A Brain stem injury can occur via blunt force trauma to the brain no matter the age at onset. A head injury can result from a substantial handicap to the individual who sustained the brain injury and may trigger numerous types of cognitive impairments like lack of focus, memory, or other motor-neurological disorders such as ataxia, ALS, Spinal muscular atrophy, or Parkinson’s Disease. A brain stem injury may also consist of any damage that’s vascular by nature and not by blunt force trauma event that directly caused or instigated the intracranial Injury.
Etiology of Traumatic Brain Injury
Modern treatment options for head injuries are usually divided into two types: closed-head injuries and penetrating head injuries. Overlap for the two types does exist, and closed head injury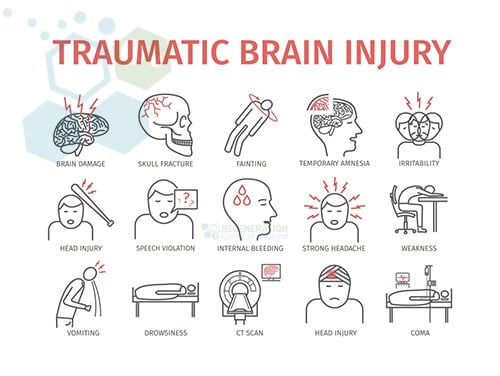 treatments can be further segmented into mild, moderate, or severe/traumatic head injuries. A neurological injury is dissimilar from a traumatic brain injury (TBI) or stroke because an exterior force injures the brain in a damaging, violent manner. TBI is an injury in the brain brought about by some traumatic influence. TBI and brain damage can be caused by blows to the head (severe head trauma), cerebral trauma, cranial penetration, or even violent trembling. Depending on the cause and severity of the trauma, the brain damage can be classified as severe, moderate, or mild, and damage from neurodegeneration can include glial cells, neurons, endothelial cells, and Axonal Degeneration. [1]
treatments can be further segmented into mild, moderate, or severe/traumatic head injuries. A neurological injury is dissimilar from a traumatic brain injury (TBI) or stroke because an exterior force injures the brain in a damaging, violent manner. TBI is an injury in the brain brought about by some traumatic influence. TBI and brain damage can be caused by blows to the head (severe head trauma), cerebral trauma, cranial penetration, or even violent trembling. Depending on the cause and severity of the trauma, the brain damage can be classified as severe, moderate, or mild, and damage from neurodegeneration can include glial cells, neurons, endothelial cells, and Axonal Degeneration. [1]
Classifications of Traumatic Brain Injuries (TBI)
A TBI occurs after damage to the brain from external forces such as Impacts, rapid deceleration or acceleration, blast 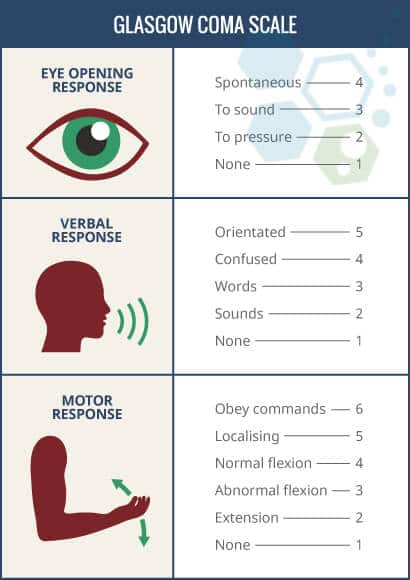 waves, or blunt force trauma. After such an incident, overall neurological impairment can be temporary or permanent depending on the severity of blunt force trauma to the head. The focus of this article will be to understand the signs, symptoms, and new treatment options for traumatic head injuries that occur after birth only, especially those following traumatic brain injury. There are currently two subsets of brain damage, including traumatic and non-traumatic (non-penetrating) brain injuries resulting from exposure to toxins, brain stroke, or viral infections. Most brain injuries are classified as either neurotrauma or central nervous system injuries that can affect cell signaling and neurotransmitters, which can lead to other neurodegenerative conditions like dementia. Recent medical studies also indicate that inflammatory responses following traumatic brain injury and autoimmune processes are significant factors process that leads patients from TBI events to eventual permanent loss of cognitive capabilities.
waves, or blunt force trauma. After such an incident, overall neurological impairment can be temporary or permanent depending on the severity of blunt force trauma to the head. The focus of this article will be to understand the signs, symptoms, and new treatment options for traumatic head injuries that occur after birth only, especially those following traumatic brain injury. There are currently two subsets of brain damage, including traumatic and non-traumatic (non-penetrating) brain injuries resulting from exposure to toxins, brain stroke, or viral infections. Most brain injuries are classified as either neurotrauma or central nervous system injuries that can affect cell signaling and neurotransmitters, which can lead to other neurodegenerative conditions like dementia. Recent medical studies also indicate that inflammatory responses following traumatic brain injury and autoimmune processes are significant factors process that leads patients from TBI events to eventual permanent loss of cognitive capabilities.
TBI is classified based on several factors, including severity, causative forces, anatomical locations of the Injury, and the mechanism. Mechanism-related injuries are either considered penetrating head injuries or nonpenetrating/blunt/closed Injuries. An open or penetrating head injury happens when an object goes through the skull and breaches the outermost membrane of the brain, known as the dura mater.
Glasgow Coma Scale – GCS
Traumatic Brain injuries are classified into three categories: mild, moderate, and severe. The most commonly used system around the world to classify TBI severity is known as The Glasgow Coma Scale (GCS). The GCS scale (3–15) grades a victim based on their level of consciousness, which measures motor, verbal, and eye-opening reactions. A brain injury with a GCS of 13 or above is considered mild, a head injury with a GCS score of 9–12 is deemed moderate, and any GCS score below eight is considered a severe head injury.
The GCS scale can also be changed after the victim is resuscitated, after post-traumatic amnesia (PTA), or after recovering from the loss of consciousness (LOC). Other methods of classifying the severity of TBI include using neuroimaging scans from CT, MRI, or PET to measure brain swelling, diffuse Injury, or focal lesions. A mild TBI is also commonly known as a concussion, but such an injury results in brain contusion or leads to trauma-induced paralysis.
Stem Cells Used in Cases with Anoxic Brain Damage
Each region of the human brain and spinal cord possesses specialized cells, including several cell types involved in treating traumatic brain injury. The Regen Center NeuroCell protocol uses adult MSC+ cells isolated and differentiated into neural, glial, and Astrocytes. These are crucial cell types involved in the damaged brain’s response following traumatic brain injury and are needed for specific regions that help develop the central nervous system (CNS).
Our neural cell replacement therapy for spinal cord injuries targets damaged areas and then repairs dead or diseased progenitor cells in the neurogenic region.
Initial symptoms and signs of the TBI could consist of:
- Headaches
- Blurred vision
- Dizziness
- Confusion
- Seizures
- Memory loss
- Loss of consciousness
- Paralysis or severe traumatic brain injury can lead to significant long-term disabilities and severe movement disorders
- Coma
Focal vs. Diffuse Brain Injuries
Using a CT scan, TBI lesions can also be classified by their pathological features, including extra-axial or intra-axial. Extra-axial lesions refer to injuries outside the brain but inside the skull, while intra-axial lesions refer to injuries inside the brain tissue. Depending on the severity, results from these injuries can be diffuse, focal, or both.
Warning Symptoms After Traumatic Brain Injury
Symptoms of Diffuse injuries include edema (brain swelling) and destruction to white matter tracts, cerebral hemispheres, and axons (diffuse axonal). Focal injuries, on the other hand, occur primarily in the orbitofrontal cortex and temporal lobes, resulting in behavioral changes, problems with decision-making, language difficulties, and decision-making skills.
Focal lesions such as Hematomas result in rapid blood collection around the brain. They can result in Intracerebral hemorrhage stroke, subdural hematoma (bleeding between the arachnoid membrane and the dura), subarachnoid hemorrhage (bleeding between the arachnoid membrane and the pia mater), aphasia, epidural hematoma (bleeding into the dura matter), or intraventricular hemorrhage (bleeding in the ventricles).
Stem Cell Treatment for TBI after Blunt Force Trauma
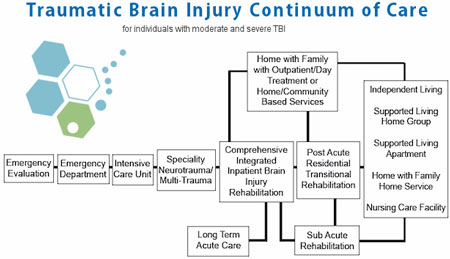
Early intervention is the key to optimal results in recovering from brain injuries that affect the nervous system. Response during the first 60 minutes after Injury, i.e., “golden hour,” is recommended.[2] For most patients, treatment options depend on the age of the Injury and stage of recovery. Patients in the acute phase are looking to stabilize the condition from progressing using a combination of surgery, physical rehabilitation, and therapy for traumatic brain injury.
For Acute stages of TBI or injuries that occurred playing sports, maintaining proper blood flow to the brain is critical to avoid brain herniation and seizures. In this stage, Decompressive craniectomy (DC) can be used to relieve intracranial pressure along with hyperbaric oxygen therapies to ensure proper oxygen supplies are maintained. Neuroimaging from brain scans is also used to target better therapies using analgesics, Sedatives, paralytic agents, and sometimes hypertonic saline to reduce swelling, regulate body temperature and hypotension, reduce the risk of heart failure, how to treat brain fog, or avoid electrolyte imbalances.
Patients with TBI are at a much higher risk of complications and adverse side effects, requiring contact monitoring for signs of deterioration or loss of consciousness. Other complications of Traumatic Brain Injuries include pulmonary edema and cardiac arrhythmia. In chronic stages of TBI, pharmacological-based treatments can be used to treat behavioral (psychiatric issues) and post-traumatic epilepsy. Learn about the best food for your brain.
Reverse Damage From Brain Injury – Stop Concussions
Brain Stem cell transplantation into the affected region might be beneficial in certain circumstances wherein the damage is not too severe and has occurred relatively recently. (from 6 months up to two years after initial Injury) The purpose of neural stem cell implantation is to attempt to restore signal functions with comparable properties. In situations of TBI, numerous cell kinds are required (glial, neuronal, vascular, endothelial ) to regenerate the complex tasks of largely damaged regions of the brain.[3]
Neural Cell Replacement Therapy
In much more severe instances of traumatic brain-related injuries, such as Chronic traumatic encephalopathy (CTE), some complications can be fatal. While the rigorousness of the TBI
Though the severity of traumatic brain injury differs broadly, the consequences of it, in the long run, are frequently devastating and life-changing for the injured brain. TBI is typically very sudden, and early intervention is the key to a full recovery. The physical, non-congenital harm towards the brain by an external force may permanently or temporarily disrupt regular brain function, often seen in patients following traumatic brain injury. [4] Brain characteristics and functions that may be affected include temporary or permanent loss of consciousness, speech, language, memory, character, mobility, joint pain with lupus, peripheral neuropathy, and recognition of other people. Since the brain controls all bodily functions, any harm to the brain (neurons) can impair physical and psychological activity, no matter how little or severe.[5]
TREATMENT RISKS & PRECAUTIONS
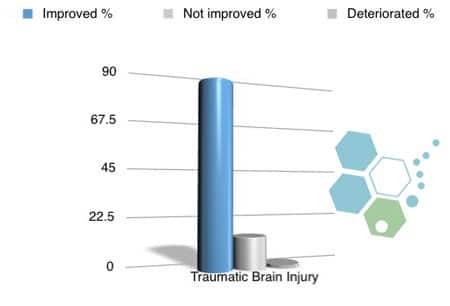
Please note that not all patients are suitable candidates for treating brain injuries with stem cells. Patients with extensive brain damage, severe cognitive impairment, or other critical health issues might not be good candidates for treatment.Stem Cell Treatment For TBI – 2025 Protocol
Total Number of MSC+ Cell Sessions Needed: For most patients, we will need multiple Infusions of isolated and expanded mesenchymal cells, which can be cultured from autologous sources of bone marrow (BMMSC) or allogeneic sources of cells (UC-MSC) and Neural Stem cells (MSC–NSC). These stem cells, and our proprietary combination of growth factors are joined to enhance the therapeutic potential of the treatment. The growth factors we isolate and culture are naturally occurring proteins in cells that stimulate cell growth, proliferation, healing, and differentiation and are combined with stem cells to support brain repair and regeneration. Some of the growth factors we isolate for TBI patients include Brain-Derived Neurotrophic Factor (BDNF), Nerve Growth Factor (NGF), Epidermal Growth Factor (EGF), Vascular Endothelial Growth Factor (VEGF), Fibroblast Growth Factors (FGFs), Insulin-like Growth Factor 1 (IGF-1), Glial Cell Line-Derived Neurotrophic Factor (GDNF)
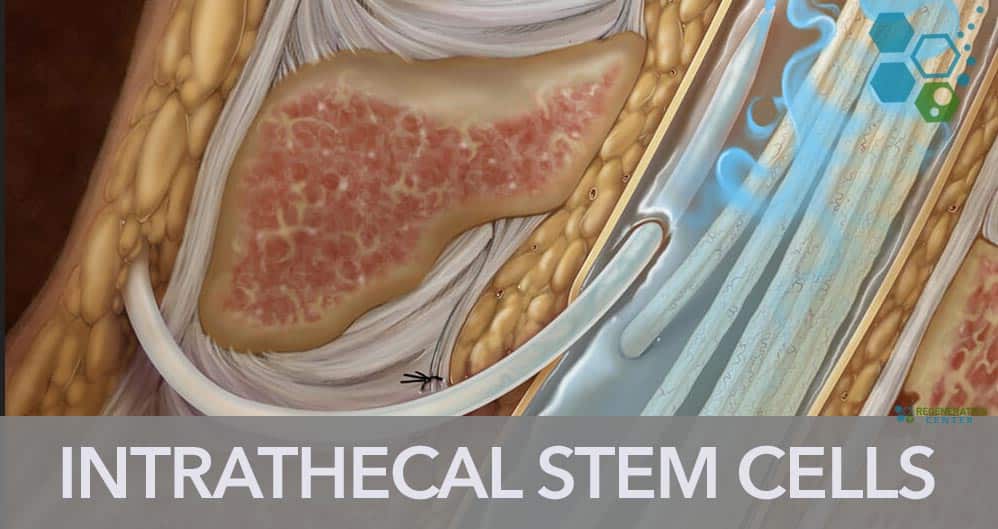
Delivery Methods of MSC+ and Neural Stem Cells: The types of cellular infusions will vary based on patient needs. However, our treatment aims to help reduce systemic neuroinflammation and promote faster recovery of lost cognitive function through neurogenesis for most acute brain stem injuries. To achieve these results, the cells can be administered using a combination of Intravenous infusions, stereotactic-guided delivery, inhalation therapy via micro-nebulized mesenchymal cells, Intrathecal infusions, and fluoroscopic guided cell delivery (in a hospital setting only). All intrathecal injections at The Regeneration Center are done by a board-certified neurosurgeon and are needed to bypass the blood-brain barrier. Healing the blood-brain barrier (BBB) can be a crucial part of treatment because it plays a vital role in maintaining the stability of the brain’s environment and protecting it from harmful substances.
Clinical Rehabilitation Post-Treatment: Physical Rehabilitation therapy in Bangkok is optional, depending on the patients’ travel/time constraints. Complete physical rehabilitation post-therapy can be provided upon request for 2-4 hours per day and up to 5 days per week. Medical visas and extended stay accommodations for the patient and family can also be included upon request.
Cost of Treating Brain Injuries with Stem Cells & Physical Rehab
The Regeneration Center stem cell treatment for Traumatic Brain Injuries will require a minimum of 2 weeks in Bangkok, focusing on mesenchymal stem cell transplantation for the injured brain. Due to the significant differences in brain injury treatment requests, our medical team must qualify the potential candidate for treatment. Upon acceptance, a detailed treatment plan will be provided and include the specifics of the treatment plan, including the total number of nights required and the total medical-related expenses, including cell extraction, enrichment, and infusions (excluding accommodations or flights). To begin the qualification process for multi-stage TBI neural stem cell transplants, please prepare your recent medical records, such as recent Brain MRIs, CT Scan (Preferred), or PET Scans, and contact us today.
Published Clinical Citations
[1] ^ Dharmasaroja, Permphan. 2008. Bone marrow-derived mesenchymal stem cells for the treatment of ischemic stroke. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, no. 1 (November 18). doi:10.1016/j.jocn.2008.05.006. https://www.ncbi.nlm.nih.gov/pubmed/19017556
[2] ^ Dinh, Michael M, Kendall Bein, Susan Roncal, Christopher M Byrne, Jeffrey Petchell, and Jeffrey Brennan. 2012. Redefining the golden hour for severe head injury in an urban setting: the effect of prehospital arrival times on patient outcomes. Injury, no. 5 (February 14). doi:10.1016/j.injury.2012.01.011. https://www.ncbi.nlm.nih.gov/pubmed/22336130
[3] ^ Kunkanjanawan, Tanut, Parinya Noisa, and Rangsun Parnpai. Modeling neurological disorders by human induced pluripotent stem cells in Thailand Journal of biomedicine & biotechnology (November 24). doi:10.1155/2011/350131. https://www.ncbi.nlm.nih.gov/pubmed/22162635
[4] ^ Prè, Deborah, Michael W Nestor, Andrew A Sproul, Samson Jacob, Peter Koppensteiner, Vorapin Chinchalongporn, Matthew Zimmer, Ai Yamamoto, Scott A Noggle, and Ottavio Arancio. 2014. A time course analysis of the electrophysiological properties of neurons differentiated from human induced pluripotent stem cells (iPSCs). PloS one, no. 7 (July 29). doi:10.1371/journal.pone.0103418. https://www.ncbi.nlm.nih.gov/pubmed/25072157
[5] ^ Yang, Yongxiang, Yuqin Ye, Xinhong Su, Jun He, Wei Bai, and Xiaosheng He. 2017. MSCs-Derived Exosomes and Neuroinflammation, Neurogenesis and Therapy of Traumatic Brain Injury. Frontiers in cellular neuroscience (February 28). doi:10.3389/fncel.2017.00055. https://www.ncbi.nlm.nih.gov/pubmed/28293177