If a person’s motor neurons are not functioning well, they will experience significant problems with their movements, such as walking, standing up, turning, breathing, eating, speaking, and swallowing. The paracrine cell communication system carries signals from the brain to the muscles. People can perform movements through a complex process involving neurons.
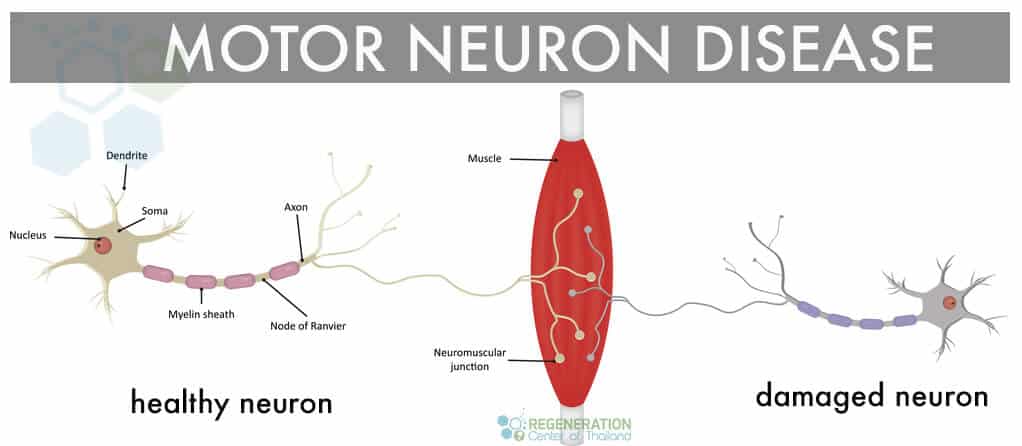
Motor neurons are mostly just nerve cells responsible for managing muscles in the body to move. Motor Neuron Disease, or “MND,” is a rapidly progressive neurological disease that damages motor neurons essential for controlling our movement. Nerve cells from the brain transmit messages to the nerve cells in the spinal cord, which are then distributed to different muscles in the body.
MND disorders are a family of conditions, and there are several classifications of motor neuron diseases depending on the patient’s symptoms and underlying causes, including:
Early symptoms of MND often affect specific areas in the body before they eventually spread to other places. Early diagnosis is critical to managing this condition and improving overall survival, so visiting a neurologist after any early symptoms is essential. There are typically three stages of MND including early, middle, and advanced (terminal MND)
Early-stage symptoms of MND are often confused with other types of unrelated neurological disorders, and the diagnosis is frequently changed after further testing. The initial signs and warning signals of MND depend upon where the disease manifests first. Typical symptoms for patients with onset MND are in the mouth ( bulbar) region, arms, legs, or lungs (respiratory system).
Symptoms of Stage 1 MND include:
As MND gets more advanced, the symptoms get more noticeable after several functions in the body are affected.
Symptoms of MND Stage 2 include:
Some secondary symptoms of advancing MND can include depression, persistent anxiety, and insomnia.
Symptoms of Advanced Stage MND (End-stage) – As the neurodegenerative effect worsens eventually, the patients are unable to eat, move, or breathe without assistance. At this stage, options are minimal, and stem cell therapy is likely not an option once the attacks have researched a phase of increasing body paralysis where patients cannot function without supportive care. Respiratory failure is typically the most common complication of MND that leads to patient death. In contrast, others become unconscious or fall into a deep sleep from which they can pass peacefully.
MND is diagnosed when the motor neurons (nerve cells) in the spine and brain lose their function. Although a lot of research has been the underlying cause of MND is still unknown but is generally attributed to environmental (sporadic) factors, familial (hereditary/genetic) causes, or a combination of the 2. In 90% of cases with MND, the patient does not have a family history; however, genetic testing was not prevalent in previous generations, so this hypothesis is likely to be changed. Most researchers studying MND believe that the cause of neural dysfunction and premature neuronal death is probably a combination of damaging environmental and genetic factors. As humans gradually age, we lose the ability to repair the damage, resulting in irreversible neurodegeneration. Research on MND, Strokes, Mixed Non-Fluent Aphasia, and Parkinson’s Disease is continuing, and it involves attacking the immune and genetic factors, toxins, viruses, and nerve growth factors that affect the activity of motor neurons. Other factors that are somewhat related to the development of MND include an autoimmune pathogenesis, exposure to toxins via smoking, and repeated head injuries, as is with professional athletes in professional fighting, mixed martial arts, or the NFL. Residents of countries such as Japan, Guam, and New Guinea also have a much higher percentage chance of exposure to chemicals and radiation, possibly due to current/previous military-industrial-related activities.
Some causes for environmental/sporadic MND include:
It’s important to note that familial and sporadic MND symptoms are nearly identical and can only be differentiated on the genetic level. The causes of motor neuron disease and Multiple Sclerosis are still unknown. Various environmental factors have been identified to lead to neurodegenerative disease. They can include exposure to environmental toxins, heavy metals like lead, pesticides, DDT, dieldrin, chemical exposure, serum uric acid, toxaphene, and organochlorines.
Evidence is still inconclusive, but some other linked environmental factors for MND include:
Mutations in a human gene happen when the set of instructions (inside the cells) gets damaged somehow. This results in the same error being replicated in new cells, which causes dysfunctions like MND. Familial MND is rare but can only be verified using proactive testing for mutated genes. The fact that MND can be passed on genetically suggests that single mutations inherited from the parents may sometimes play a much more significant role in developing the condition later in life. Clinical diagnosis for Hereditary MND necessitates mutations in at least 2 (or more) genes due to oligogenic inheritance.
The Regeneration Center does not offer gene therapies for MND. Still, it does provide DNA mutation tests for MND with confirmed diagnoses to determine if they have one or more mutated genes associated with heredity MND. We offer DNA gene sequencing tests for over 40 variants linked to MND, hereditary motor neuropathy (HMN), neuronal ceroid lipofuscinoses (NCL) disorders and genetic prion disease including C9ORF72, ALS2, TBK1, SOD1, PRNP, DCTN1, SPG11, HEXB, TARDBP, KIF5A, FUS, OPTN, PFN1, SETX, CHCHD10, CHMP2B, MATR3, UBQLN2, VAPB, TFG, VCP, BCKDHA, BCKDHB, DBT, PPM1K, SIGMAR1, ATP7B and SQSTM1.
It can often be challenging to diagnose MND in the early stages because the symptoms of MND are often similar to other neurological conditions like Parkinson’s disease & multiple sclerosis (MS). For most patients, a general physician will recommend that a neurologist review the patient’s symptoms and request additional diagnostic tests to confirm a diagnosis. A neurologist starts with a review of the patient’s complete health history and physical symptoms of the neurologic disorder.
Tests that are used to confirm MND include:
After the test, a doctor can use inclusion criteria about the patient’s symptoms to determine if the patient has ALS. The most commonly used set of criteria doctors use to diagnose MND/ALS is the El Escorial criteria. [1]
The typical symptoms of upper motor neuron disease include frequent cramps, recent weight loss, difficulty swallowing, random muscle twitching, excessive muscle wasting or weakness, fatigue, slurred speech, and drastic emotional changes. Motor neuron disease cannot be reversed. The patient and their family must make significant adjustments to help cope with this disease. The average life expectancy of someone who is diagnosed with ALS or MND without any interventional treatment is 1 to 5 years. There are different types of MND, and many of them can be fatal if left untreated. Patients with neuronal disease can go through a plateau phase where symptoms remain stable for some time, but the condition will eventually worsen. Primary Lateral Sclerosis is a type of MND that is less fatal and progresses gradually. As the disease progresses, people with MND will develop generalized paralysis, difficulty swallowing, loss of speech, and total dependence on other people in performing day-to-day activities. People who care for MND patients should also adjust to the patient’s deteriorating condition.[2]
Please note that treatments for motor neuron disease are much more effective in the earlier stages. New clinical trials and recent advances in neuro stem cell medicine using exosomes to bypass the blood-brain barrier have shown considerable promise in helping manage progressive muscular atrophy much more effectively, increasing life expectancy and quality of life for patients with mild to moderate stage MND. [3]
Any success relies on proper and consistent management in relieving symptoms. Muscle relaxants and prescribed Pain relievers such as morphine are not a long-term solution and only mask the underlying brain degeneration. Stem cell treatment for motor neuron disease focuses on the underlying issues leading to rapid muscle atrophy and nerve cell death using isolated and expanded neural stem cells along with progenitor cells and neurotrophic growth factors that help to secrete growth factors that lead to neurogenesis and the production of three types of nerve cells including oligodendrocytes, astrocytes, and neuron cells. Motor neuron replacement can be isolated in the ventral horn, bran, and innervate striated muscle to induce the proliferation of new cells and restore proper function. [4]
Mesenchymal Stem cells are un-specialized cells in your body that can change into any tissue or cell (neuro) in the human body. Stem cells are unique as they can reproduce and divide indefinitely. The motor neuron disease treatment with stem cells is non-surgical and minimally invasive. We offer several Stem cell treatment protocols for many diseases and disorders, including:
To qualify for the treatment of nerve damage, patients with upper or lower motor neuron disease must have an existing clinical diagnosis with tests to support the findings. A clinical diagnosis may take several months and include laboratory tests, such as MRIs, Brain CT Scans, electromyography, nerve conduction tests, transcranial magnetic stimulation tests (TMS), spinal taps, muscle biopsies, blood tests, and urinalysis. The Regeneration Center of Thailand offers functional medical treatments that focus primarily on repairing damaged or diseased tissues and replacing the neural capacity through neural cell replacement therapy brought about by the rapidly degenerative disease. [5]
Total Number of UC-MSC+ Cell Sessions for MND: For most patients, we will recommend multiple Infusions of isolated and expanded mesenchymal cells, which can be cultured from autologous sources or allogeneic sources (UC-MSC) of Neural Stem cells (MSC–NSC). These stem cells, and our proprietary mix of growth factors are joined to enhance the therapeutic potential of the treatment. The growth factors we isolate and culture are naturally occurring proteins in cells that stimulate cell growth, proliferation, healing, and differentiation and are combined with stem cells to support brain repair and regeneration. Some of the growth factors we isolate for MND patients include Brain-Derived Neurotrophic Factor (BDNF), Insulin-like Growth Factor 1 (IGF-1), Glial Cell Line-Derived Neurotrophic Factor (GDNF), Nerve Growth Factor (NGF), Epidermal Growth Factor (EGF), Vascular Endothelial Growth Factor (VEGF) and Fibroblast Growth Factors (FGFs).
Delivery Methods of UC-MSC+ and Neural Stem Cells: The delivery methods will vary based on patient needs. However, one of the main goals is to help reduce systemic neuroinflammation and promote faster recovery of lost cognitive function through neurogenesis. To achieve these results, the cells and growth factor complex can be administered using a combination of Intravenous infusions, intramuscular injections, stereotactic-guided delivery, inhalation therapy via micro-nebulized mesenchymal cells, Intrathecal infusions, and fluoroscopic guided cell delivery (in a hospital setting only). All intrathecal injections at The Regeneration Center are done by a board-certified neurosurgeon and are needed to bypass the blood-brain barrier. Healing the blood-brain barrier (BBB) can be a crucial part of treatment because it plays a vital role in maintaining the stability of the brain’s environment and protecting it from harmful substances. Learn how to boost neural stem cells naturally.
Rehabilitation for “MND” Motor Neuron Disease: Rehabilitation therapy will be required after the treatment. Physical Rehabilitation can take place after MND treatment in Thailand or any country in the world that offers physical and speech rehabilitation services. Post-treatment rehab facility options will be provided upon request. Medical visas and accommodations for an extended stay can also be included as necessary.
Due to varying degrees of severity, the total and exact cost of our stem cell therapy for motor neuron disease using neural stem cells will depend entirely on the patient’s actual medical needs. Our neurological stem cell team will need to better understand the patient’s needs before being able to offer a detailed treatment plan. Our neural regeneration protocol requires an initial medical review that can be done online or in person. Our medical review team will require the patient’s recent medical records, including any diagnostic exams such as Brain MRIs or CT Scans, to evaluate a potential patient. To begin assessing for our unique multi-stage MND treatment, please contact us today.
[1] ^ Agosta, Federica, Ammar Al-Chalabi, Massimo Filippi, Orla Hardiman, Ryuji Kaji, Vincent Meininger, Imaharu Nakano, et al. 2014. The El Escorial criteria: strengths and weaknesses. Amyotrophic lateral sclerosis & frontotemporal degeneration, no. 1-2 (December 8). doi:10.3109/21678421.2014.964258. https://www.ncbi.nlm.nih.gov/pubmed/25482030
[2] ^ Naujock, Maximilian, Nancy Stanslowsky, Peter Reinhardt, Jared Sterneckert, Alexandra Haase, Ulrich Martin, Kwang-Soo Kim, Reinhard Dengler, Florian Wegner, and Susanne Petri. 2014. Molecular and functional analyses of motor neurons generated from human cord-blood-derived induced pluripotent stem cells. Stem cells and development, no. 24 ( 15). doi:10.1089/scd.2014.0180. https://www.ncbi.nlm.nih.gov/pubmed/25007389
[3] ^ Phanthumchinda, K, O Supcharoen, and E Mitrabukdi. 1996. Madras pattern of motor neuron disease: case report from Thailand. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 6. https://www.ncbi.nlm.nih.gov/pubmed/8855616
[4] ^ Sarlak, Golmaryam, Anorut Jenwitheesuk, Banthit Chetsawang, and Piyarat Govitrapong. 2013. Effects of melatonin on nervous system aging: neurogenesis and neurodegeneration. Journal of Pharmacological Sciences, no. 1 (August 27). https://www.ncbi.nlm.nih.gov/pubmed/23985544
[5] ^ Terashima, Tomoya, Hideto Kojima, Hiroshi Urabe, Isamu Yamakawa, Nobuhiro Ogawa, Hiromichi Kawai, Lawrence Chan, and Hiroshi Maegawa. 2014. Stem cell factor-activated bone marrow ameliorates amyotrophic lateral sclerosis by promoting protective microglial migration. Journal of Neuroscience Research, no. 7. https://www.ncbi.nlm.nih.gov/pubmed/24936617