Spinal cord injuries occur in many ways, such as a traumatic accident or hit to the spine that results in a burst fracture of the vertebrae. The damage begins on impact when displaced bone fragments and ligaments tear into or bruise spinal tissue. Most spine injuries do not completely sever the spine and cause enough damage to cause fractures that can disable or destroy the axons. As the signal carriers of the human body, axons carry electric signals and act as messengers between the body and the brain. Most spinal injuries usually cause damage to some or all of the axons.
The spinal cord is a thick bundle of nerves designed to carry signals between the brain and the rest of the body, crucial for functional recovery after spinal cord injury. Acute spine injuries (SCI) usually occur after sudden and traumatic Injury. The SCI can be as minor as a contusion (bruise), a partial tear, or a complete spinal tear (transection). Spinal injuries are also more common in young adults and men.
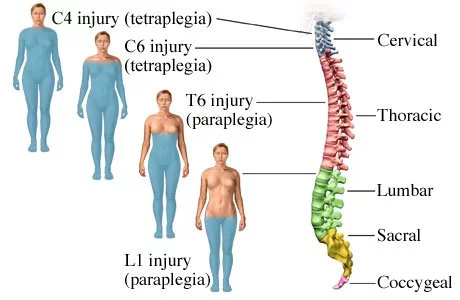
A traumatic spinal injury can result in an instant loss of movement, touch, and feeling and a reduction in organ function below the damaged vertebrae. The most common areas of spinal injuries are in the cervical ( neck ) and thoracic spine areas. Spinal injuries are one of the most common causes of permanent disability and death in both children and adults, highlighting the need for effective treatment of spinal cord injury.
The human spine consists of 33 vertebrae in total, including:
These 33 vertebrae help form our spine and protect the spinal cord and nerve bundles. Generally speaking, the higher the spine injury, the more severe the patient’s symptoms are. Injuries to the vertebrae do not necessarily mean the spinal cord is damaged, and damage to the spinal column can occur without dislocations or breaks in the vertebrae, such as in patients with spinal inflammation caused by transverse myelitis.
Spinal injuries are usually classified into two main categories:
Survivors of SCI from sports-related injuries also start suffering from other medical complications, such as chronic pain or bowel and bladder dysfunction with increased susceptibility to severe brain fog & having heart or respiratory problems. The success of any cellular treatment depends entirely on how well our doctors can manage systematic failures and chronic conditions through targeted regeneration therapy.
Cell-based treatments take a more proactive approach and boost humans’ natural repair cycle by stimulating/enhancing damaged cells and tissue repair. Repairing an injured spinal cord & bamboo spine requires going beyond traditional techniques to help you regain some/all of the lost functions. Clinical trials have shown that cell turnover and death are expected and occur naturally when the body’s cells are injured or aged. These dead cells are usually surrounded by healthy and damaged cells, which can influence recovery after spinal cord injury. Our treatment protocol for Sciatica and spinal stenosis helps boost the healing of these dead or injured cells through targeted cytokine therapy that uses nerve growth factors and paracrine signaling to trick the body into restarting the healing process.
The Regen Center offers a unique combination protocol for the treatment of neurological & spinal cord injuries using a targeted multi-step approach. Once our medical team has reviewed the patient’s current medical condition and determined the appropriate course of action, a detailed plan will be provided. If the patient does not have the quality or quantity of enhanced mesenchymal stem cells, cord tissue-derived mesenchymal stem cells (UC-MSC+) will be needed to treat spinal cord injury effectively. If required, these cells can be stored using our cryopreservation facility for over 20 years, Research has focused on olfactory ensheathing cells, stem cell differentiation tactics, glial cell line-derived neurotrophic factors and isolating neural stem cells for subacute and adult stem cells for chronic spinal cord repair.
Treatments for severe cases with extensive nerve cell atrophy require expanded UC-MSC+ mesenchymal stem cells and nerve cell growth factors injected near the damaged spinal areas via a CT-guided intra-spinal machine. The UC-MSC+ protocol for paralysis due to spinal cord injury is unique as it is the only treatment in the world that offers supplemental injections with nerve cell-specific growth factors to enhance recovery further using IV drip injections, lumbar punctures, Intrathecal injections, fluoroscopy guided (in a hospital setting only) depending on the severity of the patient’s injuries or if the patient is paralyzed to promote functional recovery following spinal cord injury.
Enhanced UC-MSC+ stem cell injections are the platinum standard in modern regenerative medicine, especially when treating spinal cord transection. The precision of cellular guidance allows our team to aim directly at adjacent areas of lesions or Injury. UC-MSC+ enhanced spinal treatment does not require dangerous open spine surgeries. UC-MSC+ stem cell injections and neural progenitor cell infusions also help patients avoid the risks and pain of additional surgeries associated with traditional treatments for the injured spinal cord.[1]
Our spinal injury treatment center aims to help repair damage naturally and safely. Our treatment protocols are designed to bypass the blood-brain barrier and take place on the cellular level to positively affect the areas near the point of impact, particularly the glial cell populations. Positive results can be dramatic if the Injury is less than two years old. For those with older injuries, the potential for functional recovery after spinal cord injury may be limited but still possible. traumatic brain injuries, severely degenerative spinal discs, osteonecrosis, peripheral neuropathy, or spinal muscular atrophy, the chances of full recovery become significantly more complicated over time.
Promote Neural Regeneration:
Enhance Functional Recovery:
Reduce Inflammation and Scar Tissue:
Support for Implanted Cell Survival and Integration:
Improve Quality of Life:
Newer tissue, cartilage, or ligament injuries respond much better to stem cell treatments. The recovery after treatment will require a lot of dedication and rehabilitation sessions. Physical improvements occur around 2-3 months after the initial treatment, and the results are permanent, significantly enhancing recovery after spinal cord injury.[2]
Treatment prices and costs at our stem cell treatment center for spinal damage depend on the severity of the Injury and the protocol needed.
The treatment requires an estimated 14-31 day stay in Bangkok, Thailand. To evaluate your suitability for our spinal treatment protocol, we must review recent radiology scans (MRIs, CT scans) and a clinical diagnosis from your primary care physician or a specialist in your home country. Once this information is reviewed, we will provide a complimentary treatment plan with fixed pricing. The final treatment plan will include all associated costs, such as hospital fees, rehabilitation, doctors’ fees, lab work, stem cell collection, and cell expansion. Additionally, we offer short-term apartment options for patients and their families. Residents of Canada, the United Kingdom, Australia, and the United States may also qualify for medical financing. Please get in touch with us for more details.
To learn more about our combination UC-MSC+ stem cell therapy for acute spinal cord injuries, please contact us.
[1] ^ Amr, Sherif M, Ashraf Gouda, Wael T Koptan, Ahmad A Galal, Dina Sabry Abdel-Fattah, Laila A Rashed, Hazem M Atta, and Mohammad T Abdel-Aziz. 2013. Bridging defects in chronic spinal cord injury using peripheral nerve grafts combined with a chitosan-laminin scaffold and enhancing regeneration through them by co-transplantation with bone-marrow-derived mesenchymal stem cells: case series of 14 patients. The journal of spinal cord medicine, no. 1 (November 26). doi:10.1179/2045772312Y.0000000069. https://www.ncbi.nlm.nih.gov/pubmed/24090088″ target=”_blank” rel=”noopener noreferrer”>https://www.ncbi.nlm.nih.gov/pubmed/24090088
[2] ^ Dajpratham, Piyapat, and Racharin Kongkasuwan. 2011. Quality of life among the traumatic spinal cord injured patients. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 10. https://www.ncbi.nlm.nih.gov/pubmed/22145512
[3] ^ Piltti, Katja M, Desiree L Salazar, Nobuko Uchida, Brian J Cummings, and Aileen J Anderson. 2013. Safety of human neural stem cell transplantation in chronic spinal cord injury. Stem cells translational medicine, no. 12 (November 4). doi:10.5966/sctm.2013-0064. https://www.ncbi.nlm.nih.gov/pubmed/24191264