Alcoholic hepatitis is a severe form of liver disease that arises from excessive alcohol consumption, representing a significant public health concern that impacts millions of individuals worldwide. The Regeneration Center would like to shed some light on the complexities of alcoholic hepatitis, exploring its causes, symptoms, diagnosis, and current treatment approaches. Furthermore, we will look into the promising role of umbilical cord-derived mesenchymal stem cell therapy as a potential treatment avenue for this challenging condition, examining the latest research and potential benefits this innovative non-surgical approach holds.
What is Alcoholic Hepatitis?
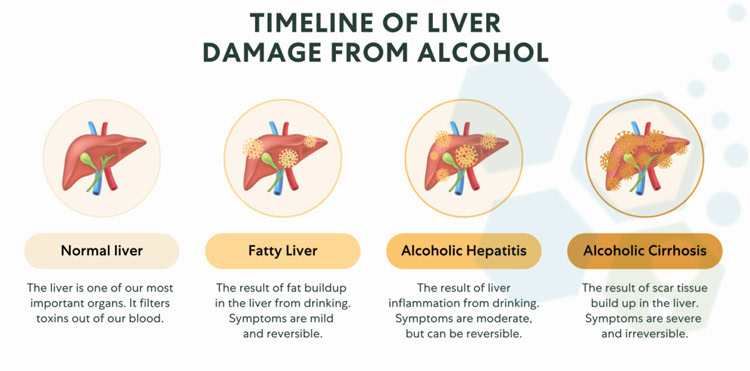
Alcoholic hepatitis (AH) is a specific type of alcohol-related liver disease characterized by inflammation of the liver and decompensated liver cirrhosis. This inflammation isn’t simply a mild reaction; it signifies significant damage to liver cells (hepatocytes), impairing the liver’s ability to perform its vital functions, such as filtering toxins from the blood, producing bile for digestion, and storing essential nutrients. Unlike some other forms of alcoholic liver disease that develop gradually over decades, AH can develop rapidly, sometimes within weeks of heavy drinking.[1]
The severity of AH can vary greatly, with some individuals experiencing mild, short-lived symptoms while others develop severe liver fibrosis and acute-on-chronic liver failure that can be life-threatening. The unpredictable nature underscores the seriousness of the condition and the importance of early diagnosis and therapeutic intervention.
Causes of Alcoholic Hepatitis
While excessive and prolonged alcohol consumption is the primary cause of alcoholic hepatitis, it’s not as simple as saying everyone who drinks heavily will develop the disease. Individual susceptibility plays a significant role, with genetics playing an essential part. This is also true when considering treatments like human mesenchymal stem cells for liver repair. Certain gene variations, particularly those involved in alcohol metabolism, can make individuals more vulnerable to the toxic effects of alcohol on the liver. For example, variations in genes encoding alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) enzymes, responsible for breaking down alcohol in the body, can influence the risk of developing AH.
Genetic Testing for Liver
 The Regeneration center and our functional medical programs offer a comprehensive list of DNA testing options to test for inheritable liver & glycogen storage diseases, including the following panels: ATP7B, SPG70, JAG1, NOTCH2, ILLD, METRS, MRS, FBP1, SLC5A1, SLC2A2, PHKA2 G6PC, GBE1,SLC37A4, PYGL GYS2, PHKB, PHKG2,FBP, FBPase 1 & RpL17
The Regeneration center and our functional medical programs offer a comprehensive list of DNA testing options to test for inheritable liver & glycogen storage diseases, including the following panels: ATP7B, SPG70, JAG1, NOTCH2, ILLD, METRS, MRS, FBP1, SLC5A1, SLC2A2, PHKA2 G6PC, GBE1,SLC37A4, PYGL GYS2, PHKB, PHKG2,FBP, FBPase 1 & RpL17
Beyond genetics, other factors contribute to the development of AH. Gender is a factor, with women appearing to be more susceptible to alcohol-induced liver damage at lower levels of consumption compared to men. This difference may be attributed to variations in alcohol metabolism, body composition, and hormonal factors between genders. Ethnicity also seems to play a role, with certain ethnic groups potentially experiencing a higher risk of AH. For instance, individuals of Hispanic/Latino descent may be more susceptible to AH, even with lower levels of alcohol consumption, compared to other ethnicities.[2]
Furthermore, the overall health of the liver before heavy drinking begins is crucial. Individuals with pre-existing liver conditions, such as fatty liver disease (hepatic steatosis) or hepatitis C, are significantly more vulnerable to developing AH. Fatty liver disease, often associated with obesity, metabolic disorders, autoimmune disease, pancreatitis and diabetes, can progress to inflammation and fibrosis, making the liver more susceptible to alcohol-induced damage. Hepatitis C, a viral infection affecting the liver, can also lead to chronic inflammation and scarring, further increasing the risk of AH. Nutritional deficiencies can exacerbate alcohol’s effects on the liver, as can the co-abuse of other substances, such as certain medications or illicit drugs. These substances can put additional stress on the liver, compounding the damage caused by alcohol and potentially complicating a patients ability to benefit from stem cell therapy for liver failure.
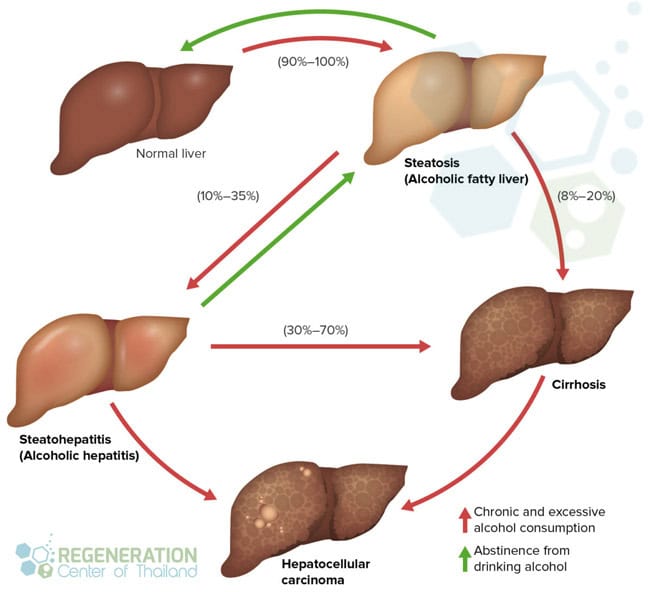
Alcoholic Liver Cirrhosis
After extended alcohol use, healthy liver tissue can be slowly replaced by atrophied, or thinning scar tissue. When this scar tissue builds up on your the, it can impede normal liver function and is categorized as liver cirrhosis. Severe liver cirrhosis is irreversible but the combination of abstinence and liver stem cell therapy may be able to contain the disease and slow the progression. If liver cirrhosis goes untreated, it will lead to end stage liver failure.
Recognize the Symptoms of Alcoholic Hepatitis
Alcoholic hepatitis presents a wide range of symptoms, often making it difficult to diagnose in its early stages. Some individuals may be completely asymptomatic, unaware of the damage being inflicted upon their liver. This silent progression makes regular medical checkups, and liver function tests essential for individuals with a history of heavy alcohol use. When symptoms do appear, they can range from mild and general to severe and life-threatening, necessitating comprehensive treatments that might include cell therapy for liver disease.
One of the most noticeable symptoms is jaundice, a yellowing of the skin and the whites of the eyes, which may also indicate the need for advanced treatments like cell therapy for liver disease. Jaundice occurs due to a buildup of bilirubin, a yellow pigment produced during the breakdown of red blood cells in the blood. Typically, the liver processes bilirubin, making it water-soluble and excreted in bile. However, a damaged liver with cirrhosis can’t perform this function effectively, leading to its accumulation in the blood and deposition in tissues, causing yellow discoloration. Fatigue is a common symptom, often described as a persistent lack of energy not relieved by rest.[3]
This profound tiredness can significantly impact daily life, exhausting even simple tasks. It arises from the liver’s impaired ability to convert stored energy into usable energy, leading to a constant low energy state. Loss of appetite is another warning sign, often accompanied by unexplained weight loss. This reduced desire to eat can be attributed to a combination of factors, including liver dysfunction, hormonal imbalances, and a buildup of toxins in the blood that can suppress appetite.
Digestive symptoms are frequent, with nausea and vomiting being common complaints. These symptoms stem from the liver’s diminished capacity to process toxins and produce bile, leading to digestive issues such as IBD and Crohn’s disease. As AH progresses, individuals may experience abdominal pain, particularly in the upper right quadrant, where the liver is located. This pain can range from a dull ache to sharp, stabbing sensations. The pain often worsens with movement or deep breathing and can be exacerbated by the accumulation of fluid in the abdomen (ascites). Fluid retention, frequently manifesting as swelling in the legs, ankles, and abdomen (ascites), can also occur due to the liver’s inability to regulate fluid balance. The damaged liver can no longer effectively produce albumin, a protein essential for maintaining average fluid balance in the body, leading to fluid leakage into tissues.
Diagnosing Alcoholic Hepatitis
Diagnosing alcoholic hepatitis is a multifaceted process that requires a comprehensive evaluation by a healthcare professional. No single test definitively diagnoses AH, so physicians rely on a combination of clinical findings, lab results, and imaging studies to make an accurate diagnosis. The diagnostic journey typically begins with a thorough medical history review. A physician will inquire about the individual’s alcohol consumption habits, asking about the quantity and frequency of alcohol intake. They’ll also assess drinking patterns over time, as even periods of abstinence interspersed with heavy drinking episodes can contribute to AH.
Hepatologist will look into the individual’s overall health history, including any pre-existing conditions, family history of liver disease, medications, and other lifestyle factors. This detailed history helps paint a comprehensive picture of the individual’s risk factors for AH and provides valuable clues for diagnosis.
A physical examination is the next step. The physician will look for physical signs of alcoholic liver disease, such as jaundice, fluid retention in the legs or abdomen, brain fog, and tenderness in the upper right abdomen where the liver is located. Additionally, the potential for stem cell therapy for liver disease might be discussed depending on the condition’s severity. They may also assess for other signs of chronic liver disease, such as enlarged blood vessels on the skin (spider angiomas), redness of the palms (palmar erythema), or changes in the shape of the fingernails (clubbing). These physical findings, while not specific to AH, can indicate advanced liver disease.
Blood tests are crucial for evaluating liver function. Liver function tests (LFTs) measure the levels of certain enzymes and proteins in the blood that can indicate liver damage or inflammation. Elevated levels of liver enzymes, such as AST (aspartate aminotransferase) and ALT (alanine aminotransferase) can indicate liver injury. These enzymes are typically found inside liver cells, and their presence in elevated amounts in the blood suggests cell damage and leakage. Doctors will also check bilirubin levels, with elevated levels suggesting impaired bilirubin processing by the liver, a common finding in AH. This may prompt consideration of new treatments like mesenchymal stromal cell therapy. Other blood tests may include a complete blood count (CBC) to check for anemia and platelet count abnormalities, which can occur with liver dysfunction, and coagulation tests (INR, PT) to assess the liver’s ability to produce clotting factors.
Imaging studies provide a visual representation of the liver, allowing physicians to assess its size, shape, and any structural abnormalities. Ultrasound is often the initial imaging test, providing a quick and non-invasive way to visualize the liver. It can detect signs of fatty liver disease, inflammation, and cirrhosis (scarring). If abnormalities are detected on ultrasound, further imaging with CT scans or MRI may be recommended to provide more detailed images and assess the extent of liver damage. In some cases, a liver biopsy may be necessary to confirm the diagnosis and assess the severity of alcoholic hepatitis. A liver biopsy involves obtaining a small sample of liver tissue, usually through a needle inserted through the skin and into the liver under ultrasound guidance. A pathologist examines The tissue sample under a microscope to look for characteristic signs of AH, such as inflammation, cell death (necrosis), and fibrosis (scarring). The biopsy can also help determine the stage of liver damage which is useful when making treatment decisions.
Traditional Treatments for Alcoholic Hepatitis
The first and most vital step in treating alcoholic hepatitis is complete and permanent abstinence from alcohol. This means no amount of alcohol is considered safe. Continued alcohol consumption, even in small amounts, will worsen liver damage and significantly decrease the effectiveness of all treatments, including interventions like mesenchymal stem cells for alcoholic liver disease. It is important for patients with AH to completely eliminate alcohol from their lives to prevent further acute liver injury and improve their chances of recovery.
Alongside abstinence, nutritional support is paramount. A healthy, balanced diet that is rich in calories and protein is essential for supporting liver regeneration. Malnutrition is common in individuals with AH, often due to a combination of poor dietary intake, malabsorption of nutrients, and increased metabolic demands. Dietary interventions usually involve working with a registered dietitian to develop a tailored meal plan that meets the individual’s nutritional needs. This plan typically includes increasing calorie and protein intake, ensuring adequate intake of vitamins and minerals, and limiting sodium and fluid intake if fluid retention is present.
Medications for ARLD
Medications play a role in managing alcoholic hepatitis and its complications. Corticosteroids, such as prednisolone, are often prescribed to reduce liver inflammation. These medications work by suppressing the immune system’s inflammatory response, which helps to reduce liver injury. However, corticosteroids also come with potential side effects, including weight gain, increased risk of infections, and developing osteoporosis, so their use must be carefully monitored. The decision to use corticosteroids is typically based on the severity of AH, with more severe cases often benefiting from their use.
Other medications may be prescribed to manage specific complications of AH. Diuretics can help reduce fluid retention (ascites) by increasing urine output and removing excess fluid from the body. Antibiotics can treat bacterial infections, which are more common in individuals with compromised liver function. The liver plays a crucial role in fighting infections, so a damaged liver can make individuals more susceptible to bacterial infections. In cases of severe alcoholic hepatitis that don’t respond to medical management, a liver transplant may be the only life-saving option. Liver transplantation involves surgically replacing the damaged liver with a healthy liver from a deceased donor. However, liver transplantation is a significant procedure with its risks and benefits, and not all individuals with AH are eligible for transplantation. Factors considered for transplantation include the severity of liver disease, overall health status, and the individual’s commitment to abstaining from alcohol after transplantation.
Liver Stem Cell Therapy: A New Frontier
Stem cell therapy represents a revolutionary approach to treating various diseases, and its potential in addressing liver conditions like alcoholic hepatitis is fascinating. Stem cells for alcoholic cirrhosis offer a unique ability to differentiate into multiple cell types within the body, including liver cells. This characteristic makes them an up-and-coming tool for regenerating damaged tissues, offering hope for restoring liver function in individuals with AH. Unlike traditional treatment approaches that focus on managing symptoms and preventing further damage, stem cell therapy holds the potential to repair and regenerate damaged liver tissue directly.
After Treatment of Liver with Stem Cells
Mesenchymal Stem cells to alleviate liver injury
The mechanisms by which stem cells can potentially treat alcoholic hepatitis are multifaceted and still under investigation. However, early research suggests several promising avenues:
- Liver Cell Regeneration: Stem cells, when introduced into the damaged liver, can differentiate into new, functional liver cells (hepatocytes). This process can directly replace dead or dying liver cells, promoting tissue repair and restoring lost liver function. The ability of stem cells to integrate into the existing liver architecture and establish functional connections with surrounding cells makes them ideal candidates for liver regeneration.
- Anti-Inflammatory Effects: Stem cells possess inherent anti-inflammatory properties, releasing molecules that can dampen down the inflammatory response in the liver. These molecules, known as cytokines and growth factors, can suppress the activity of inflammatory cells and promote tissue healing. This is particularly relevant in AH, where excessive inflammation drives much of the liver damage. By reducing inflammation, stem cells can help break the cycle of damage and promote a more favorable environment for liver recovery.
- Reducing Scar Tissue Formation: Alcoholic hepatitis often leads to the formation of scar tissue (fibrosis) in the liver. This fibrosis disrupts the standard liver structure and function, eventually leading to cirrhosis. Stem cell therapy may help limit or reverse this fibrosis, preserving the liver’s structural integrity and function. Studies have shown that stem cells can release factors that inhibit the activation of hepatic stellate cells, the primary cells responsible for collagen production and scar tissue formation in the liver.
Types of Stem Cells Used
The Regeneration Center offers several types of stem cells for treating alcoholic hepatitis, each with its unique characteristics and potential advantages: For example, mesenchymal stem cells for alcoholic liver disease show promising regenerative capabilities.
- Mesenchymal Stem Cells (MSCs): MSCs are multipotent stromal cells readily isolated from various adult tissues, including umbilical cord tissue (UC-MSC),whartons jelly stem cells, bone marrow (BM-MSC) and adipose tissue (AT-MSC). They are known for their ability to differentiate into various cell types, including liver cells, making them an attractive candidate for cell-based therapies for liver disease. MSCs also possess immunomodulatory properties, meaning they can modulate the immune response, which is beneficial in the context of AH, where inflammation plays a significant role.
- Hematopoietic Stem Cells (HSCs): HSCs are the stem cells found in bone marrow that give rise to all blood cell types. While not directly differentiating into liver cells, Hematopoietic stem cells have demonstrated a remarkable ability to home to sites of inflammation and release factors that modulate the immune response, potentially reducing liver inflammation in AH. HSCs can also differentiate into endothelial progenitor cells, which contribute to forming new blood vessels, potentially improving blood flow and oxygen delivery to the damaged liver tissue.
- Induced Pluripotent Stem Cells (iPSCs): iPSCs are a type of stem cell that is generated by reprogramming adult cells, such as skin cells or blood cells, to revert to an embryonic-like state. This process endows them with the potential to differentiate into any cell type in the body, including liver cells. iPSCs hold immense promise for regenerative medicine, as they can be used to generate personalized liver cells from the patient’s own cells, minimizing the risk of immune rejection. However, iPSC technology is still relatively new, has additional risks and further research is needed to optimize its safety and efficacy for clinical applications [4].
TREATMENT RISKS & PRECAUTIONS
Treatment for familial conditions using gene therapies are not available. Patients with severe thrombocytopenia, coagulopathy limiting travel will not qualify for the 2 week treatment protocol. Please contact us for.Exploring Different Lineages & Delivery Methods
The success of stem cell therapy hinges not only on the type of stem cells used but also the quantities and method by which they are delivered to the liver. We have explored various delivery methods, each with its advantages and disadvantages. Isolated and expanded stem cells can be delivered to the liver through intravenous (IV) intrahepatic, intrasplenic,intraperitoneal or portal vein injections (PVI)
- Portal vein injections: PVI of stem cells is one method of delivery used in some cases of ARLD, where stem cells are administered directly into the portal vein which is the major blood vessel that supplies the liver with blood from the intestines. This method targets the liver directly, allowing for efficient delivery of stem cells to the site of injury or disease. The stem cells administered can be of various types, such as mesenchymal stem cells or hematopoietic stem cells, depending on the specific condition being treated. Once injected, these cells can potentially differentiate into liver cells or support liver regeneration and repair through the secretion of growth factors and anti-inflammatory agents. This technique is particularly explored for its potential in treating conditions like cirrhosis, liver fibrosis, and other chronic liver diseases, aiming to reduce inflammation, inhibit fibrosis, and enhance functional liver regeneration
- Intravenous Infusion: Intravenous infusion is a simpler and less invasive delivery method. Stem cells are infused into the bloodstream, where they circulate throughout the body and reach the liver through the hepatic portal vein. While less targeted than direct injection, intravenous infusion offers the advantage of potentially reaching multiple areas of liver damage. However, this approach can lead to a lower concentration of stem cells reaching the liver, and some cells may be trapped before reaching their target, reducing their therapeutic efficacy.
- Transplantation of Expanded Stem Cell-Derived Liver Cells: This method involves differentiating stem cells into functional liver cells (hepatocytes) in our laboratory before transplanting them into the patient. This approach offers the advantage of transplanting mature liver cells that can immediately begin contributing to liver function. However due to the complex cell culture techniques needed to generate sufficient numbers of functional liver cells this option takes the longest time to complete.
Assessing the Potential Benefits and Risks
While stem cell therapy for alcoholic hepatitis holds immense promise, it is crucial to approach this emerging field with a balanced perspective, carefully weighing the potential benefits against the possible risks:
Potential Benefits
- Liver Regeneration and Repair: mesenchymal stem cells alleviate liver injury and offer a potential avenue for regenerating damaged liver tissue and improving liver function, reversing some of the damage caused by AH. This regeneration can lead to improved liver function tests, reduced symptoms, reduce the risk of developing liver cancer and potentially prevent the progression of cirrhosis and acute liver failure.
- Reduced Inflammation: The anti-inflammatory effects of stem cells can help mitigate liver inflammation, a hallmark of AH, preventing further liver damage and potentially promoting healing. By dampening the inflammatory cascade, stem cells can create a more favorable microenvironment for liver regeneration and repair.
- Potential for Long-Term Remission: Stem cell therapy holds the potential for long-lasting or even permanent remission of alcoholic hepatitis, freeing individuals from the burden of chronic liver disease. Unlike traditional treatments that primarily focus on symptom management, stem cell therapy aims to address the root cause of the disease by repairing and regenerating damaged liver tissue, potentially providing a long-term solution[5].
Potential Risks
- Immune Rejection: One of the primary concerns with cord blood based cell-based therapy is the risk of immune rejection. The body’s immune system may recognize the transplanted stem cells as foreign and mount an attack against them, leading to transplant rejection. This rejection can lead to inflammation, tissue damage, and graft failure which is why HLA matching is required. To avoid this risk we select cord tissue derived stem cell that do not require HLA matching.
- Tumor Formation: While rare, there is a theoretical risk that some pluripotent stem cells such as iPSC or embryonic stem cells, have the inherent ability to proliferate uncontrollably which could contribute to tumor growth. This risk is higher with totipotent stem cells, such as iPSCs, which have unlimited self-renewal capacity. Rigorous safety studies are essential to minimize this risk and ensure the long-term safety of stem cell therapy for AH. The Regeneration Center does not offer iPSC or embryonic stem cells.
- Long-Term Effects: The long-term effects of stem cell therapy are still being studied, and more research is needed to fully understand the potential risks and benefits, particularly with regard to long-term cell survival, function, and integration within the liver. Long-term follow-up studies are crucial to assess the durability of treatment effects, monitor for any delayed adverse events, and ensure the safety and efficacy of stem cell therapy for AH in the long run.
Looking Ahead: Future Directions
Ongoing research and clinical trials are the lifeblood of progress in stem cell therapy. We are actively working to answer critical questions and translate these promising findings into effective clinical treatments for alcoholic hepatitis. Future research will likely focus on:
- Optimizing Stem Cell Sources and Delivery Methods: Identifying the most effective types of stem cells for treating AH and the most efficient and safe ways to deliver them to the liver will be crucial for maximizing therapeutic benefits. The Regeneration Center has explored various stem cell sources, including bone marrow, adipose tissue, umbilical cord blood, and iPSCs, to determine the optimal cell type for treating AH. Delivery methods are also being refined to improve cell targeting, engraftment, and survival within the liver parenchyma
- Enhancing Stem Cell Engraftment and Survival Rates: Improving the integration and survival of transplanted stem cells within the liver microenvironment is essential for long-term therapeutic success. The Regeneration Center uses various strategies to enhance cell engraftment and survival, such as using biomaterials to create scaffolds that support cell growth or using liver specific cytokines, endothelial cells, growth factors such as hepatocyte growth factor (HGF) and fibroblasts to improve their homing abilities and resistance to cell death. These strategies aim to create a more hospitable environment for transplanted stem cells and endothelial cells to thrive and exert their therapeutic effects.
- Conducting Larger-Scale Clinical Trials: Rigorous clinical trials are the cornerstone of evidence-based medicine. Large-scale clinical trials are essential to evaluate the safety and efficacy of stem cell therapy in a larger, more diverse patient population. These trials will provide invaluable data on the long-term effects of stem cell therapy, optimal dosing regimens, and potential biomarkers of treatment response. They will also help determine its place in the treatment algorithm for alcoholic hepatitis, guiding treatment decisions and improving patient outcomes.
2024 Guidelines & Treatment options for Alcoholic liver disease
Alcoholic hepatitis is a severe liver condition, but recent advances in medical research and UC-MSC stem cell therapy, offer patients a viable alternative to traditional treatments and liver transplants. Stem cell therapy holds significant promise for regenerating damaged liver tissue and improving long-term outcomes for individuals with this challenging disease. As research progresses and our understanding deepens, stem cell therapy may emerge as a transformative treatment option, offering new hope for individuals battling alcoholic hepatitis and potentially revolutionizing the way we approach liver disease treatment. The potential to not only manage symptoms but to actually reverse liver damage and restore function makes stem cell therapy an incredibly promising avenue for the future of AH treatment.
Due to the varying degrees of existing liver damage and the current stage, all potential patients must provide recent medical documents and recent liver radiology scans for review. Isolated and enhanced liver stem cell therapy can be administered multiple ways to begin reduction of severe systemic and liver inflammation thereby, restoring the liver health.
The Regeneration Center treatment for Alcoholic Hepatitis & Alcoholic liver disease with stem cells is an outpatient procedure that will require 12-14 days in Bangkok. After evaluation a detailed medical plan will be provided and will include specifics regarding the medical treatment, exact length of stay needed along with the total costs for our treatment. To learn more, please contact us today.
Published Clinical Citations
[1] ^Wakabayashi M, McKetin R, Banwell C, Yiengprugsawan V, Kelly M, Seubsman SA, Iso H, Sleigh A; Thai Cohort Study Team. Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health. 2015 Dec 24;15:1297. doi: 10.1186/s12889-015-2662-9. PMID: 26704520; PMCID: PMC4690366.
[2] ^ Chuncharunee L, Yamashiki N, Thakkinstian A, Sobhonslidsuk A. Alcohol relapse and its predictors after liver transplantation for alcoholic liver disease: a systematic review and meta-analysis. BMC Gastroenterol. 2019 Aug 22;19(1):150. doi: 10.1186/s12876-019-1050-9. PMID: 31438857; PMCID: PMC6704694.
[3] ^ Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011 Nov;141(5):1572-85. doi: 10.1053/j.gastro.2011.09.002. Epub 2011 Sep 12. PMID: 21920463; PMCID: PMC3214974
[4] ^ Zhou J, Sun C, Yang L, Wang J, Jn-Simon N, Zhou C, Bryant A, Cao Q, Li C, Petersen B, Pi L. Liver regeneration and ethanol detoxification: A new link in YAP regulation of ALDH1A1 during alcohol-related hepatocyte damage. FASEB J. 2022 Apr;36(4):e22224. doi: 10.1096/fj.202101686R. PMID: 35218575; PMCID: PMC9126254.
[5] ^ Chen L, Zhang N, Huang Y, Zhang Q, Fang Y, Fu J, Yuan Y, Chen L, Chen X, Xu Z, Li Y, Izawa H, Xiang C. Multiple Dimensions of using Mesenchymal Stem Cells for Treating Liver Diseases: From Bench to Beside. Stem Cell Rev Rep. 2023 Oct;19(7):2192-2224. doi: 10.1007/s12015-023-10583-5. Epub 2023 Jul 27. PMID: 37498509.