesothelioma, bronchiectasis, and Chronic Obstructive Pulmonary disorders. Still, it can also be developed as a complication from other disorders/diseases, such as lupus and systemic autoimmune diseases. Most people suffering from COPD are also usually smokers. Long-term exposure to large amounts of lung irritants such as air pollution, smoke, dust, and chemical fumes is also a significant contributor to people being diagnosed with acute lung injury. To better understand COPD, it is beneficial to know about the function of the pulmonary system and how the breathing processes occur. The air through the mouth goes straight to your windpipe, then to the bronchial tubes. Many smaller, thinner tubes branch out from the bronchial tubes called bronchioles inside your lungs.[1]
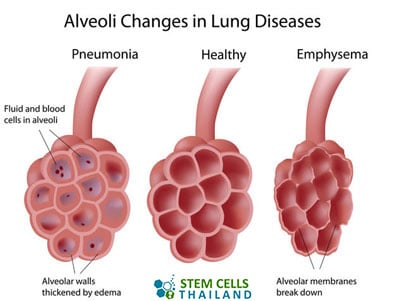
The bronchioles are directly interconnected as small round air sacs called the alveoli. The tiny blood vessels known as capillaries run inside the walls of the alveoli. As soon as air goes to the alveoli, the oxygen in the air goes through the walls of the air-filled spaces and then into the blood through the capillaries. At the same time, carbon dioxide waste gas goes into the alveoli sacs from the capillaries. This procedure is known as gas exchange.[2]
The alveoli and the airways are pretty flexible and elastic by nature. Every time you breathe, the alveoli sacs fill up like little balloons. Whenever you breathe out, the opposite happens: the air-filled spaces then deflate, and air goes out.
The Function of the Respiratory Tract
All cells in the human body require a consistent stream of fresh oxygen to stay alive. The respiratory system is responsible for delivering oxygen to all the cells in the human body while also removing the waste product of carbon dioxide, which can be lethally accumulated in excess. Several parts comprise the respiratory system, including the airway, voice box, windpipe, and respiratory tract. The airway consists of the nose, larynx, pharynx, bronchi, mouth, bronchioles, and trachea. The airways are usually divided into upper and lower respiratory tracts. After the trachea, the airways divide into an ever smaller bronchial tree (bronchi), and at the end of which tree are where the individual alveoli sacs are located.
Symptoms of COPD
The causes of COPD are numerous, but for many onset cases of COPD, the patient may not display indications. As the disease progresses, signs and complications become much more articulated. The most common signs & indications for COPD diagnosis are:
- “Smoker cough” which is another name for a persistent cough or coughing that produces a lot of excess mucus
- Labored Breathing: This mainly occurs during physical stress, such as playing sports or climbing stairs
- Strange sounds while breathing: A dry, squeaky, whistling, or wheezing sound when exhaling can indicate early-stage COPD
- Frequent tightness in the chest area is an early warning sign of chronic inflammatory COPD
- A persistent cough occurs primarily in the morning due to airway inflammation or being blocked with thick, viscous mucus
Although many COPD patients notice such complaints, they do not take them seriously. Coughing is usually the first symptom but is initially not noticed or very alarming for most. People who are not very physically active may only recognize COPD when it has reached an advanced stage where breathing is difficult, even at times of rest. Researchers have also found that many heavy smokers may already have COPD but might not feel any manifestations until it’s confirmed with a lung function test. Having COPD can also damage your body’s defense mechanisms, resulting in frequent colds or other respiratory-related infections, including influenza.
Advanced Signs of Pulmonary Diseases
The severity of a patient’s indications depends entirely on how much lung damage a person has. Patients who keep smoking will cause (lung fibrosis) and damage to the lung tissue much faster than those who stopped smoking. Intractable signs of end-stage COPD may cause swelling in the feet area, ankles, and legs and result in rapid weight loss reduction in overall muscle endurance that can result in injuries to the hips & knees.
COPD Management Guidelines
The disease develops slowly. However, there are always phases in which the signs suddenly worsen, especially for patients with COPD with acute exacerbations. The trigger is then usually a respiratory tract infection, and these exacerbations significantly accelerate the progression of chronic inflammatory COPD. Over time, COPD exacerbations increase, and reduction in lung capacity/lung function can also increase the risk of other diseases such as Spondyloarthropathy, rheumatoid arthritis, Parkinsons, ataxia, and brain strokes.
What is Emphysema?
Pulmonary Emphysema is part of a family of lung diseases called COPD. Emphysema is a chronic pulmonary disease that is diagnosed after critical damage (permanently dilated or destroyed) to the 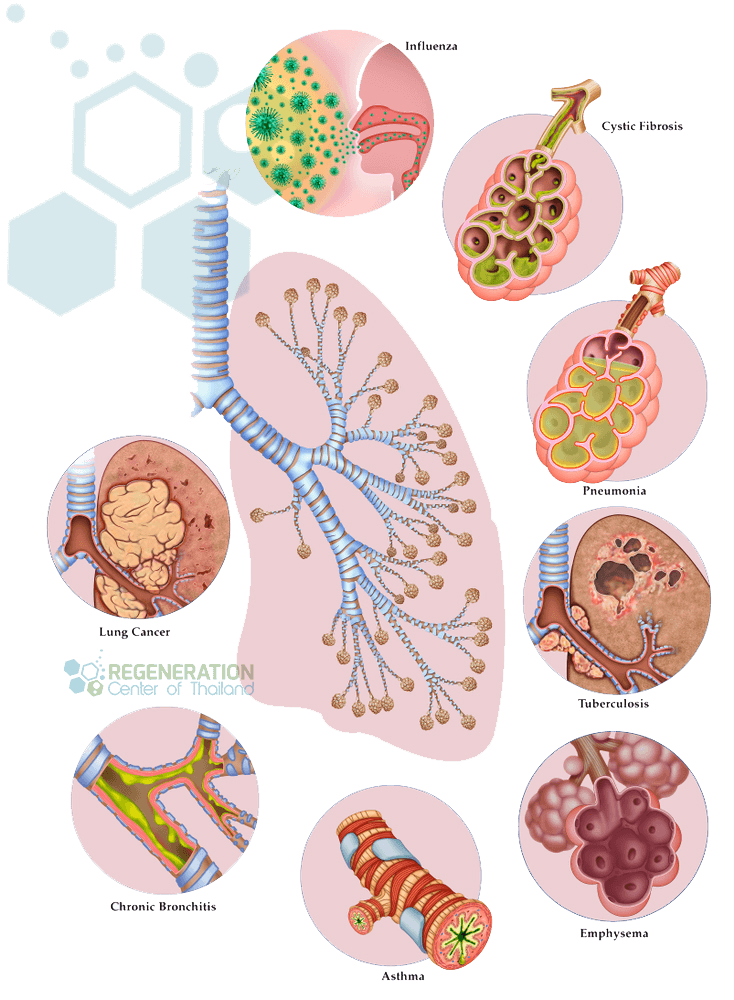 alveoli. These over-inflated lung sections retain “old” air in the air sacs, so less “fresh” atmosphere can be absorbed. Overinflation of the alveoli increases during physical exertion and is the leading cause of winded breathing. The damage to the alveoli can be done in several ways, including:
alveoli. These over-inflated lung sections retain “old” air in the air sacs, so less “fresh” atmosphere can be absorbed. Overinflation of the alveoli increases during physical exertion and is the leading cause of winded breathing. The damage to the alveoli can be done in several ways, including:
- Destroyed
- Overinflated
- Stretched
- Narrowed
Over-inflation of the alveoli results from a breakdown of the walls of the air sacs, which causes a decrease in respiratory health and frequent breathlessness. Any damage to the air sacs reduces the inner surface of the alveoli, which are critical for the gas exchange between air and blood. The reduction in cell mass results in an increasing decline of oxygen in the blood and vital organs, which can lead to peripheral neuropathy, CHF, pulmonary hypertension, and heart attacks. Damage to the alveoli sacs can be challenging to manage using traditional medications as the chronic inflammation creates permanent holes in the lower lung tissue. Persistent coughing and sputum are other common manifestations of concomitant inflammation (bronchitis).
Some Common Risk Factors and Causes of Pulmonary Emphysema include:
- Smoking
- COPD
- Recurrent respiratory infections such as bronchitis, asthma, and pneumonia
- Environmental Pollutants such as coal, cadmium, grains, and isocyanates
- automobile exhaust gases or specks of dust and gases found in the workplace
- Mineral dust & cotton dust are also COPD risk factors
- Hereditary predispositions such as Alpha-1-antitrypsin deficiency ( α1-antitrypsin ), a deficiency of a protective protein (protease inhibitor, PI). The condition is genetic and causes the body to produce too little alpha-1-antitrypsin (AAT), resulting in an AAT deficiency.
The Four Stages of COPD
| Stage of Pulmonary Disease | FEV1/FVC – Tiffeneau-Pinelli Index |
| Stage I = Mild | More than or equal to 80% |
| Stage II = Moderate | Less than 80%, More than 50% |
| Stage III – Severe | Less Than 50%, More than 30% |
| Stage IV – Very Severe | Less than 30%, Less than 50% Respiratory Failure |
Diagnosing COPD & Emphysema
Diffuse parenchymal lung disease (DPLD) and Emphysema are types of chronic obstructive pulmonary disease that display abnormal and permanently enlarged in the terminal bronchioles of the lungs. Emphysema and dyspnea usually occur in patients with bronchitis and obstructive pulmonary and respiratory problems. It is rare for patients to be diagnosed with pure Emphysema ( without displaying other indications ) unless it’s related to COPD due to hereditary/genetic abnormalities. Most patients we treat at the Lung Regen Center have a combination of bronchitis, emphysematous lungs, or cardiometabolic diseases caused by airway impairment. This combination of dyspnea is casually referred to as COPD or COLD (chronic obstructive lung disease).
There are three primary types of Emphysema, including:
- Centriacinar emphysema begins in the patient’s respiratory bronchioles and then starts to spread in the upper half area of the lungs. This type of Emphysema is usually caused by long-term tobacco/cigarette smoking.
- Panacinar emphysema is primarily found in the lower regions of the pulmonary system and tends to destroy the alveolar tissue that causes wheezing. This type of lung disease is commonly found in patients displaying an antitrypsin deficiency with alpha-1 antitrypsin and is a genetic/hereditary disease often seen in patients with end-stage Emphysema.
- Paraseptal Emphysema occurs in and around the pleura or septae. This type of disease is mainly associated with chronic autoinflammatory conditions that arise after a lung infection or dyspnea
Genetic Testing for Lung Disease & Pulmonary Cancers
The Lung Regeneration Center offers DNA screenings for mutated genes that lead to lung diseases, including:
- FLCN gene, which is associated with Birt-Hogg-Dubé syndrome (pulmonary cysts)
- TSC1 TSC2 genes, which are associated with TSC (tuberous sclerosis complex) and lung tumors
- COPA genes which are associated with autosomal dominant interstitial disease (autoimmune)
- PGM3, SPINK5, DOCK8, STAT3 genes associated with Hyper IgE syndrome, an immunodeficiency that causes frequent lung infections
- EGFR gene, which is associated with autosomal dominant genetic squamous cell lung carcinoma
- MARS gene, which is associated with autosomal dominant Charcot-Marie-Tooth disease and autosomal recessive interstitial disease
Genetic screening of pulmonary illnesses is recommended for family members of patients with a family history of lung diseases or cancers or as a tool to confirm an existing diagnosis. Early intervention key for managing Pulmonary diseases. We do not offer lung transplantation or gene therapies to treat pulmonary disease, but there are several Phase 1 clinical trials underway with the hopes of one day curing COPD completely.[3] To help reduce any risk of developing COPD, emphysematous lungs, and pulmonary hypertension, consider making lifestyle changes and getting regular exercise.
Latest Treatment Options COPD
Therapeutic options for chronic pulmonary infections and COPD vary from patient to patient, depending on severity. Still, they can help ease some signs, prevent further complications, and gradually slow the progression of the disease using a variety of methods, starting with smoking cessation.
Medications for COPD – Some medications can help to reduce indications of chronic COPD and reduce frequent exacerbations & flare-ups. Unfortunately, the effectiveness of medicines differs for different patients, so your pulmonary specialists might recommend several options to reduce inflammation, relax the airway muscles, or widen the airways to help you breathe more easily. Some common COPD medications include:
- Theophylline is generally the first clinical option for COPD patients to help prevent flare-ups and ease dyspnea and chest tightness. Taken in pill form, this older medication is known to cause side effects.
- Bronchodilator medications are delivered through a nebulizer or inhaler to loosen the tight muscles of your airways. There are two types of Bronchodilators, including anticholinergics and selective beta-2-agonist, and they are often used as a COPD exacerbation treatment.
- Glucocorticosteroids to help reduce inflammation in the airways can be taken in pill form or inhaled via nebulizer.
- Phosphodiesterase-4 inhibitors can be taken as a pill to relax the airway path and help reduce inflammation. They are generally reserved for patients with late-stage COPD or chronic bronchitis.
- Antibiotics and antivirals to fight some respiratory infections. Vaccines for COPD Bronchitis, such as pneumococcal vaccination ( PNEUMOVAX 23 ), can also be given to high-risk patients to help reduce the risk of getting respiratory infections or for protection from getting whooping cough (pertussis)
Oxygen therapy for Chronic Obstructive Pulmonary Disease – Supplemental oxygen is prescribed for patients with low blood oxygen levels. It can be taken via a nasal cannula or a mask to help patients breathe better. A portable oxygen unit is sometimes needed to allow patients to get around more easily.
Surgeries for COPD – Surgeries are usually reserved for severe cases of COPD, often as a last resort when other clinical options have failed. Surgery is more commonly used for cases of severe Emphysema. One such type of lung surgery is known as a bullectomy. Large, abnormal bullae (air spaces) are removed during a bullectomy surgery. Another type of surgery is lung volume reduction, which is used to surgically remove injured areas in the upper lung tissue. The riskiest and most challenging treatment option is lung transplants, where new lungs totally or partially replace a patient’s damaged organ from a living or deceased donor.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating COPD, Emphysema, lung fibrosis, or bronchiectasis with stem cells. Patients with advanced lung disease, severe respiratory impairment, significant comorbidities, or other critical health conditions might not be good candidates for treatment.Stem Cell Therapy for COPD
 Patients having clinical intervention at the Lung Regeneration Center have usually already tried a wide range of COPD trials with various levels of success or failure. Patients seeking a more modern approach, such as stem cell therapeutics for COPD, have tried other medical options first but often find it challenging to deal with the severe side effects or positive long-term results. Lung stem cell transplants offer patients a safe alternative that can help repair the air sacs and diseased tubes inside the lungs with healthy lung tissue. Lung regeneration is a gradual process, but once the damaged areas get repaired, the indications slowly begin to disappear, lung capacity increases, and patients can breathe more freely. With COPD, there is much less airflow in and out of the airways, resulting in frequent exacerbations. Restrictive chronic airway obstruction symptoms are due to one or more of the following reasons:
Patients having clinical intervention at the Lung Regeneration Center have usually already tried a wide range of COPD trials with various levels of success or failure. Patients seeking a more modern approach, such as stem cell therapeutics for COPD, have tried other medical options first but often find it challenging to deal with the severe side effects or positive long-term results. Lung stem cell transplants offer patients a safe alternative that can help repair the air sacs and diseased tubes inside the lungs with healthy lung tissue. Lung regeneration is a gradual process, but once the damaged areas get repaired, the indications slowly begin to disappear, lung capacity increases, and patients can breathe more freely. With COPD, there is much less airflow in and out of the airways, resulting in frequent exacerbations. Restrictive chronic airway obstruction symptoms are due to one or more of the following reasons:
- Due to an underlying medical condition, airways and sacs shed their elastic abilities.
- The walls between the alveoli are diseased or destroyed
- The walls inside the airways become inflamed and too thick for gas exchange
- Too much mucus is produced by the airways, which cause it to clog the airways
Repair & Restore Lung Function
On the basic level, Stem cells are recognized as the building blocks of biology due to their incredible regenerative properties. These totipotent cells offer a promising therapeutic approach using natural sources of cells in human tissue and blood cells. In COPD Stem Cell Treatments, the destroyed lung tissues and cells, causing various complications, are targeted for regenerating signaling pathways needed for lung repair. Recent studies have also shown that patients with airway inflammation diseases, such as COPD, have a higher prevalence of inflammatory bowel diseases, such as ulcerative colitis and Crohn’s disease.
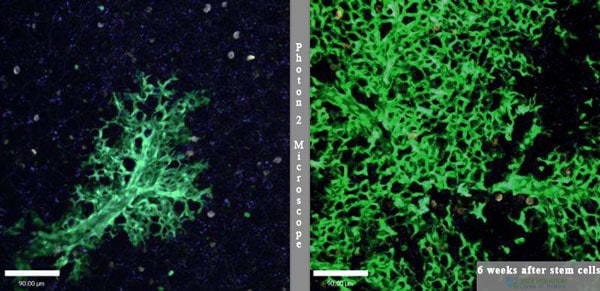
Treatment for Emphysema
Using isolated and enhanced mesenchymal stem cells (MSC+) allows us to target specific regions of the lung structure to slow/stop the spread of the disease, eliminate bronchitis, and reduce inflammation (in the alveoli pathway.) Improvements in the pulmonary system occur through a function known as immunomodulation, which makes it a powerful but safe and natural therapy for COPD. The goal of the Regeneration Center therapies for COPD and other pulmonary diseases such as Idiopathic Pulmonary Fibrosis (IPF), Bronchiectasis, Atelectasis, and Emphysema is to help create the optimal environment for angiogenesis to build new capillaries plus reduce inflammation in the lungs which lead to tissue repair and improved lung function.[4]
Natural Way to Stop Chronic Airway Obstruction
Interstitial lung diseases pose a significant challenge for pulmonologists and lung bioengineering. Diseases such as asthma, pulmonary fibrosis, lung cancer, COPD, Cystic fibrosis, Emphysema, Atelectasis & hyaline membrane disease are just some of the diseases that can be managed effectively via lung stem cell therapies. Due to the complexity and locations of the diseased regions, it has always been challenging to deliver cell therapeutic agents effectively. The Regeneration Center has developed a unique and effective protocol using a combination delivery method to target diseased or damaged lung tissue. Our lung therapy uses multiple vectors for cell delivery, including Intravenous, direct injection, and endotracheal transplants. Our proprietary Intranasal delivery method (mesenchymal stem cell nebulizer) is available for painless and targeted delivery of endogenous lung progenitor cells and lung epithelial stem cells to both the airway and vascular system to organize better pulmonary structures for functional improvements of Lung parenchymal damage.[5]
Is Lung Cellular Regeneration the Best Treatment for COPD?
Lung Cell Transplant – Requirements
 Total Clinical Sessions For COPD & Emphysema will depend on patient needs. End-stage COPD options are limited, and Exogenous Pulmonary mesenchymal Stem Cells (MSC+) are ideal for mild to moderate pulmonary diseases. The therapeutic approach will include combination therapy of endogenous lung epithelial cells, lung progenitor cells, airway progenitor cells, and pulmonary alveolar epithelial cells (for tracheal regeneration) delivered in multiple stages over a 2-week course. Long-term effects depend on the severity of the existing condition, and candidates with progressive respiratory diseases, end-stage COPD, bullous lung disease, Popcorn Lung (Bronchiolitis Obliterans) disease, other COPD complications, chronic respiratory system inflammation, and structural alveolar degeneration may not be good candidates depending on the severity of airflow obstruction. [6]
Total Clinical Sessions For COPD & Emphysema will depend on patient needs. End-stage COPD options are limited, and Exogenous Pulmonary mesenchymal Stem Cells (MSC+) are ideal for mild to moderate pulmonary diseases. The therapeutic approach will include combination therapy of endogenous lung epithelial cells, lung progenitor cells, airway progenitor cells, and pulmonary alveolar epithelial cells (for tracheal regeneration) delivered in multiple stages over a 2-week course. Long-term effects depend on the severity of the existing condition, and candidates with progressive respiratory diseases, end-stage COPD, bullous lung disease, Popcorn Lung (Bronchiolitis Obliterans) disease, other COPD complications, chronic respiratory system inflammation, and structural alveolar degeneration may not be good candidates depending on the severity of airflow obstruction. [6]
Pulmonary Rehabilitation After Therapy (Optional): Pulmonary Rehabilitation and breathing exercises for COPD are strongly recommended and are available at affiliated local hospitals in Bangkok, depending on the patient’s travel limitations and timing constraints. A dedicated lung rehabilitation specialist will be available upon request for 2-5 hours per day and up to 6 days per week. Medical visas and accommodations for an extended stay with an oxygen nebulizer for the patient can also be provided upon special request.
Total Treatment Length: The Lung Regeneration Center protocol is an outpatient procedure but will require multiple stages of over two weeks of therapy in Bangkok (depending on the severity/spread of the underlying disease).
COPD Treatment Benefits & Guidelines
Due to the varying degrees of lung damage, our medical team must review patients’ preclinical and clinical records to understand their needs better. Learn more about COPD clinical trials around the world. To get more information about lung cell therapy or to begin the COPD lung stem cells review process, please prepare your recent pulmonary tests and medical records (MRI or Chest CT Scans) and contact us today.
2025 Guidelines for Treating COPD & Emphysema
The total number of pulmonary stem cell infusions will depend on the severity of restrictive lung disease, and multiple stages may be necessary for patients with scarring on the lung tissue or diffuse parenchymal complications. For optimal results, the Regeneration Center uses a proprietary method of cell delivery that achieves 40% better results than just IV infusions. Due to the progressive nature of lung diseases, some patients may require allogeneic UC-MSC+ cells. Patients with honeycombing, severe respiratory damage, or multiple comorbidities may require multiple infusions.
Lung Rehabilitation after Pulmonary Stem Cell Therapy
Post-Treatment Lung Rehabilitation: Pulmonary rehabilitation services are optional but are highly recommended after any treatment. For patients with the option to stay in Thailand, we offer a complete integrative rehabilitation program in partnership with local hospitals in Bangkok. Pulmonary rehabilitation is also beneficial for patients experiencing severe difficulty in breathing or severe hardening of the lungs. Smoking is also much discouraged for patients with this condition, and active smokers will not qualify for our treatment. The rehabilitation packages in Bangkok are available to all candidates as needed (2-5 hours per day, six days per week). Medical treatment visas and hotel accommodations for long-term stays can also be provided upon request.
Due to varying degrees of respiratory diseases, our medical team must review patients’ medical files for approval. The medical review can be done online or in person. Suitable candidates will be required to stay a minimum of two weeks in Bangkok. To begin the qualification process, please prepare your recent pulmonary tests, such as spirometry exams, lung function tests, and radiology scans from an MRI or (HRCT) High-Resolution Chest Scans, and contact us today.
Published Clinical Citations
[1] ^ Al-Jamal, R, W A H Wallace, and D J Harrison. 2005. Gene therapy for chronic obstructive pulmonary disease: twilight or triumph? Expert opinion on biological therapy, no. 3. https://www.ncbi.nlm.nih.gov/pubmed/15833071
[2] ^ Antonucci, Ivana, Andrea Pantalone, Stefano Tete, Vincenzo Salini, Cesar V Borlongan, David Hess, and Liborio Stuppia. 2012. Amniotic fluid stem cells: a promising therapeutic resource for cell-based regenerative therapy. Current pharmaceutical design, no. 13. https://www.ncbi.nlm.nih.gov/pubmed/22352751
[3] ^ Jin, Zhixian, Xinghua Pan, Kaihua Zhou, Hong Bi, Liyan Wang, Lu Yu, and Qing Wang. 2015. Biological effects and mechanisms of action of mesenchymal stem cell therapy in chronic obstructive pulmonary disease. The Journal of international medical research, no. 3 (April 1). doi:10.1177/0300060514568733. https://www.ncbi.nlm.nih.gov/pubmed/25834280
[4] ^ Lim, Sam, David Chi-Leung Lam, Abdul Razak Muttalif, Faisal Yunus, Somkiat Wongtim, Le Thi Tuyet Lan, Vikram Shetty, et al. 2015. The impact of chronic obstructive pulmonary disease (COPD) in Thailand and the Asia-Pacific region is the EPIC Asia population-based survey. Asia Pacific Family Medicine, no. 1 (April 23). doi:10.1186/s12930-015-0020-9. https://www.ncbi.nlm.nih.gov/pubmed/25937817
[5] ^ Mora, Ana L, and Mauricio Rojas. 2013. Adult stem cells for chronic lung diseases. Respirology (Carlton, Vic.), no. 7. doi:10.1111/resp.12112. https://www.ncbi.nlm.nih.gov/pubmed/23648014
[6] ^ Akram, Khondoker M, Neil Patel, Monica A Spiteri, and Nicholas R Forsyth. 2016. Lung Regeneration: Endogenous and Exogenous Stem Cell-Mediated Therapeutic Approaches. International Journal of molecular sciences, no. 1 (January 19). doi:10.3390/ijms17010128. https://www.ncbi.nlm.nih.gov/pubmed/267607