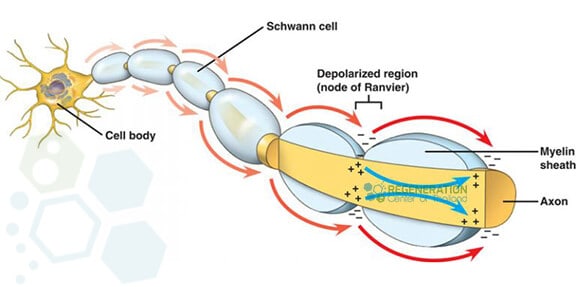
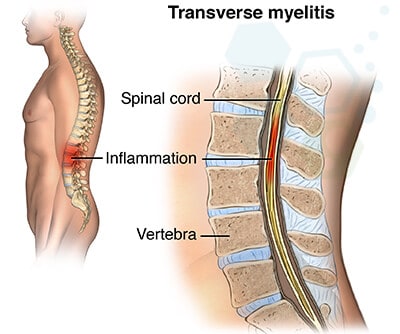
Transverse myelitis is a rare neurological impairment caused by inflammation in both sides of the spinal cord, resulting in damage to the myelin sheath, an insulating material covering nerve cell fibers. These nerve fibers are responsible for motor and sensory signals that carry information to and from the brain. Myelitis refers to inflammation in the spinal cord, while transverse refers to a specific pattern of changes in sensations across the body. Symptoms of TM can be sudden (acute) or slowly develop over a more extended period. [1]
What is Transverse Myelitis (TM)?
TM results in a bilateral sensory deficit that can affect patients at any age-irrelevant of race & gender. The condition does not appear to be hereditary and is typically diagnosed between patients from age 10 to 40 years old. Recovery from TM can be slow, but with early intervention and modern regenerative medicine, patients can recover from transverse myelitis with little to no lingering symptoms. If left untreated, the damage from transverse myelitis can be permanent, with impairments affecting patients’ ability to do routine daily tasks. Most patients go through a single episode of transverse Myelitis, while others can have a recurrence, especially if the patient has other underlying issues, such as autoimmune disease.
Causes of Transverse Myelitis
For many patients, the diagnosis of TM is idiopathic (no known cause), but for others, damage to the bundle of nerve fibers in the spinal cord can be attributed to:
- Fungal infections in the spine (Blastomyces, aspergillus, cryptococcus, coccidiosis)
- Viral infections from herpes viruses, Epstein-Barr, varicella-zoster, hepatitis B, cytomegalovirus, flaviviruses (West Nile and Zika), echovirus, rubella, mumps, and measles
- Bacterial infections from tuberculosis, actinomyces, syphilis, pertussis, diphtheria, tetanus, Lyme disease, middle-ear infections, skin infections, gastroenteritis (Campylobacter jejuni), and mycoplasma bacterial pneumonia
- Immune system disorders from Neuromyelitis Optica, amyotrophic lateral sclerosis, multiple sclerosis and type 1 diabetes
- Parasitic infections, including angtiostrongyloides, cysticercosis, toxoplasmosis, and schistosomiasis
Vascular dysfunctions from arterial-venous fistulas, arteriovenous malformation, disk embolisms, and intra-spinal cavernous malformations
Inflammatory disorders such as systemic lupus erythematosus, mixed connective tissue disease, Crohn’s disease, Bechet’s syndrome, IPF, sarcoidosis, Sjogren’s syndrome, and scleroderma
For some patients, a diagnosis of transverse myelitis might be the first symptom of a completely different immune-mediated disease, such as ankylosing spondylitis. Some patients are diagnosed with “Partial” Myelitis, while others are diagnosed as “complete” due to severe numbness & paralysis on both sides of the spinal cord.
Common symptoms of TM
The diagnosis of transverse myelitis can be acute(sudden) or subacute (develops over one month). [2] The spinal cord area at which the attack occurs will determine which parts of the patient’s body are affected. For some patients, damage to one segment of the spine will only affect function at that level or below, while in others, the damage to myelin is 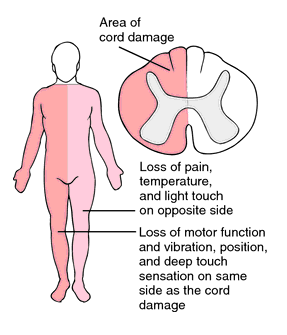 localized in the nerves of the upper back and cervical spine.
localized in the nerves of the upper back and cervical spine.
Common symptoms of transverse myelitis include:
- Bladder & Bowel dysfunction – Symptoms include increased frequency of using the bathroom due to constipation or incontinence
- Sharp pain that is usually localized to the lower back area but can include radiate pain like sensations down the arms, legs, or torso
- Sensory alterations—TM is known to cause abnormal sensations (paresthesias) throughout the body, including burning, prickling, tickling sensations, coldness, tingling, or numbness in the legs, torso, arms, and genital areas.
- Weakness of the legs and arms – Often misdiagnosed as Myasthenia gravis (MG), MND, Specific non-fluent aphasia, Ataxia patients with transverse myelitis can develop rapidly progressive weakness in the legs. If the spinal inflammation is in the upper spinal cord areas, it will affect the arms. Some patients can also develop partial paralysis of the legs(paraparesis), leading to complete paralysis in the legs (paraplegia).
Depending on age, some patients are also experiencing frequent muscle spasms, overall discomfort, fever, headaches, respiratory problems, loss of appetite, sexual dysfunction, anxiety, chronic back pain, and depression.[3]
Diagnosis of Transverse Myelitis
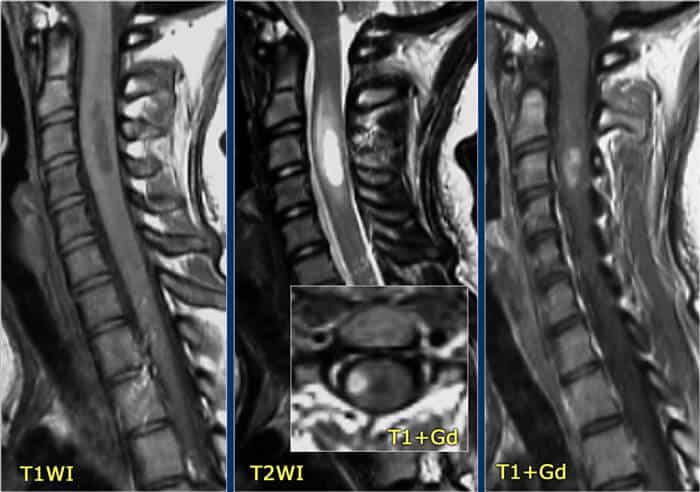
 Diagnosing spinal cord injury or spinal cord inflammation is based on the clinical analysis of patient symptoms, reviewing medical history, and conducting various examinations. The diagnosis of myelitis is then confirmed by medullary MRI, which shows a white spot (hyper signal) in the spinal cord, affecting more than half of it in width and variable height. It is often enhanced after the injection of contrast. A detailed evaluation can require many steps but is necessary to reach a diagnosis. The clinical diagnosis of transverse myelitis is reached through a process of elimination using a series of exams that can include:
Diagnosing spinal cord injury or spinal cord inflammation is based on the clinical analysis of patient symptoms, reviewing medical history, and conducting various examinations. The diagnosis of myelitis is then confirmed by medullary MRI, which shows a white spot (hyper signal) in the spinal cord, affecting more than half of it in width and variable height. It is often enhanced after the injection of contrast. A detailed evaluation can require many steps but is necessary to reach a diagnosis. The clinical diagnosis of transverse myelitis is reached through a process of elimination using a series of exams that can include:
- Blood tests – The least minor invasive type of test available, blood tests are used to first rule out other disorders with similar symptoms, including vitamin B12 deficiency or HIV. Blood tests check for anti-aquaporin-4, anti-myelin oligodendrocyte, and paraneoplastic autoantibodies. The presence of these proteins (autoantibodies) can show a direct link to conditions like Alzheimer’s or autoimmune disorders and can lead to a confirmed cause of transverse myelitis.
- Cerebrospinal fluid (CSF) analysis and Lumbar punctures (spinal tap) are much more invasive than radiology and blood tests. Still, they are necessary to correctly identify higher-than-normal protein levels and leukocytes (white blood cells), which are crucial for the body to help fight infections.
- Radiology scans from MRI or CT—Computed tomography (CT) and magnetic resonance imaging (MRI) scans are used to detect inflammation. Radiology scans help create a three-dimensional (cross-sectional) view/image of areas in the body, including the spinal cord and brain. An MRI of the spine can confirm any lesions in the spinal cord, while a brain CT scan can provide signs of other potential causes. If none of the methods lead to a specific reason, the patient is often diagnosed with idiopathic transverse myelitis.
Traditional treatment options for Transverse Myelitis
Treatment options for transverse myelitis depend on the patient’s age, severity, or underlying cause. Traditional treatment options are designed to target the infection itself, reduce inflammation in the spinal cord, and manage or alleviate symptoms such as pain. Traditional management for TM and its many complications include:
- Prescription medications to target any complications or symptoms, including tonic spasms(painful muscle contractions), incontinence, stiffness, and depression
- Antiviral, antibiotic, or antiparasitic medicines for those with viral infections of the spinal cord
- Intravenous immunoglobulin (IVIG) medications can reset the immune system. IVIG is a concentrated injection of antibodies from healthy donors that can bind to the antibodies causing the disorder and remove them from circulation in the body.
- Pain medicines can reduce muscle pain. Common medications include ibuprofen, acetaminophen, and naproxen. Nerve pain can be reduced using a combination of duloxetine (an antidepressant), tizanidine, baclofen, or cyclobenzaprine (a muscle relaxant), and gabapentin or pregabalin, which are anticonvulsant drugs.
- Systemic corticosteroids, such as methylprednisolone or dexamethasone, can decrease inflammation and swelling in the spine or reduce immune system activity. These powerful medications can reduce the risk of future attacks.
- Plasmapheresis (Plasma exchange therapy) is often used for patients who don’t respond well to corticosteroids. Plasma exchange therapy helps reduce abnormal immune system activity by first removing the fluid in which blood cells and antibodies are suspended (plasma) and replacing it with other liquids such as saline or albumin. Thus, the antibodies or proteins that could be causing the severe inflammatory reaction in the spine are filtered out.
TREATMENT RISKS & PRECAUTIONS
Please note that not all patients diagnosed with Transverse Myelitis are suitable candidates for treatment with UC-MSC+ stem cells. Individuals with complete spinal cord transection, complete paralysis, severe nerve damage, advanced paralysis, movement disorders, respiratory issues or other significant health complications may not be appropriate candidates for this therapy.UC-MSC+ Stem Cell Therapy for Transverse Myelitis
For over 12 years, the Regeneration Center has been on the leading edge of functional healthcare and regenerative medical research to understand better how our immune system attacks the nerve cell fibers and myelin in patients diagnosed with autoimmune disorders. Our work focuses on using modern cell-based therapeutics to repair demyelinated spinal cords. Our research has led to a much greater understanding of the underlying mechanisms responsible for damaging the myelin sheath. It offers patients a viable means to prevent and treat transverse myelitis, reduce relapse rate, and diminish harmful inflammatory activities.[4]
After an inflammatory injury, patients are left with a spinal cord injury in which the signaling capacity of nerve cells has died, resulting in loss of sensation, permanent weakness, and bladder/bowel dysfunction. The Regeneration Center has developed a novel strategy to direct stem cells into becoming healthy motor neurons. It uses proprietary developed growth factors to direct them to repair the damaged myelin sheath and reconnect with muscle fibers.
Using isolated and enhanced MSCs+ Mesenchymal cells from autologous or allogeneic sources, the Regeneration Center has successfully repaired lost function in the central nervous system. This advanced treatment for TM represents a realistic option to restore some function in patients with partial paralysis.[5] MSCs+ Stem cells carry anti-inflammatory properties that help stimulate neuronal activity, regulate the immune system, and reduce the production of inflammatory proteins (associated with stress). Our combination therapy uses multipotent glial cells and neural progenitor cells to help directly promote axons’ rapid growth (nerve fibers) at the lesion sites. MSC+ cells can differentiate into many other cell lineages, making them an attractive & non-toxic alternative to traditional treatment for Transverse Myelitis. MSC+ cells work via the paracrine effect, helping to stimulate neurogenesis, secrete neurotrophic growth factors, modulate the plasticity of damaged tissue, restore synaptic transmitter sites, and integrate into existing synaptic/neural networks. MSC+ stem cells also carry immunomodulatory properties that help inhibit the release of undesired pro-inflammatory cytokines.Learn more about stem cell therapies.
The treatment may also require astrocytes, Oligodendrocyte progenitor cells (OPCs), and glial cells (Glia, neuroglia), which are non-neuronal cells that help form myelin and also provide support and protection for existing healthy neurons. OPC stem cells help in the production and proliferation of myelin-producing oligodendrocytes needed for remyelination. They are part of an effective stem cell treatment protocol for transverse myelitis.
Type of Injections: A more aggressive combination therapy may be required for patients with acute transverse myelitis. Autologous cells might not be appropriate for all cases, and allogeneic cell infusions will require multiple infusions and will not require invasive surgery to collect cells. MSC+ cells can be delivered via a Guided Radio Scanner (when necessary) or via an intravenous drip, nebulizer, or intrathecal delivery to bypass the BBB.
Physical Rehabilitation Post-Therapy: Physical Rehabilitation therapy for TM in Bangkok is optional, depending on the patients’ travel/time constraints. Complete physical rehabilitation post-therapy can be provided upon request for 2-5 hours per day and up to 5 days per week. Medical visas and extended stay accommodations for the patients and families can also be included upon request.
Evidence of Disease Recovery
Inflammation is a way for our bodies to protect itself. Since the spinal cord is tightly wrapped in bony vertebrae, there is zero room for swelling or inflammation. Even a minor inflammation applies significant pressure to the spinal cord and can damage healthy tissue surrounding the point of inflammation.
The overall success and efficacy of UC-MSC+ stem cell treatment are measured by reducing the relapse rate and total lesions 6-12 months after MSC+ treatment. The secondary outcome is achieved by accelerating recovery time, improving overall neural function, and restoring tissue. Improvements are measured using follow-up exams and radiology scans post-MSC+ Therapy.
Treatment Prognosis
Challenges to the effective treatment of transverse Myelitis are related to how rapidly the disease progresses and the limitations of disease-modifying drugs. Much work remains to understand the pathogenesis of transverse myelitis fully. TM affects all age groups regardless of gender, family history, or race. Some patients may require aggressive immunosuppression but must be monitored for complications from immunosuppression. Stem cell therapy does offer an alternative; however, early intervention with consistent physical Therapy and rehabilitation will be needed for a healthy recovery.
TM Treatment Guidelines
Due to the varying degrees of existing medical conditions and the stage of inflammation, our medical team will need to review the potential candidate’s current medical condition before a treatment protocol can be established. Upon acceptance, we can provide a more accurate assessment of the patient’s condition and what we expect to achieve post-therapy. The final plan will include a daily treatment outline with the required days and the complete and fixed medical-related expenses (excluding accommodations or flights). Stem Cell Therapy for transverse myelitis using MSC+ cells will require a minimum of 10-16 days in Bangkok. To begin the qualification process for our multi-stage protocol, please prepare recent medical records and contact us today.
Published Clinical Citations
[1] ^Aungsumart, S., & Apiwattanakul, M. (2017). Clinical outcomes and predictive factors related to good outcomes in plasma exchange in severe attack of NMOSD and long extensive transverse Myelitis: Case series and review of the literature. Multiple sclerosis and related disorders, 13, 93–97. https://doi.org/10.1016/j.msard.2017.02.015
[2] ^Tradtrantip, L., Asavapanumas, N., & Verkman, A. S. (2020). Emerging therapeutic targets for neuromyelitis optica spectrum disorder. Expert opinion on therapeutic targets, 24(3), 219–229. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02482-2
[3] ^Krishnan, C., Kaplin, A. I., Deshpande, D. M., Pardo, C. A., & Kerr, D. A. (2004). Transverse myelitis: pathogenesis, diagnosis and treatment. Frontiers in bioscience : a journal and virtual library, 9, 1483–1499. https://doi.org/10.2741/1351
[4] ^Burman, J., Tolf, A., Hägglund, H., & Askmark, H. (2018). Autologous hematopoietic stem cell transplantation for neurological diseases. Journal of neurology, neurosurgery, and psychiatry, 89(2), 147–155. https://doi.org/10.1136/jnnp-2017-316271
[5] ^Lu, Z., Ye, D., Qian, L., Zhu, L., Wang, C., Guan, D., Zhang, X., & Xu, Y. (2012). Human umbilical cord mesenchymal stem cell therapy on neuromyelitis optica. Current neurovascular research, 9(4), 250–255. https://doi.org/10.2174/156720212803530708

