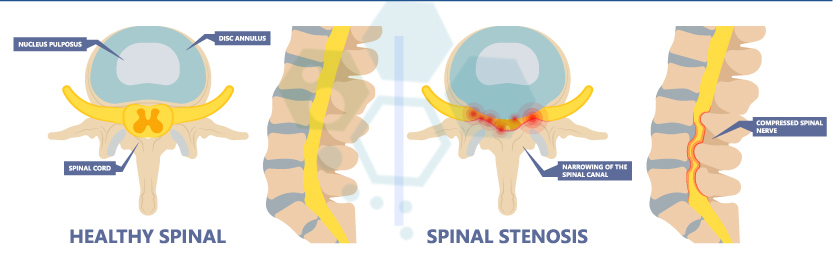
Spinal Stenosis is a medical condition characterized by the narrowing of the spinal canal, which results in increased pressure on the spinal cord and nerve roots. This condition can be congenital or develop over time due to age-related changes in the spine, such as bone spurs and thickened ligaments. Depending on where it occurs, it can cause pain, numbness, and weakness in various body parts.
Symptoms associated with Spinal Stenosis
The most common symptoms associated with spinal Stenosis include pain and numbness along the back or legs that worsens with standing or walking and is relieved after sitting down or leaning 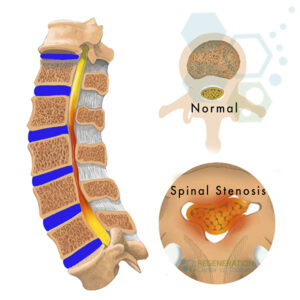 forward; tingling sensations in the arms; muscle weakness in the legs leading to difficulty walking for long distances; fatigue due spinal stenosis; urinary incontinence and constipation (IBD), mctd and headaches [1]. For some patients with FMS, ligament injuries, hip injuries, and shoulder and knee injuries, the pain can also radiate outwards from where it is seen or experienced most commonly, making it difficult to complete daily activities.
forward; tingling sensations in the arms; muscle weakness in the legs leading to difficulty walking for long distances; fatigue due spinal stenosis; urinary incontinence and constipation (IBD), mctd and headaches [1]. For some patients with FMS, ligament injuries, hip injuries, and shoulder and knee injuries, the pain can also radiate outwards from where it is seen or experienced most commonly, making it difficult to complete daily activities.
Causes of Spinal Canal Stenosis
Potential causes of spinal Stenosis can include other age-related changes like herniated discs, arthritis formation within joints, thickening of ligaments, a buildup of bony growths (bone spurs) that pinch nearby nerves, trauma such as an injury causing misalignment in vertebrae, which can decrease available space or diseases like Paget’s disease which involves excessive bone growth. Additionally, tumors and cysts may contribute to reduced areas for nerve pathways within the spine.
Symptoms of Lumbar spinal stenosis
Symptoms of spinal stenosis can vary depending on the severity of the condition and where it is located. Some common symptoms include pain in the lower back, buttocks, or thighs; cramping in the legs or arms; weakness or numbness in the legs, arms, hands, or feet; tingling sensation in the back or extremities; difficulty walking for long distances; balance issues such as feeling unsteady when turning or bending.
Potential causes of Spinal Stenosis include bulging discs, bone spurs (osteophytes) developing on either vertebral facet joints, hypertrophy of surrounding ligaments like the supraspinous ligament, and intraspinal enlargements from tumors or nerve entrapment. In addition to these causes specifically causing spinal stenosis, other conditions like sarcopenia, osteoarthritis, and lumbar spondylolisthesis have been linked with stenosis development through their mechanical effects on nerves [2].
When the spinal column narrows, it may press on the spine, compressing the root or femoral nerves and resulting in pain. Causes for a diagnosis can vary greatly, ranging from genetics to activity level to age-related wear and tear. Other potential risk factors for spinal Stenosis include previous injuries (especially from a fall), ankylosing spondylitis, metabolic diseases, diminishing bone density as we age (osteoporosis), scoliosis, arthritis, tumors, and viral or bacterial infections such as Lyme disease. A history of being born with a congenitally narrow spinal canal is also associated with a higher risk of developing the condition later in life.
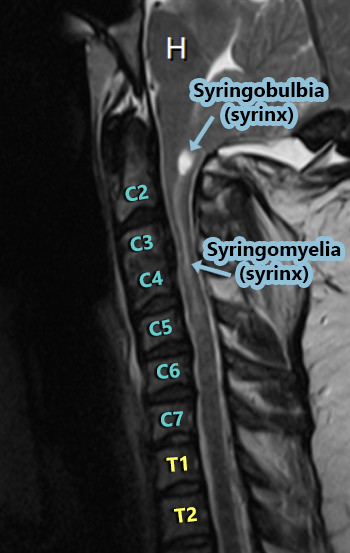
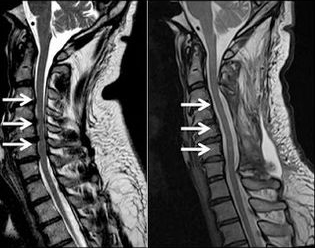
Diagnosing Cervical Spinal Stenosis
Diagnosis of spinal stenosis in the cervical (neck area) or lumbar (lower back) can be made through various means, including physical examination, imaging tests (CT scan and MRI scan), myelogram, electrical studies (nerve conduction tests), and musculoskeletal tests. During the initial physical examination, your orthopedic doctor may check the limbs for reflexes and strength. Patients are tested performing simple neurological tasks. Imaging scans are also used to identify bone structure compression or narrowing. Types of radiology scans can include X-rays, MRI scans, CT scans, and Ultrasound. MRI scans are beneficial for cross-sectional images using magnetic fields and radio waves.
In some cases, a myelogram may also be ordered, requiring contrast dye to determine if there are any blockages in the area. Non-invasive electrical studies and nerve conduction tests can be used to assess how well nerves respond to stimuli. At the same time, biochemistry tests can check for evidence of infections or inflammation, as secondary infections have been known to cause spinal stenosis.
Current Treatments for Spinal Stenosis
Depending on the stage and severity, doctors may recommend certain lifestyle modifications, such as physical therapy, to help enhance overall strength and flexibility and reduce inflammation in tissues around your spine. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to help reduce pain and swelling for patients. Steroids could be used if more severe inflammation is found, accompanied by spasms throughout surrounding muscles. In some cases, surgery may be suggested to increase available nerve paths, alleviating pressure caused by spinal Stenosis. Surgery may require rods or screws combined with fused vertebrae sections.
Non-surgical treatments may include:
- Physical therapy—Physical therapy can involve manual manipulation, massage, ultrasound, and stretching. It is often used to reduce pain, improve flexibility and strength in the lumbar spine, and promote better posture.
- Medications – Nonsteroidal anti-inflammatory drugs (NSAIDs) are generally prescribed to reduce inflammation in the abdomen and around the spine. Oral corticosteroids can also be prescribed to minimize epidural swelling and provide short-term relief from spinal stenosis symptoms. Your physician may also offer additional medications, such as muscle relaxants or narcotics, for temporary pain relief on an as-needed basis [3]
- Support Devices—Braces or supports for the neck or lower back can be worn to help relieve pressure over time. They will maintain proper posture, encourage healing by improving circulation around affected areas, help relieve muscle spasms and pain levels, and further restrict movement of the discs within the vertebral column.
- Biologic therapies (Protein-based therapies) -Biological therapies use the body’s natural healing mechanisms to regenerate or repair damaged tissues. One such example is Platelet-Rich Plasma (PRP) therapy. In PRP therapy, a patient’s blood is spun in a centrifuge to concentrate the platelets, which are then re-injected into the area of injury or degeneration. Platelets are a source of growth factors, proteins that help stimulate healing. Another potential protein-based treatment is using bone morphogenetic proteins (BMPs). These proteins form bone and cartilaginous tissue and have been used to promote spinal fusion in some patients. Similarly, other growth factors like transforming growth factor-beta (TGF-beta) and fibroblast growth factors (FGFs) might also be utilized in some therapeutic protocols.
Treatment for Lumbar & Cervical Spinal Stenosis
Surgery for Spinal Stenosis
Surgical treatment options may include:
- Micro endoscopic Discectomy. This minimally invasive procedure involves removing a portion of a herniated disc with specialized instruments guided by an endoscope containing a fiberoptic light source and a camera clip that passes through small incisions in your back muscles between vertebrae to access the spine.
- Spinal Fusion – This procedure uses rods or screws attached to bone grafts across multiple vertebrae to immobilize them together. Hence, they heal into one solid piece of bone while allowing some minimal movement at the level above or below it.
- Laminectomy – This procedure removes all or part of the lamina, making more room for nerves exiting your spinal canal, and relieves any pressure caused by spinal stenosis that is pinching nerves or causing pain.
Stem cell therapy for Spinal Stenosis
For many patients, stem cell therapy offers a non-surgical alternative to treat degenerative discs and spinal stenosis has been proven to show improvements in several areas. Depending on patient needs, stem cells from different sources (autologous vs. allogeneic) have varying degrees of effectiveness in promoting differentiation and producing desired biological effects. Since 2007, The Regeneration Center has developed a deep understanding of stem cell therapies for low back pain (LBP), Intervertebral disc degeneration (IDD), acute spinal injuries, spinal stenosis, and intervertebral disc herniation.
Isolated and expanded stem cells have been used to intervene in spinal stenosis and inflammation to help slow down progression, boost stem cell production, and achieve repair through cell regeneration. The Regeneration Medical Center currently offers several types of cell therapies, including:
- Mesenchymal stem cells (MSC+)
- Intervertebral disc-derived stem cells (IVDSC+)
- Adipose-derived mesenchymal stem cells (ADMSC+)
- Bone marrow mesenchymal stem cells (BMSC+)
- Umbilical cord mesenchymal stem cells (UCMSC+)
- Nucleus pulposus stem cells (NPSC+)
- Annulus fibrosus stem cells (AFSC+)
- Cartilage endplate stem cells (CESC+)
Stem Cells for Lumbar Spinal Stenosis 
The three primary functions of regenerative stem cells are:
- They can initiate cell signaling to differentiate into intervertebral disks (IVD-like cells, chondrocyte-like cells, or IVD chondrocytes).
- Stem cell transplants can help support the viability of existing resident cells near the implantation site. These cells are delivered using multiple types of growth factors, chemokines, ECM components, and anti-inflammatory substances through paracrine mechanisms [4].
- Stem cell transplants help the patient’s immune regulation by increasing pro-inflammatory cytokines to promote angiopoietins, chemotaxis, and release of cytokines. When used correctly, they can help produce anti-inflammatory cytokines and growth factors and act as anti-metabolic mediators to modulate the immune response, which is vital for cases with osteoporosis.
Spinal Stenosis Surgery Alternative
Types of Stem Cells and Delivery Methods: Multiple Sessions of Enhanced UC-MSC+ Mesenchymal Cells & spinal regenerative therapy protocol will depend on the underlying stage’s severity and the patient’s condition. Our clinical grade lab cell-enriched allogeneic cell protocols cells do not require any invasive surgeries. The cells are delivered via intravenous drips, direct local injections, intradiscal injections, intrathecal injections, fluoroscopy-guided stem cell delivery (in a hospital setting only), or a combination of different delivery methods to achieve the best results. To learn about the basics of stem cells, visit here[5].
Cervical Stenosis Treatment Guidelines – 2025
Safety and efficacy are as important as results; therefore, our unique multi-stage cellular therapy for spinal stenosis will require 1-2 Weeks in Bangkok, Thailand. Due to the varying degrees of spinal damage experienced by each patient, our orthopedic team will need to evaluate potential candidates. Upon completion of the evaluation, a detailed treatment plan will be provided. It will include specific recommendations such as a day-by-day treatment calendar (appointment dates), total nights required, and fixed medical costs (excluding accommodations or flights). To begin the treatment evaluation, please prepare recent medical records such as (MRI or CT Scans) and contact us today.
Post-Treatment Physical Rehabilitation & Pain Relief: For patients with Cervical Stenosis with myelopathy, Ankylosing spondylitis (spinal stenosis), or osteoporosis, physical rehabilitation after your treatment f is optional depending on travel limitations. Total post-therapy rehab plans are also available for 2-4 hours per day and up to 5 days per week. We also offer complete regenerative medical packages, assistance with medical visas, and extended stay accommodations for the patient + family upon request.
Published Clinical Citations
[1] ^Kasai Y, Paholpak P, Wisanuyotin T, Sukitthanakornkul N, Hanarwut P, Chaiyamoon A, Iamsaard S, Mizuno T. Incidence and Skeletal Features of Developmental Cervical and Lumbar Spinal Stenosis.Intermittent Neurogenic Claudication Asian Spine J. 2022 May 10. doi: 10.31616/asj.2022.0015. Epub ahead of print. PMID: 35527532.
[2] ^Lee JY, Whang PG, Lee JY, Phillips FM, Patel AA. Lumbar spinal stenosis. Instr Course Lect. 2013;62:383-96. PMID: 23395043.
[3] ^Chaimongkhol T, Thiamkaew A, Mahakkanukrauh P. The characteristics of osteophyte around lumbar vertebral foramina associated with spinal stenosis. Anat Cell Biol. 2019 Jun;52(2):143-148. doi: 10.5115/acb.2019.52.2.143. Epub 2019 Jun 30. PMID: 31338231; PMCID: PMC6624344.
[4] ^ Vadalà G, Ambrosio L, Russo F, Papalia R, Denaro V. Stem Cells and Intervertebral Disc Regeneration Overview-What They Can and Can’t Do. Int J Spine Surg. 2021 Apr;15(s1):40-53. doi: 10.14444/8054. Epub 2021 Apr 21. PMID: 34376495; PMCID: PMC8092931.
[5] ^ Sivakamasundari V, Lufkin T. Stemming the Degeneration: IVD Stem Cells and Stem Cell Regenerative Therapy for Degenerative Disc Disease. Adv Stem Cells. Halo Vest vs. Spinal Fusion 2013;2013:724547. doi: 10.5171/2013.724547. PMID: 23951558; PMCID: PMC3742038.