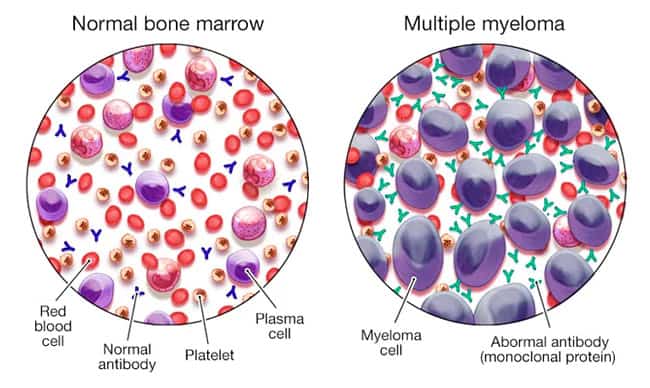
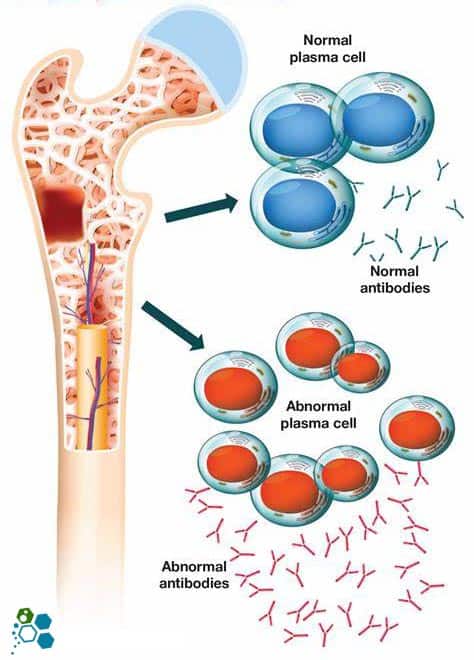
Myeloma & Multiple myeloma (also known as Kahler’s disease) is type of cancer that develops in the bone marrow (plasma cells). Plasma cells are part of our immune system and are considered white blood cells that help make antibodies (also called immunoglobulins) to help the body fight infections. The plasma white blood cells help create antibodies when a patient develops an infection. The body makes different types of antibodies for different kinds of conditions, and these help antibodies find, attack and kill 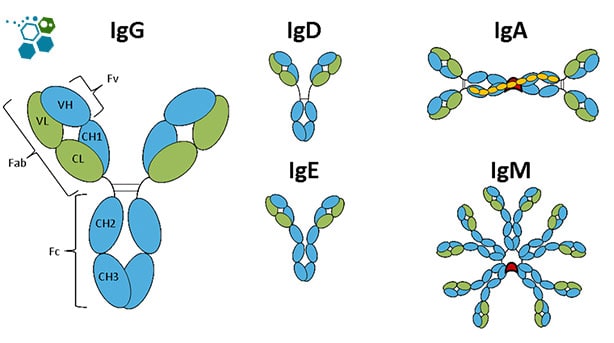 viruses and bacteria, thus protecting us from getting sick
viruses and bacteria, thus protecting us from getting sick
There are five immunoglobulins (antibody) types:
- IgA
- IgG
- IgM
- IgD
- IgE
About Multiple Myeloma
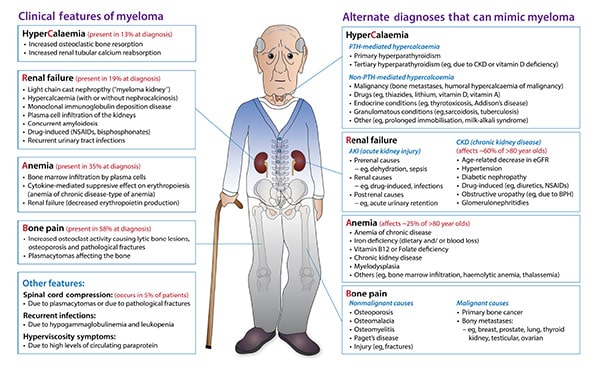
These plasma cells are considered abnormal for patients with multiple myeloma and have grown out of control. Such uncontrolled growth leads to various symptoms, including bone pain, osteoarthritis, fractures, and diminishing amounts of healthy blood cells (white blood cells and red blood cells). These newly developed cancer cells also start producing large amounts of proteins, that can cause kidney damage resulting in renal failure [1].
The treatment options for patients with myeloma & multiple myeloma have become much more effective thanks to recent advances in stem cell therapy, immunomodulation medications, and much better supportive care, which have led to much-improved survival rates over the past ten years. Traditionally the primary options for treatment included targeted (non-chemotherapy) medications that target cancer cells, corticosteroid infusions, standard chemotherapy, and modified bone marrow stem cell transplants [2].
Each patient’s needs are unique, and all options should be weighed carefully. Conventional therapies rarely cure cancer completely, so many patients end up having multiple treatment protocols during the overall course of their illness. Stem cell therapy is not appropriate in all cases. It might not be a good option for some patients due to several factors, including multiple commodities, advanced stage of cancer, advanced age or other physical limitations.
Care for your Cancer During Covid-19
COVID-19 or “coronavirus disease 2019.” It is an infection caused by the SARS-CoV-2 virus. This virus first appeared in 2018 and has since spread rapidly worldwide. Vaccinating for Covid helps lower the risk of severe illness; oncologists recommend getting the COVID-19 vaccination for anyone with active cancer or a history of cancer.
Early Detection, Diagnosis, and Staging
When should treatment for Myeloma start? — myeloma & MM can remain pretty stable in some patients for long periods. Some patients with onset myeloma who do not show symptoms are called smouldering myeloma. Patients with this condition may be recommended to wait several months before considering intervention treatment. However, patients at high risk for cancer progression may start treatment immediately. The Regeneration Center can discuss your options and help you determine when to start treatment[3].
Patients diagnosed with (MGUS) or monoclonal gammopathy of undetermined significance generally will not require treatment, but long-term monitoring is needed to ensure remission. Only a tiny percentage of patients diagnosed with MGUS eventually develop full-blown myeloma. Once the symptoms of MM cancer develop, immediate treatment with one or multiple options (discussed below) is recommended for nearly all cases.
Traditional treatments for Multiple Myeloma
There are nine main types of treatment for a patient with multiple myeloma. The options depend on several factors, including the age of diagnosis, if the condition has relapsed, the patient’s age and overall health.
- Newly developed cancer medications – There are currently several (non-chemotherapy) based medications developed recently for treating multiple myeloma. These cancer medications may be good options for recently diagnosed patients and those who have relapsed. Usually, these medications are combined with steroid medications (dexamethasone) or standard chemotherapy agents.
- Proteasome inhibitors – The proteasome is responsible for breaking down proteins in cells and is very active in multiple myeloma cells due to the excess protein produced. Proteasome inhibitors help to block the action of protein build, so these cells die. The Proteasome inhibitors can include Velcade (bortezomib), Kyprolis (carfilzomib), and Ninlaro (ixazomib). Usually, Velcade is given subcutaneously (under the skin), Kyprolis is given via IV, and Ninlaro is generally taken as oral pills. The side effects of these Proteasome inhibitors can include nerve damage and a higher risk of developing infections. If Velcade is given via IV, it can result in a much higher risk of developing nerve damage (neuropathy), so it is often not preferred.
- Immunomodulation medications – These more natural medications use the body’s immune system to fight the cancerous myeloma cells. They include Revlimid (lenalidomide), Pomalyst (pomalidomide), and Thalomid (thalidomide). However, these medications can potentially cause severe congenital disabilities in pregnant women and are therefore not recommended for expecting mothers. When Immunomodulation medications are given in combination with steroids, the meds can increase the risk of developing blood clots for some patients.
- Monoclonal antibodies – Monoclonal antibodies “MA” are considered purified proteins that are used to target specific groups of cells in the body. Monoclonal antibodies can treat myeloma by targeting the surface antigens of the cancer cells. There are several types of monoclonal antibodies currently available for use in the treatment of multiple myeloma. The most often used Monoclonal antibodies used today include Darzalex (daratumumab), Empliciti (elotuzumab), Sarclisa (isatuximab – isatuximab-irfc), and Blenrep (belantamab mafodotin). All Monoclonal antibodies are given intravenously, while Darzalex can be given subcutaneously also. Belantamab mafodotin is another antibody linked to chemotherapy, which is known to cause damage to the cornea of the eyes and, therefore, no longer recommended for most cases.
- Nuclear export inhibitor – Nuclear export machinery inside a cell transfers proteins out of the cell nucleus. Xpovio (Selinexor) is a new medication that can block this action so that the proteins build up, causing the cells to die. Xpovio can also be used in the treatment of multiple relapsed multiple myeloma.
- Chemotherapy – Chemotherapy cancer treatments refer to the use of certain medicines that can slow down or stop the prolifereation of cancer cells. For most patients, chemotherapy can help partially control multiple myeloma, and for some patients, traditional chemotherapy can lead to complete remission of Multiple Myeloma. Chemotherapy medications most often used for patients with multiple myeloma include Alkeran (melphalan), Cytoxan (cyclophosphamide), Adriamycin (doxorubicin), and Doxil (liposomal doxorubicin)).
- Stem cell transplants – Stem cell transplants can be done using the patient’s stem cells (autologous) or stem cells donated from a relative or matched donor (allogeneic). In cases of multiple myeloma, most stem cell transplants have been shown to control the spread, prevent relapse and prolong life. Modified stem cells can be used as part of the initial intervention (newly diagnosed) or in case of relapse. For some patients, more than one stem cell transplant session may be needed to control the growth of the disease adequately. Stem cell therapy for patients with multiple myeloma is generally a much safer option than chemotherapy, with significantly fewer side effects.
- Corticosteroids – Corticosteroids (steropids) are anti-inflammatory medications. Corticosteroids used in the treatment of Multiple Myeloma include prednisone & dexamethasone.
- “CAR-T” cell therapy – CAR-T cell therapy is another type of cell immunotherapy that can be effective in patients with refractory or multiple myeloma. CAR-T cell therapy requires genetically modifying cells taken from a patient’s immune system; this vector allows the modified cells to directly target the cancer cells without being seen as foreign. Gene therapy is also currently being used in clinical trials.
Treating Complications from Multiple Myeloma
Patients treated for Multiple myeloma can display a wide variety of complications including some that can be life-threatening. Some common complications can include the following:
- Loss or impaired renal function — Nearly 50% of patients with multiple myeloma report having impaired kidney function or development of lupus, diabetic nephropathy & kidney disease. Treatment for kidney failure can include Renal stem cell transplants, hemodialysis or peritoneal dialysis, prednisone and allopurinol for patients with PKD along with medication to lower uric acid. This waste product occurs after increased turnover of cancer cells resulting in damage to the renal system. Patients are encouraged to stay hydrated enough to produce about three litres of urine daily. Patients should also avoid using any NSAIDs such as Motrin, Advil or Aleve as they can cause worsening of kidney function.
- Elevated blood calcium levels: High blood calcium levels occur when the bone is lost. Patients with multiple myeloma are advised to remain physically active to help counter the risk of atrophy and bone loss. Treatment of higher than normal blood calcium levels can include prednisone with IV fluids. If traditional remedies fail, stem cell treatment for osteoporosis that can help act against rapid bone loss may also be recommended.
- Bone Fractures and pain: Physical Exercise can help promote bone strength for patients with multiple myeloma; however, extreme caution should be taken to avoid injuries which can complicate treatment options. Bone pain, including tenderness, aching, or other discomforts in the bone, can be controlled with pain-relieving medications, chemotherapy, and radiation therapy for strengthening bones and preventing ankylosing spondylitis or additional bone damage for patients with multiple myeloma. Patients with early bone erosion symptoms can use stem cell therapy to reduce bone pain and the risk of further fractures. Early intervention is recommended for all patients showing early signs of bone erosions on radiology scans.
- Infections: Bacterial and viral infections are usually found with fever and are often treated with powerful antibiotics. Continual use of antibiotics can help prevent some diseases. If patients are experiencing frequent infections, they are encouraged to get the flu and the pneumococcal vaccine which can help reduce the risk of pneumonia for high-risk patients.
- Spinal cord compression: Spinal cord injuries, including compression, requires immediate treatment to avoid irreversible damage, including transverse myelopathy and paralysis. Initial treatments can include radiation therapy and dexamethasone to help reduce Spinal cord oedema (swelling around the spinal cord). If available therapies fail, surgery might be required to relieve pressure. Patients experiencing severe back pain or DDD, weakness, connective tissue disease, neuropathy (numbness or tingling in the legs) or problems with bladder or bowel control or incontinence should contact their doctor and seek treatment immediately.
- Patients getting regular Dental procedures (root canal or teeth extraction) may be at a higher risk of acquiring infection or osteonecrosis of the jaw. Ideally, patients with MM should postpone such dental procedures until they have recovered and are in remission.
- Hyperviscosity syndrome: Thickening of the blood, also known as hyperviscosity syndrome, is rare and can be treated with plasmapheresis. Plasmapheresis is a type of blood filtration system used to remove excess monoclonal proteins causing the thickening.
- Anaemia: Low red blood cell count, also known as Anemia, may require patients to get blood transfusions or treatment with EPO (erythropoietin). Erythropoietin helps to stimulate the rapid production of red blood cells. EPO is most often given via injection several times per week. EPO therapy can help increase levels of haemoglobin protein in red blood cells that carry oxygen. EPO sessions can help improve several symptoms and reduces the requirement for blood transfusions.
TREATMENT PRECAUTIONS & RISKS
Please note cancer stem cell therapies and immunotherapy is not appropriate for all types of cancers. Risk is a part of any medical treatment. Though scientific based regenerative immunotherapies we can make treating of blood cancers like myeloma safer and a more reliable therapeutic option, however there are always the risks of complications and or developing side effects.It is important to discuss all treatment options with your primary care provider to find the best option for you.Relapsed or Refractory Multiple Myeloma
A very high percentage of patients who opt for traditional treatments for mesothelioma and multiple myeloma eventually relapse, and many are also resistant to initial interventions. The condition is classified as multiple refractory myelomas when patients do not respond or respond poorly. Non-responsive myeloma treatments can fail during the initial administration of chemotherapy or sometimes to the chemotherapy that is given after the initial relapse. From a treatment perspective, patients with multiple refractory myelomas are much more challenging to treat.
Patients with refractory myeloma or relapsed status are often treated with a combination of medications from several classes.
The main classes of medications that are used to treat refractory myeloma and relapsed patients are:
- Proteasome inhibitors, Including carfilzomib, bortezomib and ixazomib
- Monoclonal Antibodies targeting myeloma cells, including isatuximab, daratumumab, belantamab mafodotin and elotuzumab
- Immunomodulatory medications including pomalidomide, lenalidomide and thalidomide
- Modified Stem cell transplants
- Chemotherapy medications, including cyclophosphamide & melphalan
- Glucocorticoids such as dexamethasone
- Nuclear export inhibitors, including selinexor
A combination of these treatments can be used depending on the patient’s diagnosis, and all options have varying side effects. After each relapse, patients can try new protocols for meaningful benefits and improvements. Patients with relapses that occur after one year can also be treated again by repeating the initial chemotherapy regimen that was temporarily successful. A second session will work in most cases; however, the response is usually muted and less potent than the original course. If patients do not respond well to the initial round of chemotherapy, they can still be eligible for enhanced MSC+ stem cell transplantation or “CAR-T” therapy.
Stem Cell Transplants for Multiple Myeloma
Patients with Multiple Myeloma often need stem cell transplants to recover from the destructive nature of high-dose chemotherapy, which essentially destroys all the cells in the patient’s bone marrow. MSC+ Stem cell transplants allow for new healthy blood-forming hematopoietic stem cells, reduce apoptosis and induce angiogenesis. During the early days of stem cell research, the cells mostly came from bone marrow and were referred to as bone marrow stem cell transplants[4].
CAR T-cell therapy for Bone Cancer
Today, The Regeneration Center can modify T-Cells and harvest stem cells from multiple sources including peripheral blood, cord tissue and cord blood stem cells. Natural Killer “NK” cells and enhanced Mesenchymal cell transplants can be used to treat various myeloma without the toxicity and risk of chemotherapy. For some patients, a combination multi-stage treatment is needed to reduce the number of circulating myeloma cells & cancer stem cells before new transplants are given.
T-Cells Programmed to Attack Cancer Cells
Autologous vs Allogeneic Stem cell transplants
Autologous stem cell transplants use a person’s stem cells, which can be removed from peripheral blood or bone marrow. After the cells are collected, they are either cryogenically stored for future treatment or sent to our lab to begin the long cell isolation and expansion stage. Patients who opt for traditional myeloma therapies begin high-radiation chemotherapy to kill all the cancer cells. When chemotherapy is complete, the patients stored or lab-prepared stem cells are reintroduced into their system intravenously.
Patients with comorbidities or late stages might require 1 or 2 autologous stem cell transplants that are given in 6 to 12 months. The Regeneration Center uses this approach for some cases as research has shown that a staggering therapy can help some patients more than receiving just a single transplant.
Allogeneic Stem Cell transplants are when patients are receiving stem cells from a donor, i.e. another person, are referred to as allogeneic stem cell transplants. The best treatment results for patients needing allogeneic stem cells happen through matching donor cell types to patients. This is often much easier if the donor is closely related to the recipient. In cases with no matches, cord tissue-derived allogeneic stem cell transplants might be an option as it does not require HLA matching. Cord blood stem cell transplants are considered riskier than autologous stem cell transplants, but they might not be as potent or better at fighting cancer cells. Transplanted (Allogeneic) cells have the advantage that they can help destroy myeloma cells in what is referred to as the graft vs tumour effect.
Allogeneic stem cell transplants might be better options for patients with a variety of cancers, including kidney cancer, lung cancer, liver cancer, colorectal cancer, cancer in the pancreas and prostate cancer. Allogeneic stem cells are also often used for noncancerous diseases, including alcohol induced liver cirrhosis,TBI due to hypoxia, lung disease, crohns disease, incomplete spinal injuries, heart disease, alzheimers and degenerative disc disease.
Side effects of Allogeneic stem cell therapy
Some side effects from stem cell transplants are similar to the side effects from chemotherapy, only much less severe. One of the primary side effects is Low haemoglobin count, which can increase the risk of infection and bleeding. One of the main side effects of allogeneic transplants is graft-versus-host disease (GVHD). GVHD occurs when transplanted immune cells are marked as foreign and attacked. Graft-versus-host disease can affect multiple functions and can be life-threatening. For this reason, HLA matching is required to help match both patient and donor cells. If both people share the same HLA type, they are considered a ‘good match. I
If you or a loved one have been diagnosed with Multiple Myeloma, be aware of alternative medical solutions to fight cancer using MSC+ modified immune cells [5].Take the first step toward treatment by allowing your care to be handled by our team of experts in our advanced facility. We are here to help. To learn more about the safe and effective alternative treatment for Multiple Myeloma please contact us today.
Published Clinical Citations
[1] ^Wudhikarn K, Wills B, Lesokhin AM. Monoclonal antibodies in multiple myeloma: Current and emerging targets and mechanisms of action. Best Pract Res Clin Haematol. 2020 Mar;33(1):101143. doi: 10.1016/j.beha.2020.101143. Epub 2020 Jan 11. PMID: 32139009; PMCID: PMC7060936.
[2] ^Tan D, Lee JH, Chen W, Shimizu K, Hou J, Suzuki K, Nawarawong W, Huang SY, Sang Chim C, Kim K, Kumar L, Malhotra P, Chng WJ, Durie B; Asian Myeloma Network. Recent advances in the management of multiple myeloma: clinical impact based on resource-stratification. Consensus statement of the Asian Myeloma Network at the 16th international myeloma workshop. Leuk Lymphoma. 2018 Oct;59(10):2305-2317. doi: 10.1080/10428194.2018.1427858. Epub 2018 Feb 2. PMID: 29390932.
[3] ^ Xu S, De Veirman K, De Becker A, Vanderkerken K, Van Riet I. Mesenchymal stem cells in multiple myeloma: a therapeutical tool or target? Leukemia. 2018 Jul;32(7):1500-1514. doi: 10.1038/s41375-018-0061-9. Epub 2018 Feb 22. PMID: 29535427; PMCID: PMC6035148.
[4] ^Huff CA, Matsui W. Multiple myeloma cancer stem cells. J Clin Oncol. 2008 Jun 10;26(17):2895-900. doi: 10.1200/JCO.2007.15.8428. PMID: 18539970; PMCID: PMC2610256.
[5] ^Giuliani N, Mangoni M, Rizzoli V. Osteogenic differentiation of mesenchymal stem cells in multiple myeloma: identification of potential therapeutic targets. Exp Hematol. 2009 Aug;37(8):879-86. doi: 10.1016/j.exphem.2009.04.004. Epub 2009 May 14. PMID: 19446662.