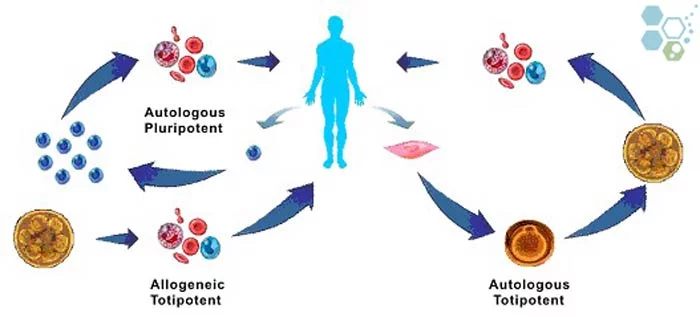
Autologous stem cells such as Adipose tissue derived stem cells are the opposite of allogenic stem cells, as only one patient stands as both donor and receiver.
Autologous Stem Cell Therapy
The stem cells will be harvested from the patient’s body, most common location of which is the bone marrow, and will be transplanted back to the patient for treatment of a variety of conditions including: shoulder injuries, Acute coronary syndrome,diastolic heart failure, als fasciculations and anoxic brain injuries.
Autologous stem cell transplantation (ASCT) is a procedure in which a patient’s own stem cells are harvested, stored, and then returned to the patient after they’ve undergone a high dose of chemotherapy and/or radiation. This procedure is often used to treat certain types of cancers, especially hematological malignancies such as lymphoma and multiple myeloma.
Autologous stem cell transplantation has the advantage of using the patient’s own cells, which reduces the risk of graft-versus-host disease (GVHD), a potential complication of allogeneic transplants where donor cells attack the recipient’s tissues. However, ASCT is still a major medical procedure with potential risks and complications, and decisions regarding its use should be made in close consultation with a medical oncologist or hematologist.
Zombie cells, also called senescent cells, are non-dividing cells that accumulate in the body due to stress or damage, resisting… Read More
Chimeric antigen receptor-T cell treatment (CAR-T cell therapy) holds immense potential to revolutionize organ transplantation, particularly for patients who struggle… Read More
In the ever-evolving landscape of nutrition science, the discourse around dietary fats has undergone significant transformation. The Regeneration Center is… Read More
New research shows that specific types of brain cells become active after brain injuries and exhibit properties similar to those… Read More
Chemokines, critical components in the immune system, are small proteins that facilitate the migration and positioning of immune cells throughout… Read More
Stem cell research examines everything from gene expression to differentiation capacities to therapeutic potentials. With such diverse data types and… Read More