Neural stem cell therapy represents an emerging frontier in treating burst fractures, offering patients with burst fractures and Spinal cord compression injuries a potential alternative to conventional surgical interventions and back fracture surgery. The Regeneration Center applies various stem cell lineages and delivery methods to bypass the BBB. Our treatments include neural cell growth factors with strong regenerative and proliferative capacity needed for positive neurological recovery results. While our initial therapy outcomes have indicated positive outcomes, significant challenges remain regarding optimization protocols, delivery mechanisms, and long-term safety profiles. The complex interplay between cellular therapy and spinal trauma recovery warrants ongoing efforts. We encourage our patients to get multiple opinions from qualified doctors with experience in the application of stem cell therapy for spinal cord injuries.
1 Year After Stem Cells for Spinal Compression Fracture
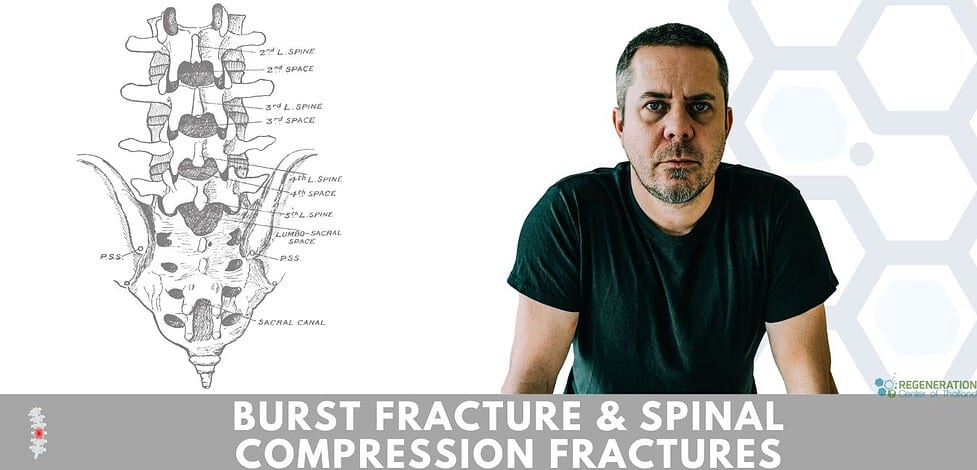
Understanding Burst Fractures: Causes and Impact
Understanding the nature of a burst fracture, which occurs when vertebral bodies experience severe axial compression, is crucial. This traumatic injury, often resulting from high-energy impacts, such as motor vehicle accidents, falls from heights, swimming, gunshot injuries, or sports-related trauma, can have significant implications for patient care. The biomechanical vulnerability of the thoracolumbar region makes it particularly susceptible to these injuries.
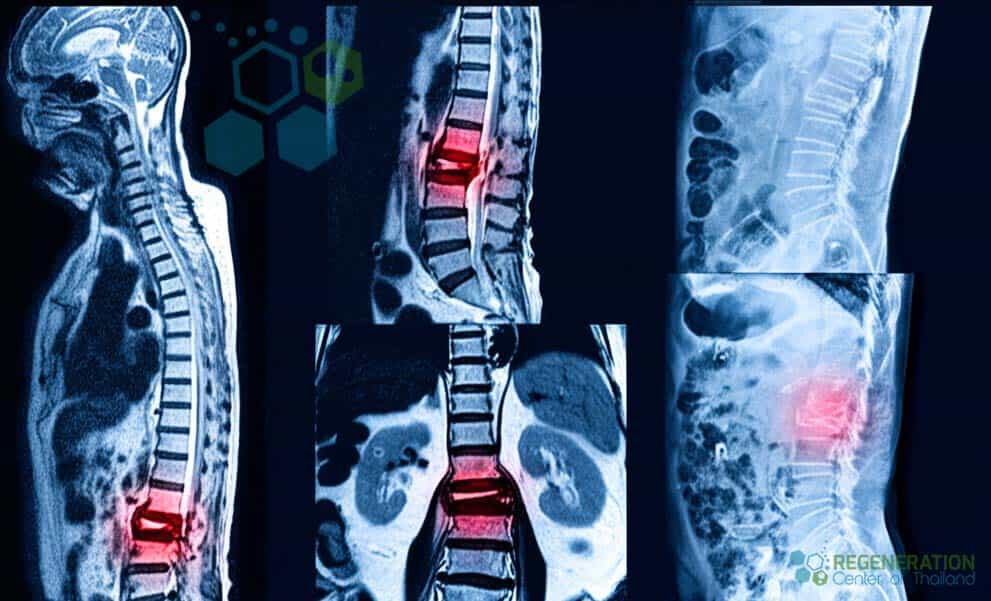
Risk factors include osteoporosis, prior vertebral fractures or degenerative disc disease, and participation in high-risk activities. Severity assessment evaluates neurological deficits, spinal canal  compromise, and vertebral body integrity. Radiological diagnosis through CT scans and MRI imaging reveals fragment displacement patterns and potential spinal cord involvement. Conservative management, incorporating bracing and rehabilitation protocols, may be appropriate for stable burst fractures without neurological compromise. However, unstable fractures with significant canal compromise or neurological deficits typically require surgical intervention. Understanding these factors is essential for healthcare providers to determine the most appropriate treatment strategies and improve patient outcomes.
compromise, and vertebral body integrity. Radiological diagnosis through CT scans and MRI imaging reveals fragment displacement patterns and potential spinal cord involvement. Conservative management, incorporating bracing and rehabilitation protocols, may be appropriate for stable burst fractures without neurological compromise. However, unstable fractures with significant canal compromise or neurological deficits typically require surgical intervention. Understanding these factors is essential for healthcare providers to determine the most appropriate treatment strategies and improve patient outcomes.
The Evolution of Traditional Treatment Methods
Over the past several decades, treatment approaches for burst fractures have undergone profound refinement, evolving from primarily conservative methods to increasingly sophisticated surgical interventions. The traditional protocols initially centered on extended bed rest and external bracing, coupled with extensive pain management techniques involving both pharmacological and physical therapy approaches.
The Regeneration Center Difference
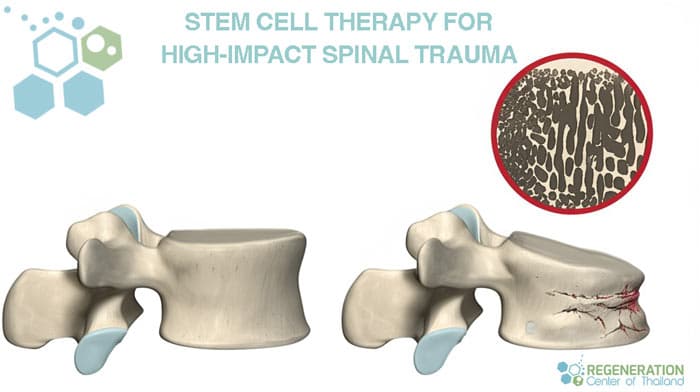
As our understanding has advanced, surgical intervention considerations have expanded to include various stabilization procedures, explicitly focusing on spinal fusion and instrumentation methods. These developments drastically impacted the rehabilitation timeline, reducing hospital stays and improving patient outcomes. The implementation of minimally invasive techniques further revolutionized the treatment landscape, offering reduced tissue trauma and accelerated healing potential. Long-term recovery protocols for burst fractures have evolved to incorporate evidence-based physical therapy regimens, structured mobility progression, and integrated pain management strategies. This systematic approach has enhanced patient recovery trajectories while minimizing complications and optimizing functional outcomes, providing reassurance to patients and their families about the comprehensive stem cell treatment for high-impact spinal trauma and burst fractures.
Mechanisms of Action for High-impact Spinal Trauma
High-impact spinal trauma involves complex biomechanical forces that converge upon vertebral structures, resulting in multi-directional stress patterns and subsequent structural failure. The primary mechanisms encompass axial compression, shear forces, and rotational torque, which disrupt the structural integrity of vertebral bodies and surrounding tissues. The cascade of physiological responses initiates immediately after trauma, triggering inflammatory mediators and cellular recruitment to the injury site. This acute phase critically influences subsequent tissue regeneration and biomechanical restoration processes. Healing mechanisms depend on cell differentiation pathways, particularly the activation of mesenchymal stem cells and their migration to damaged areas.
Local inflammation reduction occurs through multiple pathways, including modulating pro-inflammatory cytokines and releasing anti-inflammatory factors. These processes facilitate the natural progression of tissue repair while supporting the restoration of spinal column stability and neurological function.
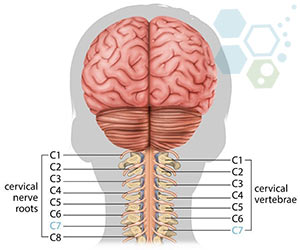
Types of Stem Cells Used for Cervical, Thoracic & Lumbar Injuries
Several distinct stem cell lineages have demonstrated therapeutic potential for patients with spinal injuries. Mesenchymal stem cells (MSCs) and neural stem cells (NSCs) are the primary candidates. MSCs can be derived from bone marrow, adipose tissue, placental tissue, or umbilical cord tissue (UC-MSC) and exhibit significant immunomodulatory and regenerative properties while raising minimal ethical concerns.
While embryonic stem cells possess remarkable pluripotency, their clinical application remains limited due to ethical considerations and tumor formation risks which is why they are not used by the Regeneration Center. Hematopoietic stem cells from cord blood are well-studied for treating blood disorders but have very restricted potential in spinal cord repair. Due to the various risks and benefits, the Regeneration Center offers a combination therapy from patient-specific somatic cells and differentiated into multiple neural cell types and growth factors needed for a balanced treatment approach.
Each stem cell type presents distinct advantages and limitations. MSCs demonstrate the most extensive clinical applications for our functional therapies and personalized medical approaches. The selection of stem cell lineages, growth factors, and infusion methods will depend on several factors, including injury severity, timing of intervention, and specific therapeutic objectives.
Spinal Compression Fracture vs Vertebral Burst Fracture
Structural differences between spinal compression and vertebral burst fractures manifest primarily in injury patterns and mechanical characteristics. Compression fractures typically involve vertical collapse of the anterior vertebral body, while burst fractures exhibit multi-directional fragmentation with retropulsion of bone fragments into the spinal canal.
Compression fractures generally preserve neurological function due to minimal canal compromise, though vertebral height restoration remains vital to prevent progressive degenerative changes. In contrast, burst fractures frequently threaten neurological integrity through canal stenosis and potential cord compression, necessitating urgent intervention.
The long-term implications also differ noticeably. Compression fractures may lead to gradual height loss and kyphotic deformity, potentially accelerating adjacent segment disease. When adequately treated, Burst fractures focus on immediate stabilization and decompression to maintain neurological function. Both conditions require careful biomechanical assessment to determine ideal treatment strategies and prevent further structural deterioration.
Therapeutic Benefits and Expected Outcomes
The therapeutic application of stem cell therapy in vertebral burst fractures has demonstrated promising outcomes across multiple clinical parameters. For patients with injuries less than 24 months old, our post-treatment follow-ups have shown measurable tissue regeneration within the fractured vertebrae, accompanied by enhanced recovery rates compared to conventional treatments. Patients typically report substantial pain reduction within the first three months post-treatment.
Improvements in mobility are documented through standardized functional assessments, with patients demonstrating an increased range of motion and reduced mechanical restrictions. The regenerative properties of stem cells facilitate the restoration of vertebral height and structural integrity, contributing to the long-term stability of the spinal column. Success rates vary based on age, injury severity, and overall health status, but data suggests positive outcomes in 45-65% of cases. Our therapy’s capacity to promote natural healing processes while minimizing surgical intervention significantly advances burst fracture treatment protocols.
Challenges and Limitations of Stem Cell Therapy
Despite our positive results, significant challenges persist in the clinical implementation of stem cell therapy for burst fractures, encompassing both technical and biological limitations. Among these, ensuring optimal cell viability during the culturing and delivery transplantation is particularly challenging, as stem cells are highly sensitive to environmental conditions, transportation stresses, and procedural manipulations, which can significantly diminish their regenerative potential. Additionally, achieving precise cell differentiation into bone-forming osteoblasts at the injury site remains challenging due to complex biological signaling pathways and unpredictable microenvironments in severely traumatized tissue.
Donor site morbidity represents another critical limitation, especially when harvesting autologous stem cells from bone marrow or adipose tissues. Procedures such as bone marrow aspiration or adipose tissue extraction can lead to complications, including infection, hematoma formation, persistent pain, and prolonged recovery times, thus impacting patient comfort and overall therapeutic acceptance.
TREATMENT RISKS & PRECAUTIONS
Not all patients are suitable candidates for treating burst fractures, thoracic spine injury, Lumbar vertebra fractures, or Spinal cord compression with stem cells. Patients with complete injuries, severe nerve compression, or multiple comorbidities may not be good candidates for estimated two-week treatment.Moreover, technical limitations involve challenges in accurately delivering stem cells to the exact location of the burst fracture and ensuring their retention and survival at the injury site. Poor cell retention may necessitate multiple treatments, increasing procedural complexity, patient discomfort, and associated costs. Furthermore, biological variability between patients significantly influences treatment outcomes. Differences in age, health status, genetic background, and underlying comorbidities can result in inconsistent therapeutic efficacy. Addressing these technical and biological hurdles is crucial for enhancing stem cell therapy’s safety and effectiveness in managing burst fractures.
UC-MSC+ Cells for Spinal Compression Fracture
At What Age Is Stem Cell Treatment Most Effective for Burst Fractures?
Based on our previous cases and clinical trials, the ideal patient age for stem cell treatment effectiveness typically ranges between 20 and 50 years. Endogenous stem cell populations and regenerative capacity remain maximal during this period, contributing to enhanced recovery speed. Long-term efficacy evaluation suggests younger patients achieve superior outcomes, though stem cell selection and expansion methods can compensate for age-related decline. However, individual factors such as overall health status and injury severity ultimately influence treatment success more than age alone.
Stem cell therapy demonstrated significant potential for treating burst fractures, offering enhanced regenerative capabilities compared to conventional treatments. Current evidence supports its efficacy in promoting bone healing and neurological recovery. While technical challenges persist regarding standardization and long-term safety protocols, continued research and regulatory refinement will likely establish stem cell interventions as a viable therapeutic option for severe vertebral trauma patients.
Stem Cell Treatment for Thoracic Spine Injury & Vertebral Burst Fracture
The total number of cell infusions for Traumatic Spine injury will depend on the patient’s needs. Most patients require multiple infusions of expanded mesenchymal (UC-MSC+) cells per session. Older injuries or patients with neurological deficits due to spinal injury may require several stages for meaningful recovery.
Types of Stem Cells Used and Delivery Methods: Patients with lumbar vertebra fracture, spinal compression fracture, spinal fusion after burst fracture, thoracic spine injury, and spinal cord compression will require multiple sessions of clinical grade expanded UC-MSC+ Mesenchymal cells along with our proprietary mix of cell isolated growth factors that include Vascular Endothelial Growth Factors (VEGF), Insulin-like Growth Factor-1 (IGF-1), Transforming Growth Factor-beta (TGF-β), Connective Tissue Growth Factors (CTGF), Bone Morphogenetic Proteins (BMPs), Fibroblast Growth Factors (FGF), Platelet-Derived Growth Factors (PDGF), Epidermal Growth Factors (EGF), and Nerve Growth Factors (NGF). We offer allogenic and autologous protocols depending on the patient’s age and type of injury. The autologous protocols require multiple trips over 2 months, with 2 to 4 weeks of cell expansion needed before the cell populations can be used, while the allogeneic UC-MSC+ protocol does additional wait times and can be completed in less than two weeks. The isolated stem cells and growth factors used in our treatments are delivered via a combination of methods, including intravenous drips (IV), direct local injections, intrathecal injections, intradiscal injections, fluoroscopy-guided stem cell delivery (in a hospital setting only), to achieve the best results. To learn about the basics of stem cells, visit here.
Cost of Stem Cells for Cervical, Thoracic or Lumbar Fractures
The treatment scale and scope at our stem cell treatment center will depend entirely on the severity of the type of Injury and the patient’s actual medical needs. Our outpatient treatment will require an estimated 14-31 day treatment in Bangkok, Thailand. To evaluate your suitability for spinal cord compression and burst fracture therapy, we must review the patient’s current lab results, including radiology scans (MRI, PET, CT scans) and supporting lab results. Once the patient’s medical information is reviewed, we will provide a comprehensive treatment plan with fixed-cost pricing. The final therapy plan will include all associated medical costs, hospital fees (if applicable), post-treatment rehabilitation (if applicable), doctor’s fees, lab work, stem cell collection, and cell expansion. Additionally, we offer short-term wheelchair-accessible serviced apartment options for patients and their families.
To learn more about our unique combination (UC-MSC+) stem cell therapy for spinal compression fracture & alternatives to back fracture surgery, please contact us today