Primary Sclerosing Cholangitis (PSC) presents a significant therapeutic challenge in hepatology, with conventional treatments offering limited success in disease management. The emergence of isolated and expanded mesenchymal stem cell therapy represents a novel approach to addressing the underlying pathophysiology of PSC. Results from our previous clinical applications have shown measurable benefits in modulating inflammatory responses and promoting biliary regeneration. However, the complexity of PSC’s autoimmune mechanisms and the varied patient responses to stem cell interventions warrant careful examination of this promising treatment modality.
Understanding Primary Sclerosing Cholangitis
Primary Sclerosing Cholangitis (PSC) is a progressive, chronic cholestatic liver disease characterized by inflammation and fibrosis of both intrahepatic and extrahepatic bile ducts. The causes of PSC remain incompletely understood, though research indicates a complex interplay between genetic factors, immune system dysfunction, and environmental triggers. Patients with PSC may also experience complications involving other digestive organs, such as liver cancer (cholangiocarcinoma) and pancreatitis, highlighting the importance of comprehensive diagnostic assessments.
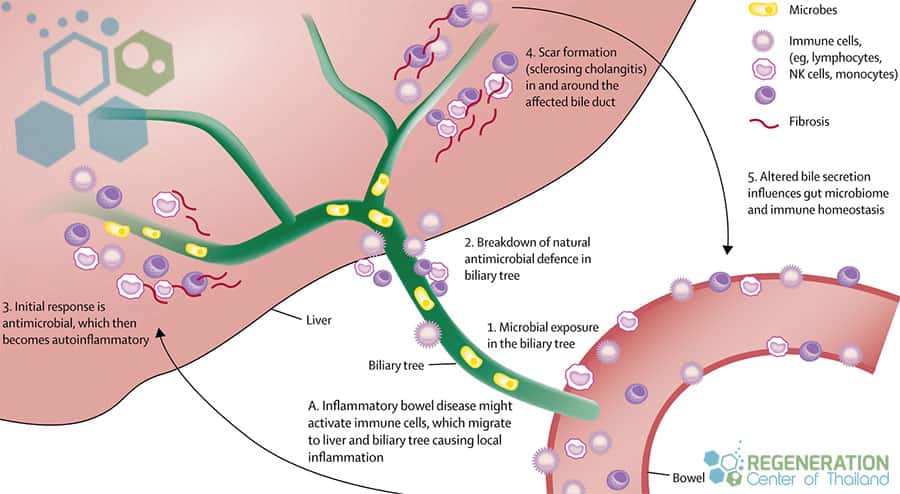
The progression of PSC typically manifests through recurring episodes of cholangitis, leading to bile duct strictures and eventual liver cirrhosis. Genetic factors in PSC play a significant role, with studies identifying multiple risk loci, particularly in the HLA complex region[1]. Approximately 60-80% of PSC patients also present with inflammatory bowel disease, suggesting shared pathogenic mechanisms.
The disease predominantly affects males between 30 and 40 years of age and advances at varying rates. Without intervention, PSC often progresses to end-stage liver disease, necessitating liver transplantation. Early diagnosis and monitoring are pivotal for managing complications and optimizing treatment outcomes in affected individuals.
PSC and Its Strong Link to Ulcerative Colitis
The profound association between Primary Sclerosing Cholangiomyelitis (PSC) and Ulcerative Colitis (UC) represents one of the most potent disease correlations observed in hepatology. Approximately 70-80% of PSC patients exhibit concurrent UC. This autoimmune condition link manifests through shared inflammatory pathways affecting the biliary system and the colon. Research indicates that patients with both conditions often experience more extensive gastrointestinal complications compared to those with isolated UC [2].
The inflammatory bowel disease component typically presents before or simultaneously with PSC diagnosis, though some cases emerge afterward. The concurrent presence of both conditions necessitates detailed monitoring and coordinated targeted treatment approaches. Patients with PSC must remain vigilant in testing for complications in both organ systems, as the disease progression in one condition can influence the other. This relationship also suggests common immunological mechanisms, leading us to investigate how combined targeted therapies could address both conditions simultaneously.
Current Treatment Methods for PSC
Currently available treatment methods for Primary Sclerosing Cholangitis remain limited, with no approved therapies specifically targeting the underlying disease mechanism. Medication management focuses primarily on symptom control and complications prevention, utilizing ursodeoxycholic acid (UDCA) to improve bile flow and reduce inflammation of the bile ducts. Managing PSC often requires addressing metabolic complications, as patients can develop associated conditions like Diabetic Nephropathy, PKD, Diabetes Type 1 or Type 2 diabetes, further complicating their disease progression [3].
When bile duct strictures develop, endoscopic or percutaneous interventions may be necessary to maintain biliary drainage and prevent cholangitis. Dietary modifications, including fat-soluble vitamin supplementation and reduced sodium intake, help manage nutritional deficiencies and fluid retention commonly associated with advanced disease.
For patients nearing end-stage liver disease, stem cell therapy or liver transplantation remains the only curative option. However, PSC can recur in the transplanted liver in approximately 20-25% of cases. The Regeneration Center does not offer liver transplant options as post-transplant management requires careful monitoring and immunosuppression to prevent rejection while managing the risk of recurrent disease.
Difference Between PSC and Primary Biliary Cholangitis (PBC)
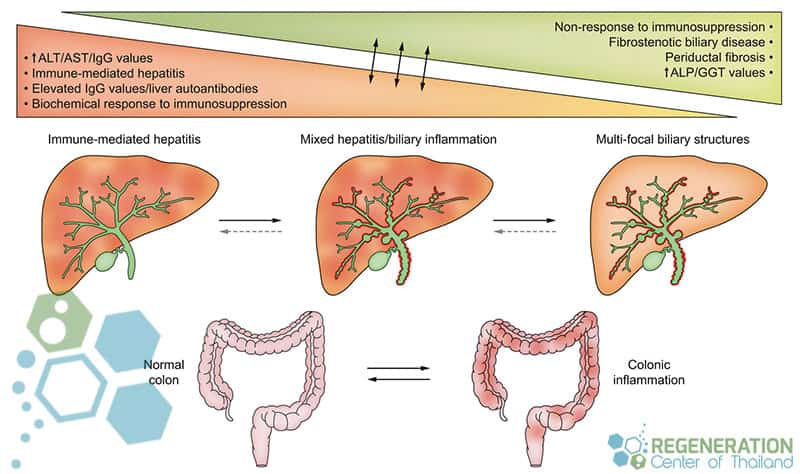
Although both conditions affect the biliary system, Primary Sclerosing Cholangitis (PSC) and Primary Biliary Cholangitis (PBC) exhibit distinct pathological mechanisms, disease progression patterns, and demographic profiles. PSC mainly affects the large bile ducts with a characteristic pattern of multifocal strictures and dilations, while PBC targets small intrahepatic bile ducts. The liver damage comparison reveals that PSC causes periductal fibrosis in a concentric pattern, whereas PBC leads to granulomatous destruction of tiny ducts. Unlike PSC, which has strong autoimmune and genetic factors, other hepatic conditions such as Alcohol-related Liver Disease (ARLD) are directly linked to lifestyle and prolonged excessive alcohol intake.
Despite their similarities in autoimmune diseases such as multiple sclerosis, connective tissue disease, and rheumatoid arthritis, PSC is strongly associated with inflammatory bowel disease, particularly ulcerative colitis, while PBC demonstrates specific anti-mitochondrial antibodies. Demographically, PSC typically affects younger males, with onset around age 30-40, while PBC predominantly occurs in middle-aged women. The bile duct characteristics in imaging studies show that PSC presents a “beaded” appearance in cholangiography, distinguishing it from the normal-appearing large ducts in PBC patients.
Stem Cell Treatment for Primary Sclerosing Cholangitis
Recent advancements in stem cell therapy have emerged as a promising investigational treatment for Primary Sclerosing Cholangitis (PSC), targeting both inflammatory processes and biliary regeneration. The Regeneration Center has focused on various adult stem cell transplantation approaches, including multipotent mesenchymal stem cells and hematopoietic stem cell therapy, to modulate the immune response and promote tissue repair[4].
Stem cell regeneration protocols typically involve either autologous or allogeneic transplantation methods. The therapeutic mechanism relies on stem cell mobilization from bone marrow or adipose tissue and systematic administration to target damaged bile ducts. These cells demonstrate immunomodulatory properties and the ability to differentiate into cholangiocytes, potentially reversing biliary damage and apoptosis.
Clinical trials have shown promising results in reducing inflammation and improving liver function markers. However, ideal, suitable, or favorable timing, dosing, and delivery methods remain under investigation. Combining stem cell therapy with conventional treatments may enhance therapeutic outcomes for PSC patients. However, more long-term controlled studies are needed to establish clinical efficacy and consistent results.
Benefits and Risks of Stem Cell Therapy for PSC
Stem cell therapy for PSC presents a complex balance of therapeutic benefits and potential complications that warrant careful clinical consideration. Clinical studies indicate significant possible benefits, including improved quality of life through reduced bile duct inflammation and enhanced liver function. The therapy may decrease fibrosis progression and potentially reduce the need for liver transplants in selected patients.
However, essential risks must be evaluated, including immune reactions, potential tumor formation, and procedure-related complications. Administration site reactions and temporary elevation of liver enzymes have been reported in some cases. The long-term efficacy and safety profile requires further investigation through controlled clinical trials.
After Treatment of the Liver with Stem Cells
The therapeutic benefits of reduced inflammation and biliary regeneration must be weighed against these risks for each patient individually. Careful patient selection, monitoring, and adherence to established protocols are essential to maximize positive outcomes while minimizing potential complications in PSC stem cell interventions.
TREATMENT RISKS & PRECAUTIONS
Treatment for hereditary PSC using gene therapies is in private trials only and not available at this time. Patients with severe liver fibrosis, PSC complications or travel limitation may not be candidates for the estimated 2-week treatment protocol.Stem cell therapy represents a novel therapeutic frontier for managing Primary Sclerosing Cholangitis, offering potential immunomodulatory and regenerative benefits. While preliminary data suggests promise in reducing biliary inflammation and hepatic fibrosis, rigorous clinical trials are essential to establish long-term safety profiles and standardized protocols. Implementation requires careful patient stratification, exhaustive monitoring, and integration with existing treatment modalities to optimize therapeutic outcomes in PSC patients.
2025 Guidelines for Treating PSC
Due to the varying severity of liver damage, all potential patients must provide recent medical documents, lab results, and radiology scans for review. It aims to offer a less invasive alternative. Isolated and enhanced UC-MSC+ stem cells will be administered with liver-specific growth factors through intravenous (IV), intrasplenic, intrahepatic, intraperitoneal, or portal vein injections (PVI), where the cells can transport through the blood supply into the hepatic system to initiate the regenerative cycle and restore liver health [5].
Cost of Stem Cells for Primary Sclerosing Cholangitis
The Regeneration Center treatment protocol for hepatic fibrosis, Primary Sclerosing Cholangitis & liver disease will depend entirely on patient needs. The multi-stage treatment we offer is performed as an outpatient procedure and will require 10-12 days in Bangkok. We must review copies of recent lab results and radiology scans to evaluate a patient for potential treatment. After completion of treatment evaluation, a detailed plan will be provided that will include the specific medical recommendations for the patient, the total length of stay required, and the total fixed costs for the entire medical portion. To learn more about treating PSC and Bile duct strictures with stem cells, please contact us today.
Published Clinical Citations
[1] ^ Karlsen TH, Schrumpf E, Boberg KM. Genetic epidemiology of primary sclerosing cholangitis. World J Gastroenterol. 2007 Nov 7;13(41):5421-31. doi: 10.3748/wjg.v13.i41.5421. PMID: 17907284; PMCID: PMC4171275.
[2] ^Wijarnpreecha K, Panjawatanan P, Mousa OY, Cheungpasitporn W, Pungpapong S, Ungprasert P. Association between appendectomy and risk of primary sclerosing cholangitis: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Oct;42(5):436-442. doi: 10.1016/j.clinre.2018.03.011. Epub 2018 Apr 11. PMID: 29655526.
[3] ^ Lightner AL, Dadgar N, Vaidya A, Simon R, Fulmer C, Siddiki H, Narayanan Menon KV, Liu P, Matthew Walsh R. Mesenchymal stem cells: A novel treatment option for primary sclerosing cholangitis. Cell Biol Int. 2023 Feb;47(2):467-479. doi: 10.1002/cbin.11943. Epub 2022 Nov 2. PMID: 36321586.
[4] ^ Dorner H, Stolzer I, Mattner J, Kaminski S, Leistl S, Edrich LM, Schwendner R, Hobauer J, Sebald A, Leikam S, Gonzalez Acera M, Düll M, Lang R, Seidel G, Seitz T, Hellerbrand C, Fuhrmann G, Distler U, Tenzer S, Eichhorn P, Vieth M, Schramm C, Arnold P, Becker C, Weidinger C, Siegmund B, Atreya R, Leppkes M, Naschberger E, Sampaziotis F, Dietrich P, Rauh M, Wirtz S, Kremer AE, Neurath MF, Günther C. Gut Pathobiont-Derived Outer Membrane Vesicles Drive Liver Inflammation and Fibrosis in Primary Sclerosing Cholangitis-Associated Inflammatory Bowel Disease. Gastroenterology. 2024 Nov;167(6):1183-1197.e16. doi: 10.1053/j.gastro.2024.06.032. Epub 2024 Jul 9. PMID: 38992449.
[5] ^ Meng F, Alpini G. Peri-scoping the biliary tree reveals stem cell activation in peribiliary glands in primary sclerosing cholangitis. J Hepatol. 2015 Nov;63(5):1062-3. doi: 10.1016/j.jhep.2015.07.015. Epub 2015 Jul 26. PMID: 26212028.