Cell-based cancer treatments such as NK Cell Therapy are an excellent alternative to traditionally dangerous, high dose chemotherapy or radiation therapies used by oncologists around the world. CD4+ T-Lymphocyte Cell Regeneration to treat Non-Hodgkin lymphoma may be the solution.
Immunotherapy – Treat Cancer without Chemo
CAR T-cell therapy
Our immune system normally keeps track of all the substances found in the body. Detection of any new unknown substance raises an internal alarm, causing our immune system to attack it.
Chimeric antigen receptor (CAR) T-cell therapy is a new breakthrough treatment that uses our immune cells (T cells which are a type of white blood cells) to fight cancer cells more effectively. The Regeneration center is able to modify T-Cells in our lab and then reintroduced back to the cancer patient so the modified T Cells can seek and destroy cancer cells in the body. CAR T-cell therapy is also recognized as a type of cell-based gene therapy, because the process involves altering/reprogramming the genes that are inside Immune T cells to focus and attack the cancer cells only.
Stem Cells & Treating Cancer
Stem cells can, and are being used to treat cancer today. Gene Therapies and Cell-based treatments for cancer are used throughout the world but for only a few types of diseases such as Non-Hodgkins lymphoma. Stem cells can provide treatment for the two main types of blood cancers, including lymphoma and leukemia. When children or adults are given a high dosage of chemotherapy to try to irradiate as many of cancer cells as possible, which it does but at the high cost of massive destruction of bone marrow 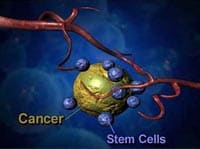 that produces stem cells that are needed by the body to recover and regenerate. To overcome this obstacle, oncologists have been using injections of umbilical cord blood, or placenta-derived stem cells from otherwise healthy donors to allow the body to recover as it naturally should have the bone marrow still been viable. These implanted stem cells are usually injected into the patients’ veins, similar to blood transfusions. Once the enhanced cells are introduced via engraftment into the body, they home their way to the patients bone marrow and quickly begin producing healthy hematopoietic blood cells. This process is not recommended for everyone and may cause other complications for patients with late stages or other underlying diseases that will affect cell therapy for cancer. Is cancer considered an autoimmune disease?
that produces stem cells that are needed by the body to recover and regenerate. To overcome this obstacle, oncologists have been using injections of umbilical cord blood, or placenta-derived stem cells from otherwise healthy donors to allow the body to recover as it naturally should have the bone marrow still been viable. These implanted stem cells are usually injected into the patients’ veins, similar to blood transfusions. Once the enhanced cells are introduced via engraftment into the body, they home their way to the patients bone marrow and quickly begin producing healthy hematopoietic blood cells. This process is not recommended for everyone and may cause other complications for patients with late stages or other underlying diseases that will affect cell therapy for cancer. Is cancer considered an autoimmune disease?
Candidates for Lymphocyte Restoration
Ideal candidates for our cancer treatment protocol are:

- Your Non-Hodgkins lymphoma or Relapsed Hodgkin’s disease
- Relapsed or high-risk non-Hodgkin’s lymphoma
- large B-cell lymphoma is likely to come back
- Non-Responsive cancer/lymphoma
- Relapsed testicular cancer
- Modified Immunotherapy for Lung Cancer
- Multiple myelomas
- Treatment for Liver cancer
- Acute leukemia
- Colorectal cancer (CRC)
- Treatment for Prostate cancer
- Treatment of pancreatic cancer
Modified Immune Cells to Fight Cancer – 2024
The Two Types of Cells Used in Cancer Remediation:
- Autologous stem cells for cancer come from your own body. Usually via Peripheral Blood stem cells, Bone marrow stem cells, dental pulp stem cells, and adipose fat stem cells.
- Allogeneic stem cells for cancer come from blood matched or family donor. (Not from your own body) Allogeneic stem cell transplants are most commonly used to treat certain types of cancers, lymphomas, and leukemia, along with bone marrow disorders line myelodysplasia. [1]
Safe, Targeted & Individualized for Better Success Rates
Stem Cell Collection and Expansion
Your specific protocol will depend on your current diagnosed needs. Typically, stem cells treatments for cancer require a multidisciplinary approach to ensure our clients can make a complete recovery and continue to live a long and healthy life.
Depending on your needs, we offer a few solutions to treat cancers with and without the need for just Chemotherapy, including:
- Radiotherapy Treatment using High Intensity Focused Ultrasound – HIFU
- Lymphocyte Regeneration using Hematopoietic stem cells [2]
- Combination of both plus other treatments such as Monoclonal antibody therapy and steroids
- Proton Beam Therapy
High-dose Stem Cell Transplants
The Regeneration center of Thailand offers a unique cancer treatment that requires cell collection for 2, or 3, days to ensure our doctors can collect enough of the needed types of cells. Collecting the stem cells requires 1 to 3 hours each visit.

The collection does not require any surgery or anesthesia and is generally non-invasive [3]. If your blood work and cell counting (flow cytometer) don’t show enough quantities of the needed types of stem cells, you may need injections of G-CSF to promote your bone marrow (iliac crest extractions) to release more stem cells. We also offer stem cells banking for up to 30 years if you are interested in saving your stem cells as an insurance policy for traumatic events such as brain strokes & heart attacks.[4]
TREATMENT PRECAUTIONS & RISKS
Please note Cell-based Therapies are not appropriate for all types of Cancers. Cell Therapy and Hematological Engineering may be limited in cases not requiring Bone Marrow Transplant TherapyCancer Immunotherapy Program Costs in 2024
All cancer treatment protocols require a minimum of 14-30 nights in Bangkok. Due to the varying degrees/stages of Illness, our medical team and oncologist will need to better understand the potential patient’s condition before acceptance into the program.
To determine eligibility and get exact fixed prices our doctors will need to better understand the patient’s existing needs via recent histological results, Biopsies, DNA Tests, blood tests, x-rays, scans, bone marrow sample results, or clinical diagnosis from your oncologist in your home country.
Upon acceptance, specifics relating to the treatment will be provided, including total number nights required along with the entire medical related costs (excluding accommodations or flights). The exact prices for the stem cell cancer protocol will include all the hospital fees, stem cell extraction, and expansion fees, doctors fees, and follow up consultations for 12 months after treatment.
To learn more or apply to our alternative treatment for cancer without Chemotherapy please contact us Today.
Published Clinical Citations
[1] ^ Kheansaard, Wasinee, Sumana Mas-Oo-di, Surasak Nilganuwong, and Dalina I Tanyong. 2012. Interferon-gamma induced nitric oxide-mediated apoptosis of anemia of chronic disease in rheumatoid arthritis. Rheumatology international, no. 1 (January 19). doi:10.1007/s00296-011-2307-y. https://www.ncbi.nlm.nih.gov/pubmed/22258456
[2] ^ Sadler, Nicole M, Britney R Harris, Brittany A Metzger, and Julia Kirshner. 2013. N-cadherin impedes proliferation of the multiple myeloma cancer stem cells. American journal of blood research, no. 4 (December 18). https://www.ncbi.nlm.nih.gov/pubmed/24396705
[3] ^ Snyder, Joshua C, Lauren K Rochelle, Larry S Barak, and Marc G Caron. 2013. The stem cell-expressed receptor Lgr5 possesses canonical and functionally active molecular determinants critical to β-arrestin-2 recruitment. PloS one, no. 12 (December 27). doi:10.1371/journal.pone.0084476. https://www.ncbi.nlm.nih.gov/pubmed/24386388
[4] ^ Subbiah, Vivek, Robert E Brown, Mary F McGuire, Jamie Buryanek, Filip Janku, Anas Younes, and David Hong. 2014. A novel immunomodulatory molecularly targeted strategy for refractory Hodgkin’s lymphoma. Oncotarget, no. 1 ( 15). https://www.ncbi.nlm.nih.gov/pubmed/24395633


