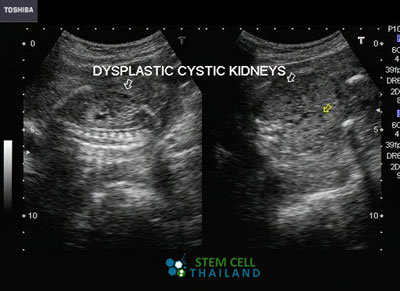
Polycystic kidney disease “PKD” is a medical condition wherein numerous fluid-filled cysts are found to have grown in either or both kidneys. These cysts cause enlargement and, if left untreated, can grow to an abnormal size that can destroy standard kidney structure and affect kidney function, which could lead to eventual kidney failure and death.
Warning Symptoms of Kidney Disease
The cysts are mostly benign or non-carcinogenic; most contain bodily fluids or water. However, because of continual fluid accumulation, their sizes could grow more significantly than those of the kidneys.
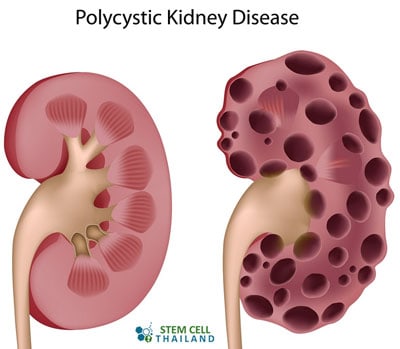 A kidney weighs less than a pound, but some cysts can weigh as much as 30 pounds, so it’s possible for things to get out of hand quickly. Polycystic kidney disease, which means “many cysts,” is a progressive disease that can severely affect kidney function and surrounding organs.
A kidney weighs less than a pound, but some cysts can weigh as much as 30 pounds, so it’s possible for things to get out of hand quickly. Polycystic kidney disease, which means “many cysts,” is a progressive disease that can severely affect kidney function and surrounding organs.
Early Diagnosis is Crucial
Rule #1 of functional medicine is early detection and awareness. Identifying the disease at the very onset is essential because our kidneys are responsible for many vital bodily functions. They are waste filters known as the “sweepers,” making them accountable for cleanliness within our bodies. The filtration process allows for the proper nutrients to be absorbed and the rest of the toxic substances to be flushed out of our systems.
Warning Signs and Symptoms of PKD
The most common signs of kidney problems are backaches or side pains, frequent urination, and blood in the urine. These four significant symptoms are characteristic of the disease and should signal your alarm to check yourself. The size of the abdomen may also noticeably increase over time.
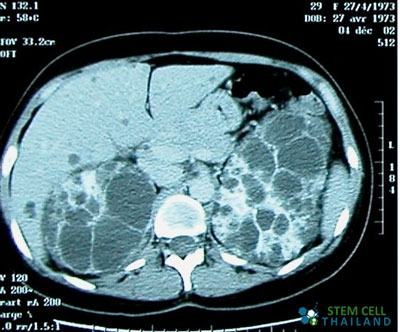
Other symptoms of congenital Polycystic Kidney Disease are headaches, high blood pressure, a history of urologic diseases, kidney lesions, renal cancer, chronic autoimmune glomerulonephritis, or conditions such as the presence of kidney stones or urinary tract infections. Although these cystic growths are usually benign most of the time, early diagnosis is crucial to prevent them from progressing rapidly, which would require patients to undergo more tedious medical procedures such as dialysis, stem cell treatments, or even kidney transplants.
Treatment for Polycystic Kidney Disease
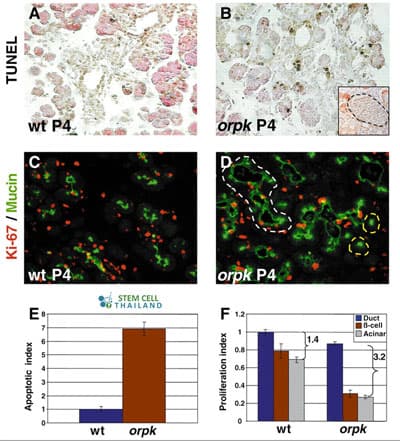
Stem cell therapy is rapidly gaining acceptance in modern science. Regeneration Center was one of the first providers of functional medicine for kidney diseases, using a non-surgical alternative to treat the symptoms of polycystic kidney disease. Our multi-stage treatment protocol seeks to reverse kidney damage and restore function with a faster recovery rate and much less risk than kidney transplants. Immune Enriched UC-MSC+ Stem cells help restore kidney function and repair damage and have been used effectively to treat numerous diseases and disorders, such as:
- Diabetes Type 2, Diabetic Neuropathy, and Acute Pancreatitis
- Neurological Conditions such as ALS, Ataxia, Alzheimer’s, Cerebral Palsy, Brain Injuries, Strokes, Parkinson’s and Motor Neuron Disease
- Orthopedic Knee Injuries, Hip Injuries, and Sports related injuries
- cardiac failure and heart disease
- Lung Diseases such as COPD or IPF
- Liver Disease
- Multiple sclerosis
- Blood disorders such as Thalassemia
- Systemic Lupus Erythematosus
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients are suitable candidates for treating Polycystic Kidney Disease with stem cells. Patients with advanced kidney enlargement, severe renal dysfunction, or other significant health complications might not be good candidates for treatment.These adult stem cells are programmed with vital nutritive factors that aid in healing damaged tissues by creating an almost new environment that is healthier for tissues and organs to thrive after disease and infections [1]. Clinical trials and medical journals have shown that stem cell transplants are the most effective known alternative treatment solution that does not require surgery. This non-surgical approach allows surrounding healthy tissue to be preserved more effectively.
With stem cell therapy being introduced into the treatment of kidney failure and renal diseases, the treatment aims to reduce and eliminate the need for dialysis significantly.[2]
Dialysis requires potent medications to be administered regularly to heal damaged renal tissues; however, their potency also adversely affects normal, healthy tissues. Our stem cell kidney protocol aims to eliminate this unnecessary scenario.
Previous Kidney Regeneration Patients
Treat PKD with Stem Cell Transplants in 2025
Due to the varying degrees of kidney damage and the stages of PKD disease, our medical team will need to qualify the potential patients before a detailed treatment protocol can be established. Our initial treatment review can be done online and takes seven business days. Suitable candidates for the PKD treatment will require approximately 10-14 days in Bangkok. Upon acceptance into the program, a detailed plan will be provided that will include the specifics, such as the exact total number of nights required, along with the total medical-related costs (excluding accommodations or flights).
Published Clinical Citations
[1] ^ Thatava, Tayaramma, Adam S Armstrong, Josep Genebriera De Lamo, Ramakrishna Edukulla, Yulia Krotova Khan, Toshie Sakuma, Seiga Ohmine, et al. Successful disease-specific induced pluripotent stem cell generation from patients with kidney transplantation. Stem cell research & therapy, no. 6 (December 6). doi:10.1186/scrt89. https://www.ncbi.nlm.nih.gov/pubmed/22142803
[2] ^ Ward, Heather H, Elsa Romero, Angela Welford, Gavin Pickett, Robert Bacallao, Vincent H Gattone, Scott A Ness, Angela Wandinger-Ness, and Tamara Roitbak. Adult human CD133/1(+) kidney cells isolated from papilla integrate into developing kidney tubules. Biochimica et biophysica acta, no. 10 (January 19). doi:10.1016/j.bbadis.2011.01.010. https://www.ncbi.nlm.nih.gov/pubmed/21255643