Congestive Heart Failure or “CHF” is a state wherein the heart does not have the capability to properly function as a pump. As a result of the cardiac-malfunction the oxygen pumped into the body is insufficient. Congestive heart failure is generally caused by simultaneous illnesses.
What is CHF?
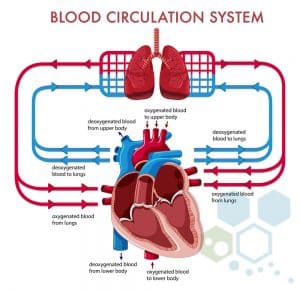 CHF or Chronic heart failure is a progressive condition that affects the power and efficiency of heart muscles. Often referred to as heart failure, this type of cardiovascular disease is diagnosed after fluid buildup around the heart, causing it to function inefficiently. There are two halves and four chambers in the human heart. The upper half of the heart has (2) atrium while the lower half has (2) ventricles that pump blood throughout the bodies tissues and organs. The atria then receive the blood back after a loop to then circulate it right back.
CHF or Chronic heart failure is a progressive condition that affects the power and efficiency of heart muscles. Often referred to as heart failure, this type of cardiovascular disease is diagnosed after fluid buildup around the heart, causing it to function inefficiently. There are two halves and four chambers in the human heart. The upper half of the heart has (2) atrium while the lower half has (2) ventricles that pump blood throughout the bodies tissues and organs. The atria then receive the blood back after a loop to then circulate it right back.
If the ventricles get damaged (diastolic heart failure) or diseased, blood and other fluids can leak from capillary blood vessels to areas including liver, lungs, stomach, and legs creating a life-threatening situation that often requires immediate medical attention. Other symptoms of damage to the heart ventricles include frequent shortness of breath, swelling (edema), and weakness.
Right Sided vs. Left-Sided Heart Failure
The left side of the heart is responsible for pumping blood while the right side pumps blood to the lungs. When blood enters
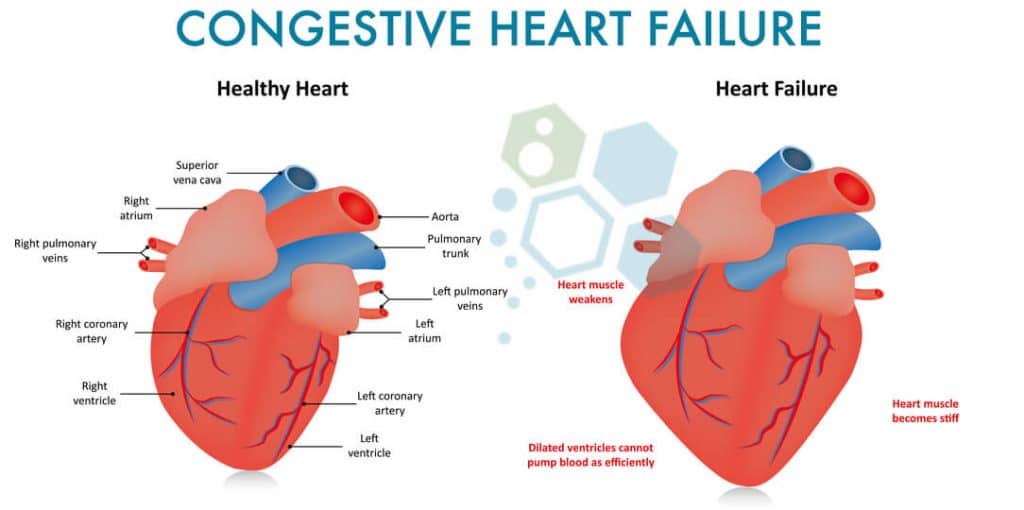
The right atrium (via vena cava) It flows to the right ventricle where it gets pumped into the lungs via the pulmonary artery. The pulmonary artery carries the deoxygenated blood to the lungs where oxygen infuses with red blood cells before returning to the left atrium via the pulmonary veins. From the pulmonary veins, blood flows to the left ventricle of the heart before being pumped back to tissues and organs in the body. The red blood cells carry Oxygen to our organs while the waste product of carbon dioxide is picked up to be removed via the lungs (breath out.) Blood can then return to the right atrium to do the processes again over and over again. The pulmonary veins are used to carry oxygenated blood, while the pulmonary arteries are responsible for taking deoxygenated blood. This relationship between veins and arteries is opposite in the rest of the body.
Heart disease is described as an Illness that weakens the cardiovascular system, heart muscle, or illnesses that trigger the heart muscles to become stiff, or disorders that create an increase in oxygen demands which consequently increases the supply for fresh oxygen when the heart is incapable of producing oxygen-rich blood at the level needed.
Congestive heart failure and ischemic heart disease can have an impact on numerous organs in the body. For instance, the injured areas of the heart directly affected by the sickness cannot produce enough blood for the kidneys, which then affect their ability to excrete water and salt (sodium). The distressed kidney function may cause the person to retain more fluids than needed. Patients with higher cardiometabolic risks or history of muscular atrophy may also develop pulmonary edema (PE).
PE occurs when the fluid in the lungs diminishes a person’s ability to exercise regularly. Fluid might likewise accumulate inside the liver, which directly affects its function by impairing the livers’ capability to create essential proteins and also in helping clear the system of harmful elements or toxins. The intestines might even turn out to be much less effective in being able to absorb the vitamins, nutrients, and medicines a human needs. The fluids can also accumulate quickly, which could result in peripheral neuropathy or edema (severe swelling) of the ankles and feet.
Stages of Congestive Heart Failure
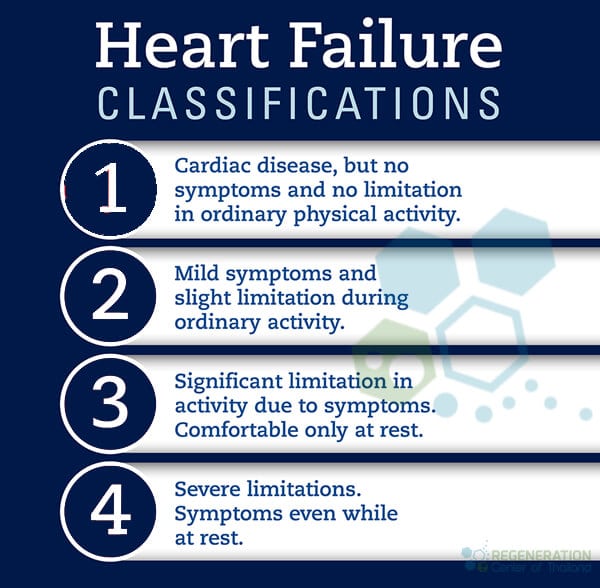
There are four main stages of Systolic heart failure: 1, 2, 3, and 4 or ( A, B, C, D depending on which country)
- Stage 1 is the lowest severity, and often are unaware of any problems. Stage 1 or pre-heart failure patients are considered at high risk of developing heart failure. Examples of these Stage 1 diagnosis include patients with diabetes, History of alcohol abuse, high blood pressure, or coronary artery disease.
- Stage 2 Systolic heart failure is considered pre-heart failure and usually given to patients with an ejection fraction (EF) percentage of 40 or less along with systolic left ventricular dysfunction.
- Stage 3 Heart Failure patients are previously or currently diagnosed with diastolic heart failure due to the underlying structural damage to the heart and cardiac function. Patients diagnosed with stage 3 (C) of heart disease are usually prescribed Beta-blockers, Hydralazine/nitrate combinations, vasodilator medicines (Aldosterone antagonist), heart stem cell repair, diuretics and may need implantable cardiac defibrillator (lCD) or biventricular pacemaker.
- Stage 4 Heart Failure is considered final (end) stage heart failure. Patients with Stage 4 (D) typically had a failed treatment in the earlier stages and required more advanced options including Open Heart surgery, cardiac stem cell treatments, Ventricular assist device, continuous inotropic medications or a heart transplant.
Causes of Diastolic Heart Failure
Cardiomyopathies and damage to the heart can occur due to many reasons, including lifestyles environmental and genetics. Autoimmune diseases such as psoriasis, rheumatoid arthritis and lupus can double the risk of heart failure. Some other common risk factors including
- Diabetes and Diabetic Nephropathy
- Hypertension
- Parkinsons
- Kidney Failure
- Lung disease
- Viral Infections
- Abuse of drugs & alcohol
- Connective tissue disorders such as systemic lupus erythematosus
- Obesity
- Exposure to toxins such as cobalt & lead
- Reaction to prescription medications

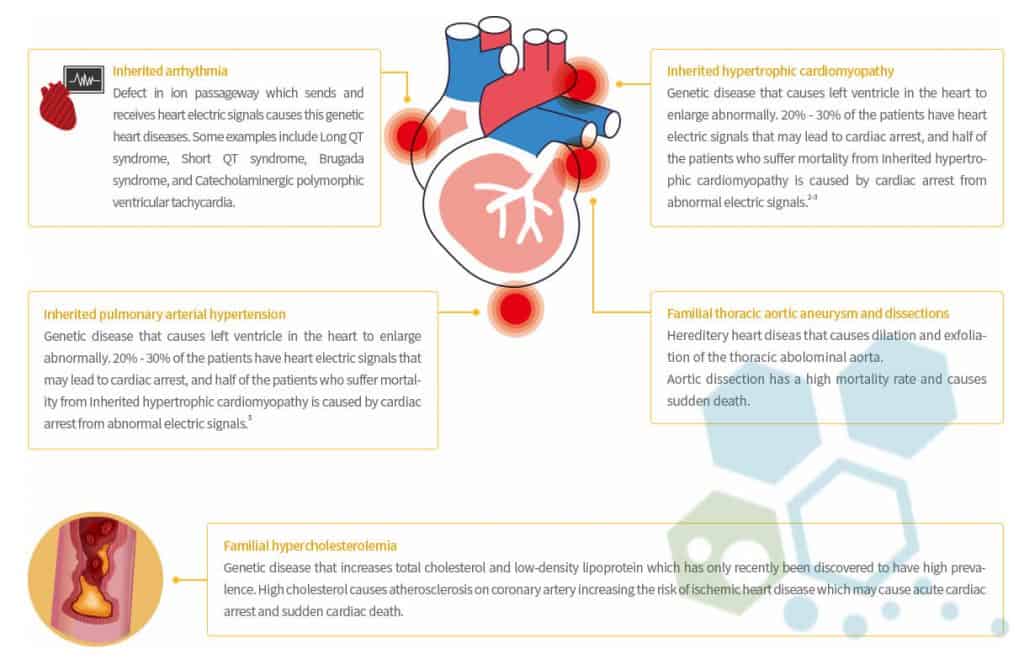
Is CHF Hereditary?
Most cases of heart failure are not hereditary, but some uncommon types of heart disorders can be passed down through generations. Examples of genetic variants include:
- Aortopathy & connective tissue disorders
- Pulmonary arterial hypertension
- Arrhythmia
- Familial Cardiomyopathy (hypertrophic)
- Congenital heart failure
- Hereditary hemorrhagic telangiectasia
- Familial hypercholesterolemia
The regeneration center of Thailand offers a comprehensive list of DNA tests for heritable heart and vascular conditions, including the following panels.
DOLK,TAZ, TCAP, TMEM43, TNNC1, TNNI3, JUP, LAMP2, LMNA, MYBPC3, DSC2, DSG2, DSP, EMD, MYH7, MYL2, MYL3, PKP2, PLN, PRKAG2, RAF1,EYA4,ABCC9, ACTC1, ACTN2,FHL1, FKRP, FKTN, FLNC, GAA, GLA, HCN4, AGL, BAG3,TNNT2, TPM1, TTN, TTR, VCL,RBM20, RYR2, SCN5A, SGCD, SLC22A5, CACNA1C, CAV3, CRYAB, CSRP3, DES, ANKRD1, CTNNA3, LDB3, PDLIM3 and DMD.
There are several randomized clinical trials underway to treat genetic heart defects using gene therapy; however, none are approved for use yet. Studies have proven that to help reduce the risk of developing end-stage heart failure, consider making changes to your diet, and get regular exercise.
Stem Cell Treatment for Heart Failure
An Ejection fraction (EF) of 20% would be considered a dangerous level and therefore indicates a highly advanced stage of heart failure. Healthy people without any cardiovascular diseases usually have ejection fractions in between 52% and 68%.
The primary issue is the fact that the chamber responsible for pumping one’s heart (The left ventricle) becomes enlarged and isn’t beating effectively, causing the EF percentage level to dangerously low levels. Ideally, EF percentages ought to be between 52% and 74%. This number also represents the quantity of blood pumped out from the heart on every beat. The walls of the left ventricle are hypokinetic. Hypokinetic state indicates they are not contracting correctly. This is also why the EF% is low, and the patients have Diastolic Dysfunction of the heart.
Regeneration Center Patient 1 Year After Stem cells for Heart
Endogenous Cell Therapy for CHF
MSC Stem cells are unspecialized cells that have two essential characteristics that distinguish them from other cells inside our bodies. Stem Cells can replenish their numbers naturally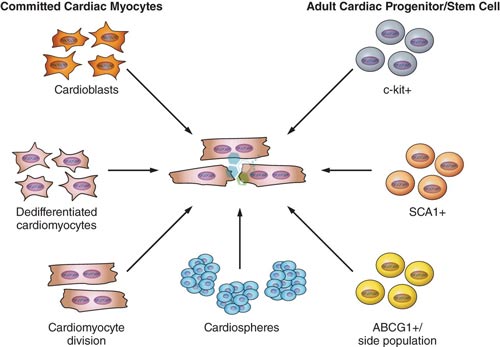 and indefinitely via cell division and the paracrine cell communication mechanism. When circulating stem cells receive chemical indicators of trauma, dysfunctions, or damage of any kind they can migrate directly to the injured/dysfunctional area and transform themselves into the specialized cells needed to perform particular functions. Functions or tissues or cells like nerve cells, circulating progenitor cells, mononuclear cells, mesenchymal stem cells, and hematopoietic progenitor cells. Other cardiology therapies include:
and indefinitely via cell division and the paracrine cell communication mechanism. When circulating stem cells receive chemical indicators of trauma, dysfunctions, or damage of any kind they can migrate directly to the injured/dysfunctional area and transform themselves into the specialized cells needed to perform particular functions. Functions or tissues or cells like nerve cells, circulating progenitor cells, mononuclear cells, mesenchymal stem cells, and hematopoietic progenitor cells. Other cardiology therapies include:
- Coronary artery disease (CAD)
- Angina
- Biventricular failures
- Disorders of the Heart Valves
- Cardiomyopathy
- Ischemia & Chronic ischaemic heart disease (IHD)
- Terminal Heart failure
- Myocardial infarction – Heart Attacks
Heart Regeneration Therapy Guidelines for 2024
Using stem cells for heart & cardiac regeneration therapies using cord tissue cells is are a breakthrough treatment that requires enriched mesenchymal stem cells (MSC+) are introduced into damaged heart tissue. This cellular proliferation helps enhance the performance/condition of patients suffering from congestive severe heart failure or brain strokes. Stem cells for CHF works primarily through the creation of new blood vessels Angiogenesis that also helps improve tissue perfusion. The freshly expanded cardiac cells are carefully “transplanted” back into the patient through targeted infusions or into the damaged heart muscle or even by infusing them into the coronary arteries. Through the process of “Homing” [2] Stem cells migrate into the heart muscles for months after the initial treatment to assist in the regeneration process through the transformation into healthy functioning heart cells and reverse coronary heart failure.
Stem cell treatment for low ejection fraction
- Sustained improvement in heart pumping power and its ability to regulate proper supply blood to the body [3]
- Improved regulation of O2 (Oxygen) Intake and Use [4]
- Increase in myocardial performance, neurohumoral activations, and functional heart capacity
- Greater Reduction in Angina [1]
- Reduction in the infarct size with a reduction in heart muscle scar and reversal of cardiogenic shock
- Long-term follow-up (≥12 months) shows noticeable improvement in the patients overall well-being and physical endurance.
- Improvement of ventricular ejection fraction resulting in a reduced need of rehospitalization [5]
CLINICAL TREATMENT PRECAUTIONS & RISKS
Please note stem cell treatment for CHF and cardiac stem cell therapies may not be appropriate for all conditions. Cell therapy and heart tissue and cell engineering are limited based on the extent of the heart muscle and tissue damage and current and accurate medical condition of the patient. Patients who are considered “high risk”, have severe inflammatory osteoarthritis or requiring sustained oxygen assistance preventing international travel may not qualify. MSC+ Cardiac therapy is appropriate for patients looking to improve ventricular performance, quality of life and overall survival rates for patients with heart failure.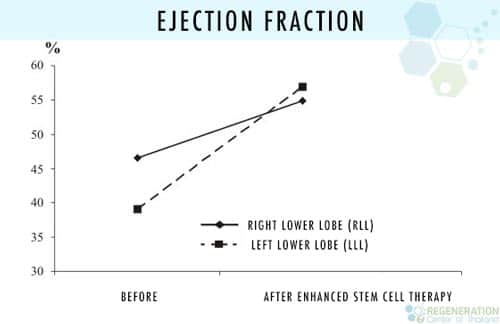
Chronic Heart Failure Treatment Options
Adjuvant therapy using Cardiopoietic MSC+ Stem cells (per treated stage) Severe cases with multiple commodities may require a multiple stage delivery using transvascular injections with direct injection Into the ventricular walls to ensure optimal results. Rehabilitation after treatment is optional based on the patients time constraints. Full rehabilitation and nursing care can be provided 2-4 hours per day and up to 4 days per week
. Medical visas and accommodations for the patient and family/friends at an extended stay hotel can be included upon request. Depending on stage and severity the estimated treatment length is 14 – 21 days in total.
CHF Therapy Requirements & Safety Advice
Our clinical cell therapy for heart failure is focused on providing measurable results which require proper extraction and expansion of MSCs and cardiosphere-derived cells before infusions. The multi-stage cardiac regeneration protocol is a 2-week procedure with the option of cardio-physical rehabilitation in Bangkok, Phuket, or Chiang Mai for 5-15 days after being treated. Due to the varying degrees of heart disease, our medical team will first need to understand the patient’s current medical needs better to determine cell therapy will be beneficial. Upon acceptance, A detailed treatment plan will be provided and will include a day by day itinerary outlining the cardiac cell regeneration protocol along with other details such as an exact total number nights required along with the total and fixed medical related costs. To begin your evaluation for the regeneration center MSC+ heart therapy please prepare evidence or recent medical records such as an Echocardiogram, EKG, Stress test, Tilt Table, Heart CT Scan or SPECT exam (Single-photon emission computed tomography) and contact us today.
Published Clinical Citations
[1] ^ Boonbaichaiyapruck, Sarana, Pavit Pienvichit, Thosapol Limpijarnkij, Pairoj Rerkpattanapipat, Apichai Pongpatananurak, Ratchanee Saelee, Artit Ungkanont, and Suradej Hongeng. 2010. Transcoronary infusion of bone marrow derived multipotent stem cells to preserve left ventricular geometry and function after myocardial infarction. Clinical cardiology Thailand, no. 7. doi:10.1002/clc.20545. https://www.ncbi.nlm.nih.gov/pubmed/20552656
[2] ^ Hou, Jingying, Lingyun Wang, Jieyu Jiang, Changqing Zhou, Tianzhu Guo, Shaoxin Zheng, and Tong Wang. Cardiac stem cells and their roles in myocardial infarction. Stem cell reviews and reports, no. 3. doi:10.1007/s12015-012-9421-4. https://www.ncbi.nlm.nih.gov/pubmed/23238707
[3] ^ Nartprayut, Kuneerat, Yaowalak U-Pratya, Pakpoom Kheolamai, Sirikul Manochantr, Methichit Chayosumrit, Surapol Issaragrisil, and Aungkura Supokawej. Cardiomyocyte differentiation of perinatally‑derived mesenchymal stem cells. Molecular medicine reports, no. 5 (March 4). doi:10.3892/mmr.2013.1356. https://www.ncbi.nlm.nih.gov/pubmed/23467912
[4] ^ Pratumvinit, Busadee, Kanit Reesukumal, Kajohnkiart Janebodin, Nicholas Ieronimakis, and Morayma Reyes. 2013. Isolation, characterization, and transplantation of cardiac endothelial cells in Thailand. BioMed research international (October 27). doi:10.1155/2013/359412. https://www.ncbi.nlm.nih.gov/pubmed/24282814
[5] ^ Sheng, Calvin C, Li Zhou, and Jijun Hao. 2012. Current stem cell delivery methods for myocardial repair. BioMed research international (December 27). doi:10.1155/2013/547902. https://www.ncbi.nlm.nih.gov/pubmed/23509740