We all know what happens when you get a cut. It gets red. It hurts. It might swell or even become extremely warm. While there are certainly more severe cases, this is a typical example 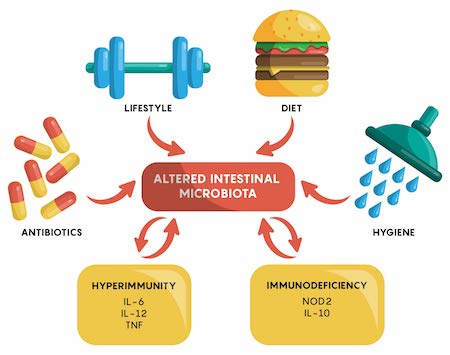 of inflammation. Inflammation is part of your body’s natural healing process. When the body detects an injury, infection, or toxic substance, it sends white blood cells and cytokines to the area to repair the problem and fight off pathogens to support your recovery. This process can cause temporary discomfort in the form of redness and swelling.
of inflammation. Inflammation is part of your body’s natural healing process. When the body detects an injury, infection, or toxic substance, it sends white blood cells and cytokines to the area to repair the problem and fight off pathogens to support your recovery. This process can cause temporary discomfort in the form of redness and swelling.
Not all inflammation is helpful, though. Your body may run into trouble if it mistakes something normal for an injury or infection. Autoimmune diseases like lupus or arthritis are examples of this. The body mistakes its healthy cells for foreign ones. When it attacks those healthy cells, it may cause unnecessary inflammation and injury.
When the immune system overreacts like this, the body may maintain a low level of inflammation. Studies have linked chronic, low-grade inflammation like this to conditions such as inflammatory bowel diseases, multiple sclerosis, atherosclerosis (fatty deposits in the arteries), cardiovascular disease, eczema, rheumatoid arthritis and psoriasis. Inflammation may also play a role in autoimmune disease, type 1 diabetes, weight gain, pancreatitis and brain function. Learn more about foods that help fight inflammation.
Is inflammation good for healing?
Inflammation plays a crucial role in the wound-healing process, which is intricately orchestrated and involves multiple phases: inflammatory, proliferative, and remodelling. The initial inflammatory phase is essential for wound healing, as it helps to clear the wound of debris and pathogens and sets the stage for tissue repair. During this phase, the body’s immune response is activated, leading to the recruitment of leukocytes, including neutrophils and monocytes, to the wound site. These cells release cytokines and growth factors that promote the healing process.
Moreover, inflammation is associated with the recruitment of fibroblasts and the production of extracellular matrix components, such as collagen, during the proliferative phase. This results in granulation tissue formation and is crucial for the subsequent remodelling of the wound. The recruitment of vascular endothelial cells, stimulated by factors like VEGF, PDGF, and TGF-b, leads to angiogenesis, further supporting the healing process.Stem cells, including mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), play a significant role in modulating inflammation and promoting tissue repair. MSCs, for example, can exert anti-inflammatory effects by modulating immune responses, thus supporting healing. They can inhibit natural killer and cytotoxic T-cells and induce T-cell apoptosis, reducing inflammatory response and promoting a more regenerative environment.
Therefore, while inflammation is a critical and necessary component of the initial wound healing stages, its regulation is essential to prevent chronic inflammation, which can lead to impaired healing or excessive scarring. The balance and transition from inflammation to the proliferative and remodelling phases are crucial for effective healing and minimizing scar formation. Stem cells contribute significantly to this process by supporting tissue repair and regeneration and modulating the inflammatory response to ensure a conducive healing environment.
The Gut Microbiome & Inflammation
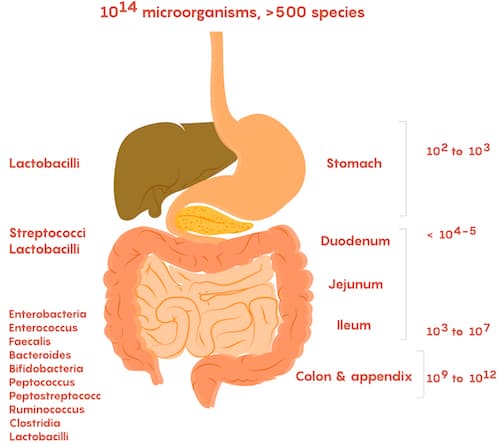 The gut has also shown to help regulate your body’s response to possible threats and system wide inflammation. Certain beneficial microbes in the gut produce anti-inflammatory molecules known as short-chain fatty acids (SCFAs) when they digest and ferment fiber. SCFAs can enter the bloodstream, where they can help regulate inflammation outside of the gut. While what you need to support your microbiome may differ from your friends and family, there are three microbe-produced molecules that may play a role in regulating inflammation in your body:
The gut has also shown to help regulate your body’s response to possible threats and system wide inflammation. Certain beneficial microbes in the gut produce anti-inflammatory molecules known as short-chain fatty acids (SCFAs) when they digest and ferment fiber. SCFAs can enter the bloodstream, where they can help regulate inflammation outside of the gut. While what you need to support your microbiome may differ from your friends and family, there are three microbe-produced molecules that may play a role in regulating inflammation in your body:
- Propionate
- Butyrate
- Polyamine.
Healing with Stem Cell: Impact on Inflammation
Healing wounds from injury is a complex process requiring a coordinated biochemical response to achieve complete tissue closure. For adults, the healing process results in scar formation, which acts as a chemical and physical barrier but is part of the standard repair cycle. Fetal healing occurs when damaged tissue is replaced without the formation of scar tissue and involves minimal inflammation.
Therefore, doctors practicing functional medicine have often targeted inflammation as a way to emulate the environment where fetal healing occurs. Doctors typically start with dressing the wounded areas and then move through various treatment options with increasing complexity depending on the patient’s healing response. Learn about elements in the human body.
This progressive treatment protocol often fails to mimic the natural healing processes that occur in an in-vivo setting. Wound care research has resulted in enormous new products, devices, scaffoldings, and cell-based therapies. Still, only 55–75% of the wounds healed properly within the randomized controlled clinical trials.
Isolated mesenchymal stem cells offer a unique treatment option that is dramatically different from current treatment options. MSC+ stem cells can be introduced inside scaffoldings (torn rotator cuffs) by direct injections or topically to work within the microenvironment and influence the natural healing process in a much more regenerative way through the paracrine function.