Blastocyst are embryos that has undergone development five or six days post fertilization period. The number of cells that a human blastocyst may contain ranges between 70 and 120. Blastocyst occur after the morula enters the females uterine cavity and develops a fluid-filled cavity. The morula then becomes what appears to be a hollow ball of cells that is also known as a blastocyst.
The development of a blastocyst is a critical stage in early embryonic development. Let’s discuss the key stages leading up to, and including, blastocyst formation, as well as the process of blastocyst transfer:
Stages of Embryonic Development Leading to Blastocyst Formation:
- Fertilization: This is when a sperm successfully penetrates and fuses with an egg (oocyte), resulting in a zygote. This usually occurs in the fallopian tube.
- Cleavage: The zygote begins to divide, undergoing several rounds of mitotic division. This results in a series of developmental stages with increasing numbers of cells:
- 2-cell stage
- 4-cell stage
- 8-cell stage, and so on.
- Morula: This stage typically occurs around 3-4 days post-fertilization. The embryo is a solid ball of cells.
- Blastocyst Formation: By day 5 or 6 post-fertilization, the embryo transforms into a blastocyst. The blastocyst consists of:
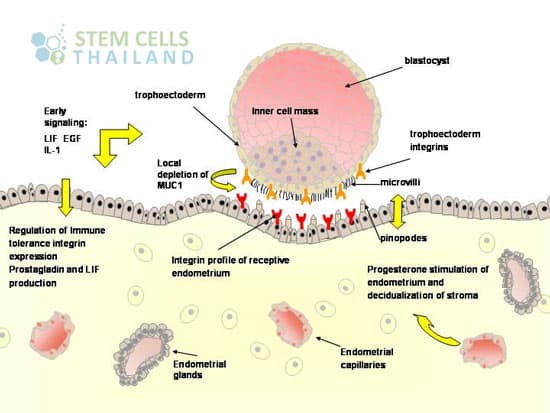
- An outer layer called the trophectoderm (or trophoblast), which will eventually contribute to the formation of the placenta.
- A fluid-filled cavity called the blastocoel.
- A group of centrally located cells called the inner cell mass (ICM), which will develop into the fetus.
Blastocyst Transfer:
Blastocyst transfer is a procedure commonly used in in vitro fertilization (IVF) treatments. The process involves:
- Culturing Embryos: After fertilization in the lab, embryos are cultured for 5-6 days until they reach the blastocyst stage.
- Selection: The best-quality blastocysts are selected for transfer. The selection is based on the appearance and developmental progress of the blastocysts.
- Transfer Procedure: A thin catheter is loaded with the selected blastocyst(s) and is carefully inserted through the cervix into the uterus, where the blastocyst is gently deposited.
- Implantation: If successful, the blastocyst will start to implant into the uterine lining a few days after the transfer. This is the beginning of pregnancy.
- Excess Blastocysts: Any remaining high-quality blastocysts can be cryopreserved (frozen) for future use.
There are several advantages to transferring embryos at the blastocyst stage:
- Higher Implantation Rates: Blastocysts have a higher potential for implantation compared to embryos transferred at earlier stages.
- Improved Selection: It’s easier for embryologists to select the most viable embryos for transfer when they’ve reached the blastocyst stage.
- Reduced Risk of Multiples: Because of the higher implantation potential, fewer blastocysts can be transferred, reducing the risk of multiple pregnancies.
However, there’s also a risk that none of the embryos will develop into blastocysts, which means there would be nothing to transfer. The decision to conduct a blastocyst transfer is typically made in consultation with fertility specialists, considering various factors including the age of the woman, the quality and number of embryos, and previous IVF outcomes.
Blastocyst Development Video
Within the blastocyst certain cells group together to form the inner cell mass that later goes on to becomes the embryo.