SpA (Spondyloarthritides) disorders are a family of autoimmune inflammatory conditions that share common manifestations like inflammation in the sacroiliac joints, spinal cord, or peripheral joints and often predisposes genetic factors such as the HLA-B27 gene. Members of the Spondyloarthritides disease family include reactive arthritis, axial spondyloarthritis (axSpA), psoriatic arthritis, and arthritic spondylitis, which is also associated with inflammatory bowel diseases such as ulcerative colitis & Crohn’s disease.
Ankylosing Spondylitis & Spinal Arthritis
What is ankylosing spondylitis?
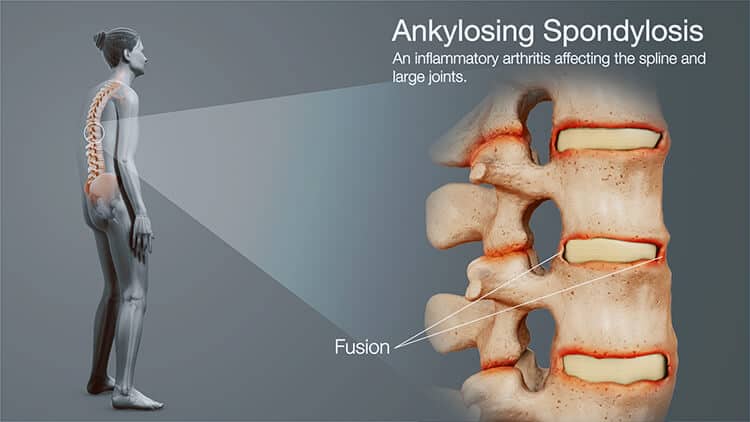
Ankylosing spondylitis (AS) is a progressive inflammatory rheumatic disease primarily found in the axial skeleton and sacroiliac joints.[1] The primary clinical manifestation of AS is frequent back pain and progressive stiffness in the spine “Bamboo spine.” Other affected areas include Oligoarthritis (arthritis affecting two to four joints), usually in the shoulders and hips. Other patients report having degenerative disc disease or enthesopathy, a disorder of the connective tissues between bones and tendons (entheses), ligament enthesopathy, and anterior uveitis. Although extensive research has been done, our current understanding of the underlying pathogenesis of ankylosing spondylitis is still minimal. Common causes are usually attributed to hereditary reasons (e.g., HLA-b27),infections, and autoimmune attacks.
Ankylosing spondylitis is classified as a type of arthritis in the spine and causes severe inflammation of the spinal joints, which leads to severe, chronic pain and frequent discomfort. For patients with more advanced AS, the chronic inflammation leads to new bone formations, causing sections of the spinal cord to become fused (fixed, immobile position) and is commonly referred to as bamboo spine. Bamboo spine generally develops due to ossification in the outer fibers of annulus fibrosus disci intervertebral (intervertebral discs), leading to Osteonecrosis of the hip or the formation of syndesmophytes (bony growth originating inside a ligament) between the adjoining vertebrae.
Spondyloarthropathy is considered highly heritable and is often associated with progressive rigidity, rheumatoid arthritis, peripheral arthritis, gouty arthritis and chronic inflammatory response in the spine and pelvis regions.
Who Gets Ankylosing spondylitis?
For most patients, diagnosis of ankylosing spondylitis comes at an early age and usually always results in some physical dysfunction and reduction in overall quality of life. It is estimated that over 90 percent of patients with ankylosing spondylitis carry mutations in the HLA-B27 gene. Recent research also shows that men are 2-3X times more likely to get diagnosed than women. Other known causes of AS include Tumor necrosis factor-alpha (TNF α) and IL-1. ANCA (Anti-neutrophil cytoplasmic antibodies) are also associated with Ankylosing spondylitis but do not necessarily correlate with how severe the patient’s condition will get.
Symptoms & Complications of Axial spondyloarthritis
As Ankylosing spondylitis begins to develop, patients report chronic inflammation in the spine, and radiology scans often show new bone formation in all spinal cord segments. Eventually, the calcification of vertebral and paravertebral ligaments will aggravate nerve endings resulting in chronic pain. The rate of new bone formation varies from patient to patient but is generally caused by increased differentiation of osteoblast cells. Patients diagnosed with spinal arthritis are at very high risks of developing spinal fractures, osteoporosis,lupus, spinal cord injuries, hypertension, heart diseases such as CHF, pulmonary complications leading to COPD or IPF (upper portion of the lung), and metabolic syndromes such as diabetes, neuropathy and diabetic nephropathy. Patients with AS also have a higher prevalence of dementia and Alzheimers, primary Sjogren’s Syndrome, ALS and MND compared with the general public. If left untreated, the condition degenerates over time, resulting in the loss of spinal mobility, place limitations in movement of the lateral flexion and anterior flexion. Other systemic failures common for patients with AS include weight loss, chronic fatigue, and fever. For most patients, pain is often worse when resting but can improve with light physical activity. [2]
Diagnosing Ankylosing Spondylitis Stage 4 Advanced
Ankylosing spondylitis and axial spondyloarthritis can be diagnosed today through checking for changes in the sacroiliac joints and spine using radiology scans such as an MRI. Genetic screenings are also done to check for the presence of the HLA-B27 marker. Patients who are HLA-B27 positive have a better-than-average risk for developing certain types of autoimmune disorders. For patients having acute inflammatory attacks, simple blood tests can be used to measure the concentration of CRP (C-reactive protein) and ESR 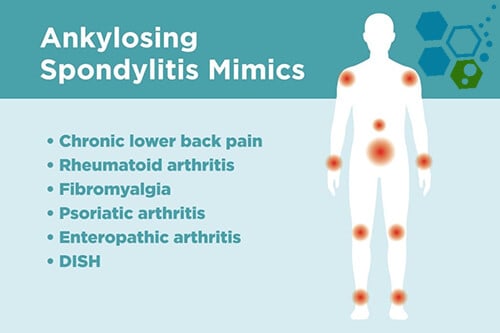 (erythrocyte sedimentation rate). However, it should be noted that there are many patients with ankylosing spondylitis whose ESR & CRP rates do not increase, so having normal CRP and ESR results might not correspond with the actual amount of inflammation that is present.
(erythrocyte sedimentation rate). However, it should be noted that there are many patients with ankylosing spondylitis whose ESR & CRP rates do not increase, so having normal CRP and ESR results might not correspond with the actual amount of inflammation that is present.
These general criteria for diagnosing spondyloarthritis include:
- Frequent inflammatory back pain
- Family history of inflammation in the tendon-bone attachments, heel, shoulder, or hip joints
- Positive test for HLA-B27 Gene – DNA Testing at Regen Center
- Elevated levels of inflammation measured by CRP/hs-CRP or ESR Blood tests
- Family history for spondyloarthritis or other rheumatic/autoimmune conditions
- Previous diagnosis for chronic lymphocytic thyroiditis
- A fair response to nonsteroidal anti-inflammatory drugs (NSAIDs)
- Psoriasis
- History of spinal inflammation
- Inflammatory bowel disease
- Frequent inflammation of the eye (uveitis)
- Inflammation of the sacroiliac joint confirmed with an MRI scan
Treatment options for Ankylosing spondylitis in 2024
Traditional antirheumatic drugs can help to improve back pain, disturbed sleep, peripheral arthritis acute phase responses, and temporarily improve quality of life; however, the major contributing factor of axial spondyloarthritis is new bone formation which is generally not affected. Due to this new alternative AS treatment try to focus on managing osteogenic differentiation to prevent new bone formation and induce a sustained disease remission period.[3]
Traditional Treatments of spondyloarthritis:
There is currently no cure for hereditary Ankylosing spondylitis. The success of modern biological treatments and traditional pharmaceutical medications can help contain the disease and reduce pain; however, early intervention is vital. It can be challenging to reach a confirmed diagnosis at the early stages to require a lengthy diagnostic stage. Starting with annual physical exams and tests can be used to detect the root of the symptoms.
Commonly used non-surgical treatments for Ankylosing spondylitis include Physical therapy & Exercise. Regular physical therapies can help restore some functionality in the joints. Occupational therapy is a great way to strengthen the tissues and muscles needed for a flexible, healthy body. Non-impact exercises can provide patients fast relief of pain and stiffness. This natural therapy can help reduce the risk of future disabilities.
Prescription Medications – DMARDs – NSAIDs
NSAIDs (nonsteroidal anti-inflammatory drugs) are the most common first treatment used for controlling symptoms. The family of such medications includes naproxen, aspirin, and ibuprofen. Other disease-modifying antirheumatic drugs (DMARDs) might be added to the patient treatment course for patients who do not respond to NSAIDs. DMARDs such as sulfasalazine include local injections of steroids to reduce stiffness, inflammation, and other discomforts. Prolonged use of medications causes severe reactions, liver cirrhosis, kidney failure, or gastrointestinal bleeding, peptic ulcers, hepatorenal damage, and cardiovascular events such as MI.
TNFα antagonists
Tumor necrosis factor-alpha is a physical blocker that is often referred to as “antagonists.” These TNFα antagonists include biological therapies such as infliximab, etanercept, adalimumab, and golimumab. Biologic medications such as interleukin 17 inhibitors & TNF blockers can trick the immune system to stop or slow down the inflammation process; however, the course of inhibiting the production of proinflammatory cytokines such as IL-17, IL-22, IFN-γ, and TNFα can result in severe side effects and for some patients reactivate tuberculosis or make patients more prone to getting new infections.
Surgical Treatment of Bamboo Spine
Thanks to advancements in medicine, surgery is very seldomly used today. However, for some late-stage cases, if pain or extreme swelling occurs rapidly, having surgery might be required. Surgeries would mainly look to replace damaged joints with new artificial joints. Such surgeries are prevalent in knee replacements and total hip replacement surgeries. Correction surgeries are also needed for patients with severe flexion deformities (downward curvature in the spine), particularly in cervical spine (neck) areas.
Risks of Surgery
Joint replacement surgeries are inherently risky and temporary as artificial joints need replacements over time. In addition, the preparation for surgery requiring general anesthesia makes the procedure even more complex to the risk of surgery. Any abrupt changes to the upper airway area can lead to problems intubating the airway. In some cases, direct spinal or epidural anesthesia may be impossible to extensive calcification of the damaged ligaments. Stiffness of the thoracic ribs can decrease pulmonary function or result in aortic insufficiency.
Stem Cell Treatment for Ankylosing Spondylitis
In the last two decades, a considerable amount of progress has been made in the regenerative treatment approach of spondyloarthritides.
The Regeneration Center Enhanced mesenchymal (MSC+) protocol includes a proprietary combination of adult mesenchymal stem cells, osteoblast-specific growth factors, adipocytes, and chondroblasts with ≥95% cell surface proteins consisting of CD90, CD73, CD105 markers. Learn more about stem cell therapy. We offer a viable treatment option for patients who have otherwise been unresponsive to traditional treatments. MSC+ cells offer significant regenerative and immunomodulatory properties that can help reduce the inflammatory responses and help repair surrounding tissues via the secretion of soluble factors provided with the growth factors during treatment.[5]
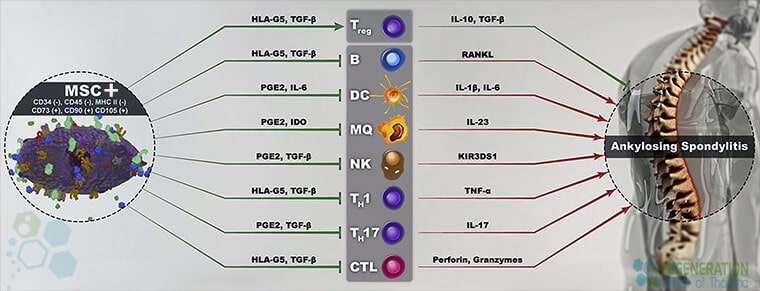
For treatment of immune-mediated inflammatory disease, the Regeneration Center has developed a unique combination therapy using hematopoietic stem cells & MSC+ cells that are particularly effective in stabilizing an otherwise abnormal rate of osteogenic differentiation. Learn about how we treat ibm muscle disease with stem cells.
MSC+ cells are engineered to provide low immunogenicity and immunomodulatory properties. MSCs+ therapy for Ankylosing spondylitis does not require immunosuppressive medications. MSC+ cell do not express HLA-DR, which makes them the ideal therapeutic medium for transplantation inpatients with immune-mediated disorders. MSC+ can eradicate dysfunctional cells restart the immune system by replacing damaged cells with cells that have been differentiated into standard B and T cells required for immune system homeostasis.[4]
The Regeneration Center Protocol for AS
Total Number of MSC+ Cell Infusions: Total Endogenous Cell Count and range of growth factors will vary based on patient needs. Multi-Point delivery of cells can be done via a Guided Radiograph (when necessary) through an Intravenous Drip, Direct injection, or Intrathecally.
Rehabilitation Post Treatment: Physical Rehabilitation in Bangkok is optional but highly recommended. Complete physical rehab services post-therapy can be provided upon request for 2-3 hours per day and up to 5 days per week.
Total Treatment Time Required: estimated around 2 weeks (depending on type and severity of condition). Medical and travel visas for extended stay accommodations at a hotel or extended stay apartment for the patient and family can also be provided upon request.
Spondyloarthritis Treatment Guidelines & Requirements
The Regen Center MSC+ Stem Cell treatment for spinal arthritis and Ankylosing spondylitis will require 12-16 days total. Due to the varying degrees of severity, our medical team will need to evaluate the patients using current medical records. Evaluations can be done in person or online (submitting documents online). After review, a detailed treatment plan will be provided that will include the specifics such as the exact total number of nights required and total medical costs for treatment of Ankylosing spondylitis with MSC+ stem cells. To begin the evaluation process, please prepare all current medical records and contact us today.
Published Clinical Citations
[1] ^Chiowchanwisawakit, P., Thaweeratthakul, P., Wattanamongkolsil, L., Srinonprasert, V., Koolvisoot, A., Muangchan, C., Nilganuwong, S., Arromdee, E., & Katchamart, W. (2019). Relationship Between Health-Related Quality of Life and Patient Acceptable Symptom State With Disease Activity and Functional Status in Patients With Ankylosing Spondylitis in Thailand. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases, 25(1), 16–23. https://doi.org/10.1097/RHU.0000000000000750
[2] ^ Luft F. C. (2017). Mesenchymal stem cells provide novel insights into ankylosing spondylitis. Journal of molecular medicine, 95(2), 119–121. https://doi.org/10.1007/s00109-016-1496-y
[3] ^Chiowchanwisawakit, P., Pithukpakorn, M., Luangtrakool, K., & Permpikul, P. (2021). HLA-B*27:04 associated with enthesitis and younger age of onset, and HLA-B allele profile in patients with ankylosing spondylitis in Thailand: A cross-sectional study. International journal of rheumatic diseases, 24(3), 411–417. https://pubmed.ncbi.nlm.nih.gov/33448675/
[4] ^Abdolmohammadi, K., Pakdel, F. D., Aghaei, H., Assadiasl, S., Fatahi, Y., Rouzbahani, N. H., Rezaiemanesh, A., Soleimani, M., Tayebi, L., & Nicknam, M. H. (2019). Ankylosing spondylitis and mesenchymal stromal/stem cell therapy: a new therapeutic approach. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 109, 1196–1205. https://doi.org/10.1016/j.biopha.2018.10.137
[5] ^ Zheng, G., Xie, Z., Wang, P., Li, J., Li, M., Cen, S., Tang, S., Liu, W., Ye, G., Li, Y., Wang, S., Wu, X., Su, H., Wu, Y., & Shen, H. (2019). Enhanced osteogenic differentiation of mesenchymal stem cells in ankylosing spondylitis: a study based on a three-dimensional biomimetic environment. Cell death & disease, 10(5), 350. https://doi.org/10.1038/s41419-019-1586-1