It keeps us upright, helps us carry much weight, and is equally flexible and stable. The human spine is an anatomical marvel that consists of millions of nerves that connect our brain to all nerves in the body. The spine is a highway for sending messages between the mind and body. Our spinal cord is protected by vertebrae bones that form the spine’s shape. Even a slight injury, loss of disc height, or degeneration of the back vertebrae or surrounding tissues can result in severe back pain.
 What is DDD?
What is DDD?
DDD, or Degenerative disc disease, is an age-related medical condition diagnosed when one or more intervertebral discs (discs between the spinal column’s vertebrae) break down or deteriorate. Lower lumbar disc disease is often painful and can significantly impact a patient’s quality of life. Disc degeneration is a normal part of the aging process, and for many senior individuals, DDD isn’t an issue. For others, however, a degenerated disc may cause severe pain and chronic discomfort in the knee joints, back, hip joint, shoulder joint, and neck areas.
Cause of Spinal Disk Deterioration
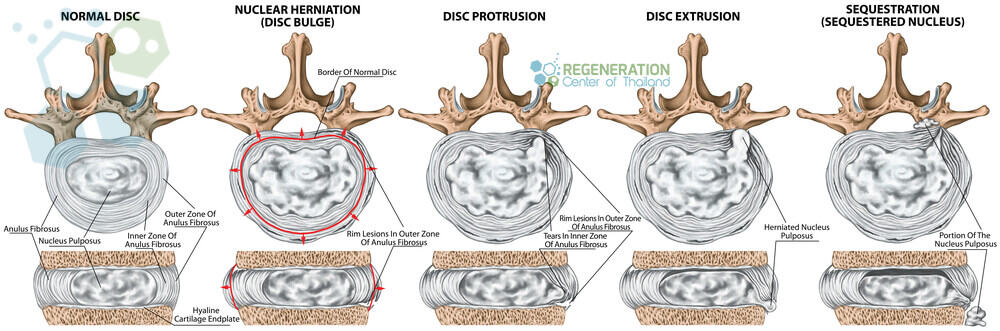
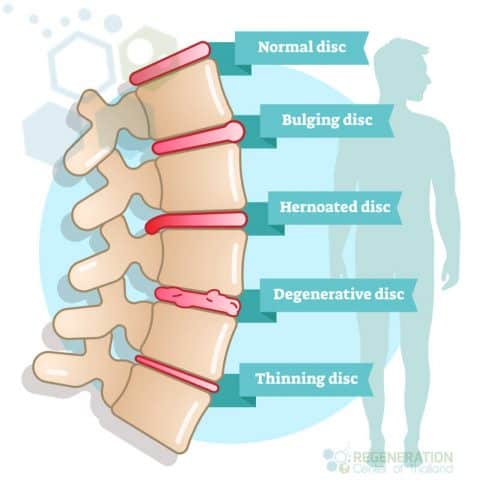
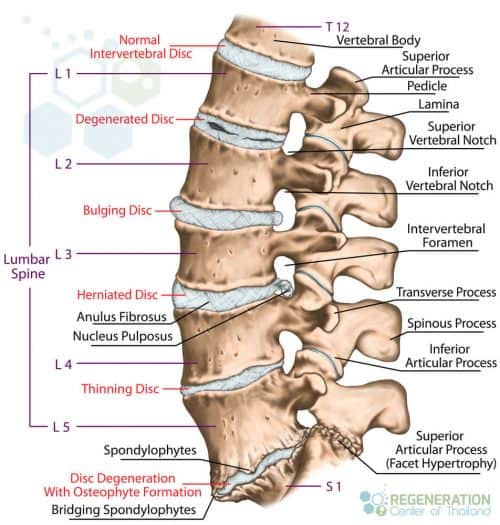
Degeneration of the spinal discs can happen for a variety of reasons. Simple events like walking, carrying heavy loads, repetitive movements, and shock-playing sports cause micro-injuries to our spinal column day after day. Often, these events go unnoticed, thanks to the vertebrae that act as shock absorbers. Every time the shock absorbers get used, a tiny amount of synovial fluid gets released to help “lubricate” the joints. During the sleep cycle, the discs can rebound to the initial stage. Still, over time, damage to chondrocytes and synovial cells from stress and inflammation causes this mechanism to lose effectiveness. This damage, over time, leads to asymmetric joint space narrowing, osteophytes, subchondral sclerosis, and cyst formations. A healthy spinal disc comprises a few parts, including the nucleus pulposus at the center of the spine and surrounded by the annulus fibrosus, a fibrous ring. The center nucleus pulposus area is a very soft, jelly-like, well-hydrated substance. Over time and with constant wear and tear, the nucleus pulposus (NP) begins to get stiff and dehydrated. This dehydration leads to a reduction in disc height & disc space narrowing, which causes excess stress on the annulus fibrosis. This stress damages the annulus, resulting in instability of posture and back pain. Such a scenario is diagnosed as intervertebral disc degeneration or DDD.
Spinal Lumbar Degeneration
This spinal degeneration disease occurs slowly and gradually. Still, it is often felt first in the lumbar spine region because they are exposed to heavier loads more often than the discs in the neck (cervical spine) region. The spinal degeneration of intervertebral discs between the ( L5-S1) lumbar vertebra L5 and the lumbosacral segment S1 are most frequently affected. With symptomatic degenerative disc failure, chronic lower back pain radiates towards the hips, or often, there is a discomfort within the buttocks or thighs while walking; other symptoms, such as sporadic tingling or weakness in the knees might also be evident. Physical pain or discomfort might also be felt while bending, sitting, lifting, and twisting.
Cervical Spine & Neck Pain
Chronic neck pain may also affect the upper spine. Patients often report discomfort or pain radiating to the arms, hands, wrists, and shoulders. The patients’ distress in the neck may interrupt healthy blood flow to the brain, consequently affecting memory and other cognitive skills. This interruption in the blood flow might also trigger headaches and vertigo.
Types of DDD – Discogenic Pain
Its location and stage of deterioration typically describe the severity of DDD:
- Cervical Disc Disease: This kind of DDD happens in the neck (cervical spine) region of the spine
- Thoracic Disc Disease: This type of DDD happens in the middle-back area of the spine
- Lumbar Disc Disease: This type of DDD degeneration in the lower back region of the spine.
Any back-related pain that is associated with intervertebral disc disruptions is referred to as “discogenic” pain. Depending on the severity of the disc bulge, the pain can be mild or very sharp. Some patients report feelings of lancinating, stabbing, or burning sensations, while others commonly report frequent numbness and tingling in extremities.
4 Stages of Degenerative Disc Disease
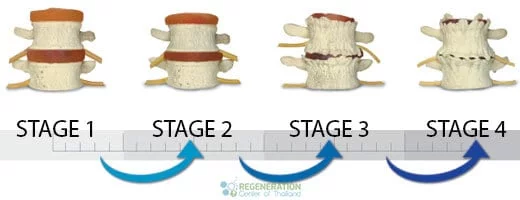
- Stage 1 of Degenerative Disc Disease is the very first sign of disk deterioration in the spine. In Stage 1, there may be damage to the shape/curvature of the spine, which affects posture. Surrounding nerves and joints are frequently inflamed due to stress and begin to age rapidly. Despite the slight loss of disc height, some patients experience very little pain or overall discomfort.
- Stage 2 Degenerative Disc Disease occurs once the condition worsens, disc space narrows, and bone spurs (bone deformations) start to appear. The changes in a patient’s posture become more apparent, and disc desiccation and narrowing have begun. Stage two patients often report frequent discomfort and pain.
- Stage 3 of Degenerative Disc Disease is when the condition has reached advanced stages with multilevel disc desiccation, apparent changes in posture, disc thinning, damage to surrounding nerves, bone spurs, and formation of scar tissue due to constant inflammation. For most patients, this stage results in significant deterioration of the physical condition and chronic pain, resulting in additional mental stress.
- Stage 4 of Degenerative Disc Disease is the most severe form of subluxation degeneration or diffuse disc bulges and is sometimes not treatable even with stem cells. At this late stage, the damage to the spine can be severe, with virtually no disc height ( bone on bone), reduction in flexibility, chronic back pain, damage to the femoral nerves and root nerves, a fusion of bones resulting in additional scar tissue, and minimal abilities.
Herniated Spinal Discs
A herniated disc is also known as a bulged, slipped, or ruptured disc. This type of DDD occurs when the nucleus of a disc is pushed out of the center annulus into the spinal canal. This is typically caused by a rupture or tear rupture in the annulus ( fibrous ring), which causes pressure on the surrounding nerves and results in pain. About 90 percent of all cases of herniated disc failure occur in the lumbar spine region (lumbar disc herniation) but can also affect the thoracic spine (thoracolumbar) or sacrum (lumbosacral areas) of the spine. Risk factors that can increase the risk of having a herniated disk include Excess body weight, causing stress on the lower back discs. People with very physically demanding jobs also have a much higher risk of getting back problems. Unbalanced repetitive motions involving lifting, pushing, twisting, pulling, and bending sideways can also increase the risk of getting herniated disks. Genetics plays a part for some as people can inherit mutated genes that increase the risk of developing herniated discs.
Diagnosing DDD & Back Pain
To diagnose DDD and cervical degenerative disc disease, an orthopedic doctor examines the patient’s medical history and performs a physical examination. An MRI scan is often needed to identify areas of damage, but for patients
 unable to have MRI Scans, a computed tomography (CT) scan can be used to identify vacuum phenomena, slippage of discs, cracks/defects in the bone structure, or damage to soft tissue structures inside the spine. Our functional medical team can also use Radiology scans to help identify spondylolisthesis (slippage) in surrounding discs. Patients can be graded and offered treatment depending on the scale and severity of the vertebra degeneration. The Regeneration Center also offers in-person evaluations to assess the patient’s range of motion, posture, and spine alignment. In some severe cases, a Discography test may determine if a specific disc is the source of pain. It involves injecting contrast dye into the disc and observing the response. Additionally, reflexes, muscle strength, and sensation are tested, particularly in the arms (for Cervical DDD) or legs (for lumbar DDD), to detect nerve root compression or irritation. Radiology scans are needed to observe the patient’s posture and spine alignment to identify abnormalities, as some severe cases of Cervical DDD can lead to spinal cord compression, causing symptoms like difficulty with coordination, balance issues, or changes in bladder/bowel control. A detailed differential diagnosis is often needed to differentiate DDD and Cervical DDD from other conditions like herniated discs, spinal stenosis, or spondylolisthesis, which may present with similar symptoms.
unable to have MRI Scans, a computed tomography (CT) scan can be used to identify vacuum phenomena, slippage of discs, cracks/defects in the bone structure, or damage to soft tissue structures inside the spine. Our functional medical team can also use Radiology scans to help identify spondylolisthesis (slippage) in surrounding discs. Patients can be graded and offered treatment depending on the scale and severity of the vertebra degeneration. The Regeneration Center also offers in-person evaluations to assess the patient’s range of motion, posture, and spine alignment. In some severe cases, a Discography test may determine if a specific disc is the source of pain. It involves injecting contrast dye into the disc and observing the response. Additionally, reflexes, muscle strength, and sensation are tested, particularly in the arms (for Cervical DDD) or legs (for lumbar DDD), to detect nerve root compression or irritation. Radiology scans are needed to observe the patient’s posture and spine alignment to identify abnormalities, as some severe cases of Cervical DDD can lead to spinal cord compression, causing symptoms like difficulty with coordination, balance issues, or changes in bladder/bowel control. A detailed differential diagnosis is often needed to differentiate DDD and Cervical DDD from other conditions like herniated discs, spinal stenosis, or spondylolisthesis, which may present with similar symptoms.
Treatment for Multilevel Degenerative Disc Disease
For the early stage of DDD or to manage the initial pain of degenerative discs, a combination of treatments is available, including:
- Over-the-counter pain medications & muscle relaxants can help treat temporary acute pain. Over long-term use, these medications can cause serious side effects or be addictive, so they must be used with extreme caution and sporadically as needed.
- Ice and Heat compression can improve blood circulation, which can help reduce tension muscle spasms and improve mobility.
- Massage therapy can help to reduce muscle spasms and stress in the low lumbar region. Thai massages are often used to reduce inflammation and pressure on the spine, which can relieve pain.
- Epidural steroid injections can be administered to reduce pain signals and inflammation. EDI injections are a temporary solution that can be injected directly into the space surrounding the spine
Treatment for Spinal Stenosis & Disc Space Narrowing
Surgery vs Stem cells for back pain & DDD
Surgical treatment of DDD is another option for mild to severe degenerative disc disease but is usually recommended if nonsurgical therapies are ineffective. Surgery for Degenerative Disc Disease can result in additional complications ( failed surgery) or irreversible damage along with extended recovery periods requiring frequent rehabilitating that can affect daily life. Operations to treat DDD can include:
- Lumbar Spinal Fusion Surgery is considered the standard surgical option for the treatment of lumbar degenerative disc disease. This fusion surgery joins two vertebrae
 to reduce pain by eliminating possible motion at the vertebral segments. Spinal fusion surgery can entirely remove the disc space (discectomy) or use bone grafting or artificial scaffolding implants to help stabilize the spine or end plates with screws and rods. The fusion surgery allows the vertebrae to grow together, changing two joints into one solid structure. Vertebrae Fusion can take months to heal and requires pain medications, physical therapy, and back braces to help stabilize & strengthen the lumbar region as the Vertebrae heal.
to reduce pain by eliminating possible motion at the vertebral segments. Spinal fusion surgery can entirely remove the disc space (discectomy) or use bone grafting or artificial scaffolding implants to help stabilize the spine or end plates with screws and rods. The fusion surgery allows the vertebrae to grow together, changing two joints into one solid structure. Vertebrae Fusion can take months to heal and requires pain medications, physical therapy, and back braces to help stabilize & strengthen the lumbar region as the Vertebrae heal. - Intervertebral disc annuloplasty (IDET) surgery seals/contains the damage by eliminating the irritated nerves causing pain by heating the damaged disc to 194° F (90 °C) for 15 minutes.
- Cervical corpectomy surgery is used for cases with cervical degenerative disc disease. It seeks to remove portions of the vertebra and intervertebral discs to provide relief and to allow for natural decompression of the spinal nerves and cervical spine. Metal endplates, screws, and bone grafts are then used to stabilize the area to allow the spine to heal.
- Anterior cervical discectomy is a surgical procedure that targets the cervical spine and endplate sclerosis. The damaged intervertebral cervical disc is first removed and then replaced with a bone graft or artificial substitute, and over time, the graft fuses with the vertebrae.
- Facetectomy surgery is most often used in treatments for facet joint disease. It surgically removes part of the facet joint to help increase the space and reduce pressure caused by spinal degeneration and collapsed discs.
- Dynamic Stabilization surgery is usually done after discectomy. This procedure is performed with an implant that acts as a stabilization post and relieves extra pressure from the spinal disc by focusing any pressure through the posterior section of the spine. Dynamic Stabilization surgery can be done with flexible rods, Dynesys screws (Pedicle), or Wallis ligament, which are interspinous spacers with bands. This surgery aims to mimic natural movements and maintain mobility by allowing the section to flex and extend as naturally as possible.
- Laminoplasty surgery creates more space for the nerve roots and spinal cord and relieves pressure on the cord. The procedure does not require bone fusion and can help preserve routine spinal rotations and movements.
- Foraminotomy surgery enlarges the vertebral foramen, increasing the space for root nerves. It is often combined with laminotomy surgery but can also be performed alone for symptoms of the vacuum disc phenomenon.
- Laminotomy surgery removes pressure on the irritated nerve roots by removing a small portion of the lamina. This is a very risky procedure that requires a significant operation that often results in substantial residual scar tissue and postlaminectomy syndrome complications.
- Microdiscectomy surgery is a new minimally invasive procedure that targets the damaged portions of herniated discs. In a Microdiscectomy procedure, the nucleus pulposus is removed using lasers or a surgical instrument guided by a microscope. This procedure is often used to treat sciatica leg pain. Still, it does carry some risk, and the potential for failed surgery can lead to complications, including cerebrospinal fluid leak (caused by dural tear), infection, additional Nerve root damage, Deep vein thrombosis, and the potential to cause a buildup of fluids in the lungs resulting in pneumonia.
- Spinal decompression surgery is considered a non-invasive procedure to temporarily enlarge the IVF region (intervertebral foramen), which can help to treat collapsed discs & rehydrate sections of the spinal discs.
- Percutaneous disc decompression surgery is used to reduce or eliminate portions of a damaged / bulging disc through a needle that is inserted into the discs.
- Spinal laminectomy surgery is most often used to treat spinal stenosis. By removing, trimming, or widening portions of the lamina, spinal laminectomy can help relieve pressure on the spinal cord and create additional space for irritated spinal nerves.
- Artificial Disc Replacement Surgery or Intervertebral disc arthroplasty is also called Total Disc Replacement (TDR) or Artificial Disc Replacement (ADR.) TDR surgery is another alternative to spinal fusion surgery but is mainly used in cases with advanced degenerative disc disease. The artificial spinal disc surgery first removes the damaged spinal disc (via discectomy), then implants an artificial disc device to help return the disc space to a functional height.
The artificial spinal discs are typically made up of:
- Central core made of polyethylene (surgical-grade plastic) or metal alloys that can bend or turn naturally and allow for movements at the spinal segment
- Two metal endplates are covered in a bio-pours coating that can be attached to the vertebral bodies. The surface helps the bone to graft itself to the device.
Recovery from a total disc replacement surgery and pain relief can take 6-12 months and might require periodic spine adjustments to ensure successful grafting without additional complications.
Treatment for Desiccated Discs & Discopathy
When the discomfort and pain from degenerative spine & degenerative disc disease are severe, conventional operative therapies are often ineffective. Adult autologous stem cells can offer an innovative non-surgical therapeutic method to reverse bulging disc degeneration and address chronic low back pain at its root for these inoperative conditions. Chronic lower back pain due to degenerative disc illness impacts an estimated 200 million individuals worldwide. While short-term solutions can be achieved by the use of analgesics, steroids, having enough rest, and frequent physiotherapy, there are still many people diagnosed with discopathy whose conditions rapidly become worse despite the traditional treatments that orthopedic surgeons recommend.
Treatment Options for Herniated Bulging Discs
If you are in this type of situation, you are often left with no other alternative but back surgery. The risky surgical method usually involves a spinal fusion or sometimes complete replacement of the degenerated disc with an artificial disc. Stem cell injections for back pain and MSC+ cell treatment for degenerative disk disease are currently the most reliable alternatives to back fusion surgery and contain endplate osteophytes.
Stem Cell Therapy for Degenerative Disc Disease
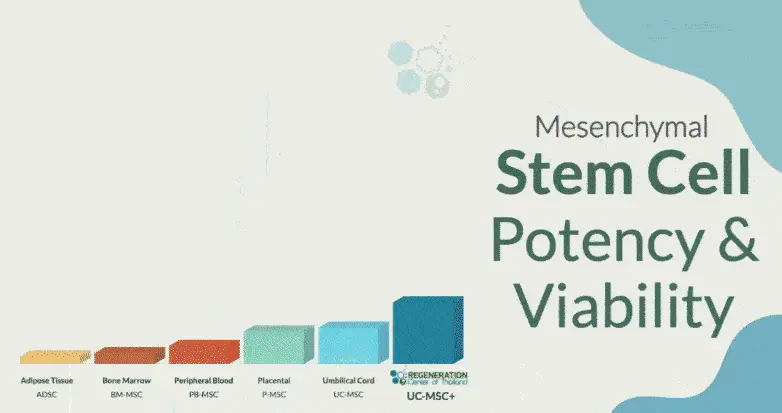
The Regeneration Center offers cutting-edge cell-based treatments for spinal diseases such as DDD. The cellular approach is unique as it uses therapeutic levels of enhanced Mesenchymal stem cells (UC-MSC+ Cells.) These UC-MSC+ cells can differentiate into stem cells of the chondrogenic lineage. This lineage of cells is especially beneficial for patients with DDD for therapeutic cartilage regeneration. Isolated and enhanced UC-MSC+ cells can differentiate into chondrocyte cells and help to modulate the local areas of damage, support new growth, promote anti-inflammatory cytokines (pro-inflammatory cytokines), and enhance the body’s natural immunomodulatory functions. Stem cells for back pain & disc regeneration therapy offer an effective alternative to back surgery, which is disk regeneration using enhanced stem cells for pain management, helping heal and restore nerve sensations. The Regeneration Center offers the most advanced treatment for sports-related injuries, osteoporosis, sarcopenia and chronic degenerative disc disease. Our stem cell injections for back pain are much safer than invasive surgical procedures. They seek to treat the actual cause of the disease and reverse the condition through a targeted multi-step treatment to regenerate the damaged discs to their normal, healthy state.[1]
Stop Back Pain without Surgery in 2025
Alternative to Fusion and Back Surgery
 The Regeneration Center recommends a unique approach to dealing with a degenerating back. With enhanced mesenchymal stem cells, post-therapy rehab, and joint pain friendly diet plan, (UC-MSC+) cells for neurological & spinal conditions can be used to repair the degenerative state of the spinal disks and surrounding tissue. We offer Autologous, and Allogeneic stem cell therapies using CD34+ stem cells, which are safe and effective for those with advanced degenerative disc disease and severe back pain due to failed surgeries or spinal arthritis. Our center uses isolated and expanded MSC+ cells that have immunomodulatory properties and decrease tissue damage by immune cells. These UC-MSC+ cells take advantage of the paracrine cell signaling mechanism to secrete neuroprotective factors and recruit angiogenic properties that help to restore the damaged areas of the spinal cord and also help to increase blood supply to surrounding tissues. [2] Patients with severe degeneration, peripheral neuropathy,or multiple ailments, including strokes, ataxia or artery disease, may require a combination therapy using a combination of stem cells from Umbilical Cord Tissue or Placenta-derived stem cells. Patients undergoing disc regeneration for DDD can expect minimal discomfort with safe cell isolation methods and delivery systems. Improvements are noticed quickly after the first treatment, starting with reducing pain and the body’s natural regenerative cycle.[3].
The Regeneration Center recommends a unique approach to dealing with a degenerating back. With enhanced mesenchymal stem cells, post-therapy rehab, and joint pain friendly diet plan, (UC-MSC+) cells for neurological & spinal conditions can be used to repair the degenerative state of the spinal disks and surrounding tissue. We offer Autologous, and Allogeneic stem cell therapies using CD34+ stem cells, which are safe and effective for those with advanced degenerative disc disease and severe back pain due to failed surgeries or spinal arthritis. Our center uses isolated and expanded MSC+ cells that have immunomodulatory properties and decrease tissue damage by immune cells. These UC-MSC+ cells take advantage of the paracrine cell signaling mechanism to secrete neuroprotective factors and recruit angiogenic properties that help to restore the damaged areas of the spinal cord and also help to increase blood supply to surrounding tissues. [2] Patients with severe degeneration, peripheral neuropathy,or multiple ailments, including strokes, ataxia or artery disease, may require a combination therapy using a combination of stem cells from Umbilical Cord Tissue or Placenta-derived stem cells. Patients undergoing disc regeneration for DDD can expect minimal discomfort with safe cell isolation methods and delivery systems. Improvements are noticed quickly after the first treatment, starting with reducing pain and the body’s natural regenerative cycle.[3].
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Degenerative Disc Disease with stem cells. Patients with advanced disc degeneration, severe spinal stenosis, significant nerve compression, or multiple comorbidities may not be good candidates for treatment.If you are currently experiencing slight to moderate discomfort or pain from a bulging disc or Herniated disc with lupus, you may be an ideal candidate for our innovative treatment, which uses proven and effective adult stem cell therapy to allow the spinal discs to regenerate without surgery.
Stem Cell Treatment for Degenerated Discs
The total number of cell infusions for DDD will depend on the patient’s needs. Most patients with mild to moderate DDD require multiple infusions of enhanced mesenchymal (UC-MSC+) cells per stage. Severe cases with multiple commodities may require several stages for sustained recovery.
Types of Stem Cells and Delivery Methods: For patients with moderate multi-level disc degeneration, multiple sessions of clinical grade expanded UC-MSC+ Mesenchymal Cells along with our proprietary mix of growth factors that can include Transforming Growth Factor-beta (TGF-β), Bone Morphogenetic Proteins (BMPs), Insulin-like Growth Factor-1 (IGF-1), Vascular Endothelial Growth Factors (VEGF), Fibroblast Growth Factors (FGF), Platelet-Derived Growth Factors (PDGF), Connective Tissue Growth Factors (CTGF), Epidermal Growth Factors (EGF), and Nerve Growth Factors (NGF). The regenerative therapy protocol will depend on the patient’s medical needs. Our autologous protocol will require 2-4 weeks of cell culturing before they can be used in therapies, while the allogeneic UC-MSC+ protocol does not require invasive surgeries or additional wait times. The isolated cells and growth factors are delivered via intravenous drips, direct local injections, intradiscal injections, intrathecal injections, fluoroscopy-guided stem cell delivery (in a hospital setting only), or a combination of different delivery methods to achieve the best results. To learn about the basics of stem cells, visit here.
DDD Treatment Guidelines – 2025
Safety and efficacy are paramount; therefore, all clinical treatments for degenerative discs with stem cells require 1-2 Weeks in Bangkok, Thailand. Due to the varying degrees of spinal disc degeneration and injury experienced by each person, our orthopedic team will need to review medical records for all potential candidates before a detailed treatment protocol can be provided. Upon completion of treatment evaluation, a detailed plan will be provided, covering a day-by-day treatment calendar with all appointments, the exact number of days required, and the total medical-related costs (excluding accommodations or flights). To begin the treatment qualification process for our multi-stage DDD treatment in Bangkok, please prepare your recent medical records (MRI or CT Scans) and contact us today.
Post-Treatment Physical Rehabilitation & Pain Relief: Physical Rehabilitation after your treatment for DDD is optional, depending on your travel restrictions. Complete physical rehab is available for 2-4 hours per day and up to 5 days per week. Regenerative medical packages, medical visas, and extended stay accommodations for the patient and family/friends can also be provided upon request.
Published Clinical Citations
[1] ^ Sivakamasundari, V, and Thomas Lufkin. 2013. Stemming the Degeneration: IVD Stem Cells and Stem Cell Regenerative Therapy for Degenerative Disc Disease in Thailand. Advances in stem cells. doi:724547. https://www.ncbi.nlm.nih.gov/pubmed/23951558
[2] ^ Yang, Fan, Victor Y L Leung, Keith D K Luk, Danny Chan, and Kenneth M C Cheung. 2009. Mesenchymal stem cells arrest intervertebral disc degeneration through chondrocytic differentiation and stimulation of endogenous cells. Molecular therapy : The Journal of the American Society of Gene Therapy, no. 11 (July 7). doi:10.1038/mt.2009.146. https://www.ncbi.nlm.nih.gov/pubmed/19584814
[3] ^ Drazin, Doniel, Jack Rosner, Pablo Avalos, and Frank Acosta. 2012. Stem cell therapy for degenerative disc disease. Advances in orthopedics (April 24). doi:10.1155/2012/961052. https://www.ncbi.nlm.nih.gov/pubmed/22593830

 What is DDD?
What is DDD?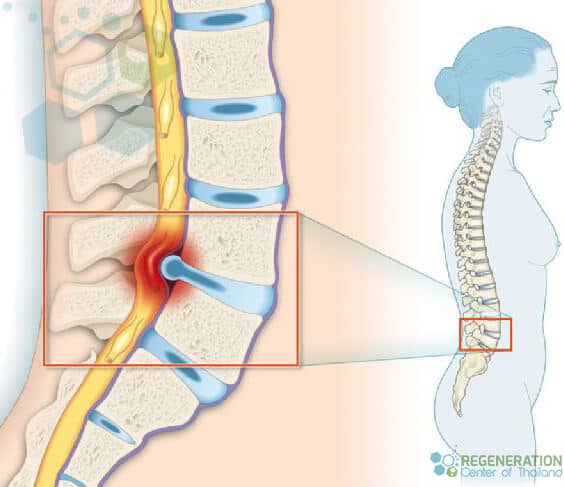 to reduce pain by eliminating possible motion at the vertebral segments. Spinal fusion surgery can entirely remove the disc space (discectomy) or use bone grafting or artificial scaffolding implants to help stabilize the spine or end plates with screws and rods. The fusion surgery allows the vertebrae to grow together, changing two joints into one solid structure. Vertebrae Fusion can take months to heal and requires pain medications, physical therapy, and back braces to help stabilize & strengthen the lumbar region as the Vertebrae heal.
to reduce pain by eliminating possible motion at the vertebral segments. Spinal fusion surgery can entirely remove the disc space (discectomy) or use bone grafting or artificial scaffolding implants to help stabilize the spine or end plates with screws and rods. The fusion surgery allows the vertebrae to grow together, changing two joints into one solid structure. Vertebrae Fusion can take months to heal and requires pain medications, physical therapy, and back braces to help stabilize & strengthen the lumbar region as the Vertebrae heal.