Stem cell treatment for Type 1 diabetes offers an innovative approach by focusing on root autoimmune causes behind the disease. Our unique therapy looks to replace the insulin-producing beta cells and counteract the destruction of insulin-producing beta cells, a hallmark of Type 1 diabetes. By restoring the body’s ability to produce insulin naturally, isolated stem cell therapy represents a significant shift from traditional treatment methods, which primarily revolve around insulin replacement and lifestyle management.[1]
The success of stem cell interventions hinges on overcoming immunological challenges and ensuring the longevity of transplanted cells. The Regeneration Centers’ innovative stem cell-based therapy for Type 1 diabetes can help regulate blood glucose levels and reduce dependence on daily insulin injections. Our unique treatment protocols and post-treatment care continue to build on top of simple diabetes management by including advances in cell culturing and transplantation.
Understanding Type 1 Diabetes
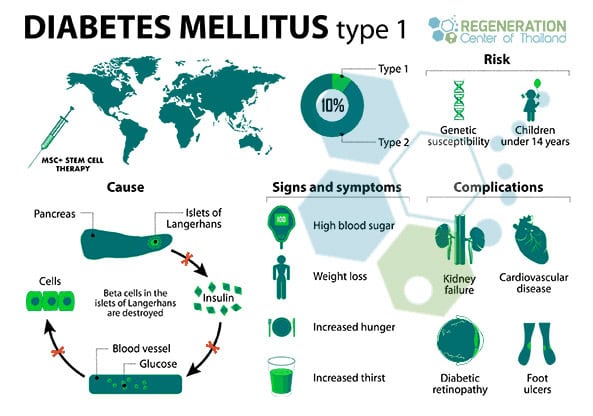
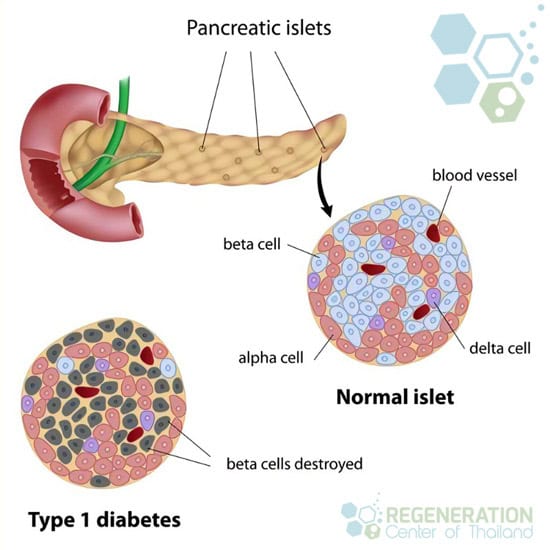 Type 1 diabetes, often diagnosed in childhood, is a chronic condition in which the pancreas produces little to no insulin. This deficiency in insulin production is pivotal in regulating blood glucose levels, necessitating a more profound understanding for those dedicated to serving and supporting affected individuals. At its core, Type 1 diabetes stems from a complex interplay between genetic susceptibility and environmental triggers, which initiates an autoimmune reaction against the insulin-producing beta cells in the pancreas.
Type 1 diabetes, often diagnosed in childhood, is a chronic condition in which the pancreas produces little to no insulin. This deficiency in insulin production is pivotal in regulating blood glucose levels, necessitating a more profound understanding for those dedicated to serving and supporting affected individuals. At its core, Type 1 diabetes stems from a complex interplay between genetic susceptibility and environmental triggers, which initiates an autoimmune reaction against the insulin-producing beta cells in the pancreas.
Genetic susceptibility means specific genes predispose individuals to a higher risk of developing Type 1 diabetes. However, not everyone with these genetic markers will develop the condition, indicating that environmental triggers also play a crucial role. While not fully understood, these triggers are believed to include viruses and other factors that can initiate the autoimmune destruction of beta cells. Type 1 diabetes involves multiple genes that can contribute to the development of the disease. Some of the key gene include: HLA-DQA1, HLA-DQB1, HLA-DRB1, INS, PTPN22, CTLA4, IL2RA, IFIH1
This autoimmune reaction is central to the development of Type 1 diabetes. The body’s immune system mistakenly identifies the beta cells as foreign invaders. It destroys them, a process known as beta cell destruction, a primary target for stem cell-derived therapies. This state significantly decreases the body’s ability to produce insulin. With type 1 diabetes, beta cells produce very little or no insulin. Without insulin production, glucose builds up in the bloodstream instead of going into the cells. This buildup of glucose in the blood is called hyperglycemia.
Understanding these intricate mechanisms is vital for those dedicated to caring for individuals with Type 1 diabetes. By grasping the nuances of genetic susceptibility, environmental triggers, autoimmune reactions, and beta cell destruction, The Regeneration Center can offer its patients more targeted therapy and aftercare support to improve long-term success.[2]
What Causes Type 1 Diabetes?
It is crucial to investigate the specific causes of type 1 diabetes to enhance our understanding of this autoimmune condition. At its core, Type 1 diabetes arises from a complex interplay between genetic predisposition and various environmental triggers that culminate in the immune system mistakenly attacking the body’s cells.
Genetic predisposition plays a pivotal role, setting the stage for the condition. Individuals with specific gene variants are at an increased risk, indicating a heritable component to the disease. However, genetics alone does not account for the onset of Type 1 diabetes; environmental triggers are also essential. These triggers can include, but are not limited to, viral infections, dietary factors, and exposure to certain chemicals and environmental toxins. Viral infections, in particular, have been closely studied for their potential to initiate the autoimmune response that leads to Type 1 diabetes. Pathogens such as enteroviruses are under investigation for their role in triggering the disease in genetically susceptible individuals, providing insights for stem cell therapy for type 1 diabetes.
The crux of Type 1 diabetes lies in the immune system’s attack against the pancreas’s insulin-producing beta cells. This autoimmune response destroys beta cells, severely impairing the body’s ability to produce insulin. The exact mechanisms by which the immune system targets these cells remain a subject of extensive research. Still, the interplay between genetic predisposition and environmental triggers is a driving force behind this process. Other common autoimmune diseases we treat include Sjogren’s syndrome, Hashimoto’s, Lyme disease, mixed connective tissue disorder, SLE Lupus, fibromyalgia, rheumatoid arthritis, and myasthenia gravis.
Symptoms and Risk Factors
Identifying the symptoms and understanding the risk factors associated with Type 1 diabetes are essential steps in managing this chronic condition effectively. Awareness of early signs, such as frequent urination, excessive thirst, unexplained weight loss, and increased hunger, can prompt early detection and timely intervention. Additionally, recognizing the risk factors that contribute to the development of Type 1 diabetes is essential in adopting preventive measures to mitigate its onset.
Genetic predisposition plays a significant role in the likelihood of developing Type 1 diabetes, indicating that individuals with a family history of this condition are at an increased risk for other metabolic diseases, pancreatitis, ARLD, kidney disease, diabetic nephropathy, ulcerative colitis, pancreatic cancer, and liver cirrhosis. This underscores the importance of genetic screening and awareness for those with a familial predisposition to understand their risk profile better and take proactive steps toward monitoring and prevention. Understanding this connection can guide efforts in reducing exposure to potential environmental triggers, possibly delaying or preventing the onset of the disease.
While the lifestyle impact is more closely associated with Type 2 diabetes, it cannot be entirely dismissed in the context of Type 1 diabetes management. Maintaining a healthy lifestyle can support overall well-being and potentially reduce the severity of complications associated with Type 1 diabetes, such as diabetic neuropathy. At-risk patients should perform cardiovascular risk assessment for heart disease, CHF, and heart attack screenings to address modifiable risk factors.
Testing & Diagnosis of Type 1 Diabetes Mellitus
Early detection of Type 1 diabetes is vital. It involves a series of tests to accurately diagnose the condition and evaluate the potential for mesenchymal stem cell therapy. These diagnostic procedures are essential for implementing timely interventions and managing the disease effectively. Health professionals play a pivotal role in this process, guiding patients through the necessary 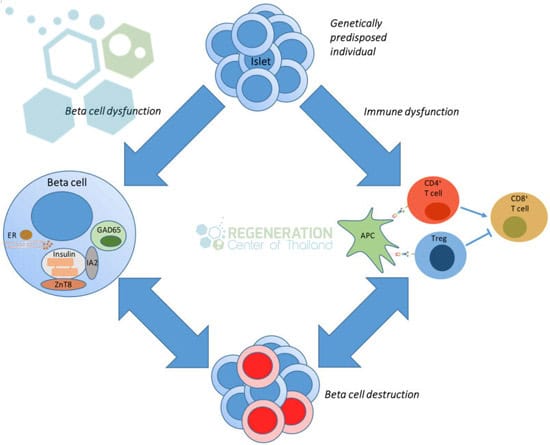 steps to guarantee a thorough understanding and management plan for Type 1 diabetes.
steps to guarantee a thorough understanding and management plan for Type 1 diabetes.
Blood tests are fundamental in the diagnostic arsenal for Type 1 diabetes. They provide invaluable insights into the patient’s blood glucose levels, which indicate the body’s ability to manage sugar. For individuals showing symptoms of diabetes, these tests are often the first step in confirming the disease and determining the need for cell therapy. Autoantibody identification is another critical component of the diagnostic process. These tests search for specific antibodies that are typically present in individuals with Type 1 diabetes, offering a clear marker of the disease’s autoimmune nature. This helps differentiate Type 1 from Type 2 diabetes, ensuring the patient receives the most appropriate care.
Glucose monitoring through fasting blood sugar tests and the oral glucose tolerance test offers further evidence of the body’s glucose management capabilities. These tests help to establish the severity of the diabetes and guide the treatment planning process. Additionally, measuring insulin levels and conducting a C peptide test is essential to understanding the body’s insulin production and the potential for mesenchymal stem cell therapy. Low levels of insulin and C peptide indicate that the pancreas is not producing enough insulin, a hallmark of islet transplantation for Type 1 diabetes. Together, these tests provide a thorough view of the patient’s condition, facilitating a tailored approach to management and care.
Hypoglycemia and Diabetic Ketoacidosis
After confirming the diagnosis of Type 1 diabetes, it is essential to address two significant complications that can arise in type 1 patients: hypoglycemia and diabetic ketoacidosis. These conditions pose immediate health risks and profoundly impact the lifestyle of those affected, underscoring the importance of effective management and preventive strategies.[3]
- Hypoglycemia, characterized by dangerously low blood sugar levels, can lead to symptoms ranging from confusion and dizziness to seizures or loss of consciousness, requiring prompt emergency treatment.
- Diabetic ketoacidosis (DKA) is a severe metabolic complication arising from a deficiency of insulin, leading to high blood sugar levels and a buildup of acids called ketones in the body. It, too, demands urgent medical intervention to prevent life-threatening consequences.
Effective management of these complications involves regular glucose monitoring and meticulous insulin adjustments to maintain blood sugar levels within a target range. This critical approach helps in averting emergencies and significantly mitigates the lifestyle impact of Type 1 diabetes, allowing patients to lead more stable and predictable lives.
Moreover, education on preventive strategies plays an essential role. Patients and their caregivers must be well-informed about recognizing early warning signs of hypoglycemia and DKA, understanding how to adjust insulin dosages appropriately, and when to seek medical help. Emphasizing the importance of dietary management, exercise, and regular health check-ups can further enable individuals to take control of their condition, reduce the risk of complications, and improve their overall quality of life.
Traditional Management Options for Type 1 Diabetic
Traditional management options for Type 1 diabetes primarily revolve around insulin therapy and lifestyle modifications to maintain blood glucose levels within a target range. This approach requires a thorough and personalized plan, emphasizing the importance of dietary adjustments, regular exercise, and a supportive environment for those affected by Type 1 diabetes. Nutritional adjustments are central to managing Type 1 diabetes effectively. A diet rich in nutrients, low in processed sugars, and balanced in carbohydrates can significantly influence blood glucose stability and improve outcomes for people with type 1 diabetes. Endocrinologists often recommend that individuals with diabetes work closely with a dietitian to develop a meal plan that supports their overall health goals while accommodating their unique dietary needs.
The impact of exercise on blood glucose levels is also remarkable. Regular physical activity can improve insulin sensitivity, helping the body to use insulin more efficiently. However, individuals with Type 1 diabetes need to monitor their blood glucose levels closely before, during, and after exercise to prevent hypoglycemia.
Beyond insulin therapy, medication types include alternatives that may be prescribed to address specific aspects of diabetes management, including stem cell therapies. These alternatives, such as GLP-1 receptor agonists, can complement insulin therapy but are unsuitable for everyone. Healthcare providers need to tailor medication plans to the individual’s needs, considering factors like their daily routine, potential side effects, and the effectiveness of the medication in controlling blood glucose levels. Lifestyle changes, encompassing dietary adjustments, increased physical activity, and medication adherence, form the cornerstone of traditional diabetes management. These interventions require ongoing commitment and adaptation to meet changing health needs.
Stem Cell Treatment for Type 1 Diabetes
While traditional management options for Type 1 diabetes focus on insulin therapy and lifestyle changes, stem cell treatment presents a groundbreaking approach aimed at addressing the underlying root causes of the disease. Our innovative treatment promises to manage symptoms and potentially provide a long-lasting solution by encouraging the body’s ability to produce insulin naturally.
The primary goal of Stem cell treatment for Type 1 Diabetes is to restore the body’s ability to produce insulin naturally. This multi-layer approach primarily revolves around multipotent stem cells, which are safer to use than pluripotent stem cells and can differentiate into multiple lineages, including insulin-producing beta cells found in the pancreas. Regeneration Center’s cells are self-renewing and offer anti-inflammatory and immunomodulatory properties. The stem cells needed are isolated and expanded in a controlled lab environment to develop into beta cells.[4]
Once we have cultured the cells to the needed lineages and quantities, they are transplanted back into the patient along with tissue-specific growth factors. The goal is for these newly transplanted beta cells to reside in the pancreas, begin functioning as normal pancreatic cells, and thereby regulate blood glucose levels by producing insulin in response to blood sugar levels. This method is unique as it can reduce or eliminate the need for insulin injections, offering a more sustainable and less invasive solution than lifelong dependency on exogenous insulin. However, challenges in ensuring the long-term viability and safety of the transplanted cells remain significant hurdles to widespread clinical applications. Immunological challenges also remain a substantial hurdle in providing consistent results. Since Type 1 diabetes is an autoimmune condition, any stem cell-based intervention must address the immune system’s role in the disease. The Regeneration Center has developed strategies to prevent the immune system from attacking newly formed insulin-producing cells, an essential step needed for the long-term success of stem cell treatments.
Success Rate after Stem Cells for Type 1 Diabetes
Stem cell treatment for type 1 diabetes and islet cell replacement therapy is not appropriate or effective in all cases. Assessing the effectiveness rate for patients requires a detailed understanding of the patient’s health history and current medical condition. This evaluation must consider several critical factors, including cell procurement, treatment longevity, and follow-up care. 6-12 months after treatment, most participants showed improvement in markers of insulin production and could maintain those levels consistently. Our participants reported spending more time in an optimal blood glucose range and were able to reduce their intake of externally administered insulin.
Cell procurement, isolation, and expansion also play a vital role in the long-term success of stem cell therapy for type 1. The origin and type of stem cells utilized can significantly impact patient outcomes, with autologous and allogeneic (donor-derived) cells that differentiate into insulin-producing cells. Treatment longevity is another vital aspect, as it determines the duration of the therapy’s effectiveness, particularly for cell transplantation therapies. Stem cell treatment represents a promising new tool to treat Type 1 diabetes, offering the potential for significant improvements in patient outcomes. While traditional methods focus on symptom management and insulin supplementation, stem cell therapy addresses the underlying autoimmune causes, potentially restoring pancreatic function.[5]
TREATMENT RISKS & PRECAUTIONS
Please note patients with multiple comorbidities, severe kidney complications or immune system dysregulation may have travel restrictions in travel to Thailand. All potential candidates seeking stem cells for diabetes must be approved in advance using current medical records and recent blood panels that include HbA1C, fasting plasma glucose (FPG), oral glucose tolerance test (OGTT), blood pressure, and lipid profiles.Treat Diabetes with Functioning Beta Cell Transplants
Cell lineages and quantities will depend on the patient’s medical needs. People with diabetes are most often treated by isolated and expanded UC-MSC+ Cells and ductal epithelial cells, β-cells & pancreatic islet-like cells. Older patients or severe cases with multiple underlying conditions will require enhanced allogeneic stem cells (Cord tissue derived w/ anti-HLA antibodies) that are differentiated into glucose-sensing, insulin-producing beta cells.[5]
Stem Cells for Type 1 Diabetes
Treatment Guidelines for Type 1 – 2024
The total number of stem cell infusions will depend on patient needs but will include Umbilical cord mesenchymal stem cells (UC-MSC+), pancreatic progenitor cells, pancreatic islet cells, and β-cells of the pancreas (insulin-producing beta cells). The pancreatic islet cells are cultured from UC-MSC stem cells and essentially look to regenerate the blood sugar-regulating functions of a healthy pancreas.
Types of Cells and Delivery Methods: A combination of expanded mesenchymal stem cells and pancreatic endocrine cells (differentiated into beta cells) are delivered along with pancreatic progenitor cells to the patient via IV, Intrapancreatic Injections, Intraperitoneal Injections, or Intra-Arterial Injections, depending on patient needs.
Rehabilitation Treatment : (Optional) Rehabilitation therapy (2 hours per day and five days per week) , medical visas, and accommodations for an extended stay can also be included at an additional cost.
Treating T1DM With Stem Cells
The cellular treatment for type 1 will require a minimum of 10-14 days in Bangkok. The costs for treating Diabetes with MSC+ cells will depend on many factors, including current health and other underlying medical conditions. To provide treatment recommendations, our medical team will need to review patients’ recent medical information and current biochemistry test results. Upon completion of therapy evaliuation, a customized treatment plan will be provided that includes all medical related costs including stem cell extractions, expansion and delivery, To learn more about the stem cells for type 1 diabetes using Adult stem cells please contact us today.
Published Clinical Citations
[1] ^Dejkhamron P, Santiprabhob J, Likitmaskul S, Deerochanawong C, Rawdaree P, Tharavanij T, Reutrakul S, Kongkanka C, Suprasongsin C, Numbenjapon N, Sahakitrungruang T, Lertwattanarak R, Engkakul P, Sriwijitkamol A, Korwutthikulrangsri M, Leelawattana R, Phimphilai M, Potisat S, Khananuraksa P, Nopmaneejumruslers C, Nitiyanant W; Thai Type 1 Diabetes and Diabetes Diagnosed Before Age 30 Years Registry, Care, and Network (T1DDAR CN). Type 1 diabetes management and outcomes: A multicenter study in Thailand. J Diabetes Investig. 2021 Apr;12(4):516-526. doi: 10.1111/jdi.13390. Epub 2020 Oct 4. Erratum in: J Diabetes Investig. 2022 Apr;13(4):749. doi: 10.1111/jdi.13794. PMID: 32815278; PMCID: PMC8015826.
[2] ^Banchuin N, Boonyasrisawat W, Vannasaeng S, Dharakul T, Yenchitsomanus PT, Deerochanawong C, Ploybutr S, Sriussadaporn S, Pasurakul T. Cell-mediated immune responses to GAD and beta-casein in type 1 diabetes mellitus in Thailand. Diabetes Res Clin Pract. 2002 Mar;55(3):237-45. doi: 10.1016/s0168-8227(01)00322-9. PMID: 11850100.
[3] ^ Dejkhamron P, Santiprabhob J, Likitmaskul S, Deerochanawong C, Rawdaree P, Tharavanij T, Reutrakul S, Kongkanka C, Suprasongsin C, Numbenjapon N, Sahakitrungruang T, Lertwattanarak R, Engkakul P, Sriwijitkamol A, Korwutthikulrangsri M, Leelawattana R, Phimphilai M, Potisat S, Khananuraksa P, Kunsuikmengrai K, Nitiyanant W; Thai Type 1 Diabetes and Diabetes diagnosed Age before 30 years Registry, Care and Network (T1DDAR CN). Young-onset diabetes patients in Thailand: Data from Thai Type 1 Diabetes and Diabetes diagnosed Age before 30 years Registry, Care and Network (T1DDAR CN). J Diabetes Investig. 2022 May;13(5):796-809. doi: 10.1111/jdi.13732. Epub 2022 Jan 6. PMID: 34890117; PMCID: PMC9077742.
[4] ^Hogrebe NJ, Ishahak M, Millman JR. Developments in stem cell-derived islet replacement therapy for treating type 1 diabetes. Cell Stem Cell. 2023 May 4;30(5):530-548. doi: 10.1016/j.stem.2023.04.002. PMID: 37146579; PMCID: PMC10167558.
[5] ^Millman JR, Xie C, Van Dervort A, Gürtler M, Pagliuca FW, Melton DA. Generation of stem cell-derived β-cells from patients with type 1 diabetes. Nat Commun. 2016 May 10;7:11463. doi: 10.1038/ncomms11463. Erratum in: Nat Commun. 2016 Aug 04;7:12379. doi: 10.1038/ncomms12379. PMID: 27163171; PMCID: PMC4866045.