The connective tissues in the human body are the structural components that hold the body’s cells together. These tissues form a matrix (framework) for the body and are composed of two major structural protein molecules: elastin and collagen. Several types of collagen protein vary in quantity depending on which body’s tissue they are found. Elastin protein can stretch and return to its original length, like springs or a rubber band. Elastin is also one of the significant components of tissues that attach bones to other bones (ligaments) and our skin. Patients with connective tissue disorders often display damage to elastin and collagen due to chronic inflammation.
Connective tissue disorders are a group of medical conditions. A connective tissue disease (CT) diagnosis is made when the connective tissues in the body are the primary target of pathology. Patients with connective tissue diseases often show abnormal immune system function with significant inflammation in the tissues due to autoimmune attacks (the immune system attacks its body tissues) [1]
Any diseases in which collagen is weak or inflamed are called collagen diseases. For some patients, collagen vascular disease is diagnosed because the connective tissues are associated with abnormalities in blood vessels.
For many patients, a diagnosis is considered idiopathic (unknown cause). For others, direct links can be traced to genetic factors, which can increase the risk of developing connective tissue disorders. For others, a diagnosis is likely due to a combination of environmental factors ( exposure to toxins) and genetic predispositions resulting in the development of connective tissue disorder.
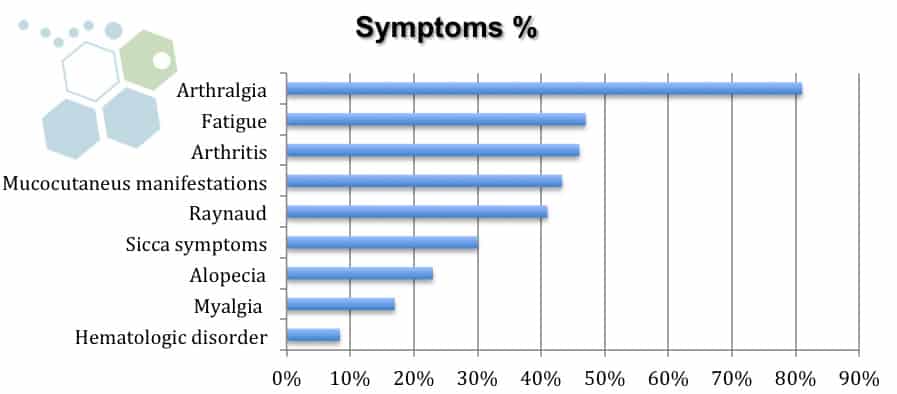
A prevalent symptom of connective tissue disease is premature fatigue, which can sometimes be misdiagnosed as FMS or CFS. Other indicators of (mixed) connective tissue disease include:
Several tests can be done to identify particular types of connective tissue disease. This can be done via a simple physical examination but often requires several rounds of blood tests, radiology scans, and genetic screenings to get clinically diagnosed with connective tissue disease.
Several types of connective tissue diseases are caused directly by genetic (familial) inheritance, including:
Other connective tissue disorders cannot be regularly attributed to gene abnormalities (scleroderma & systemic lupus erythematosus). These connective tissue disorders can occur for unknown reasons but may display weaker gene factors predisposing them to develop the disease. This group is sometimes characterized by overactivity in the immune system, resulting in significant additional antibodies in the blood circulation. To learn more about our genetic screenings for autoimmune and connective tissue diseases, visit here.
The cause of idiopathic connective tissue disease is not known. The Regeneration Center believes that the disorder can be triggered by environmental factors, especially among those who may already be genetically susceptible to some patients who are diagnosed with Type 1 Diabetes [4]. In such cases, the protective immune system malfunctions, producing specific antibodies that attack the body’s tissues.
These autoimmune diseases are considered classical connective tissue disorders because they have a “classic” / typical presentation that most physicians can quickly recognize using tests & examinations. Each classic symptom also shows blood test abnormalities in specific antibodies commonly found during blood and pathology tests. However, it should be noted that the progression rates of each classic symptom vary from patient to patient, with some evolving very slowly or rapidly.
For some patients in the early stages, the diagnosis is considered “undifferentiated” as CVD (collagen vascular disease) or UCTD (undifferentiated connective tissue disease) until additional symptoms appear. The change from CVD to UCTD may occur over the years or never materialize. In some cases, the undifferentiated features might disappear entirely, at which point there is a detectable disease resulting in a natural cure. If a patient has more than one type of autoimmune connective tissue disease, the condition is often classified as overlap syndrome.[5]
One common overlap syndrome is shared by diseases such as lupus, scleroderma, and polymyositis; these are called MCTD (mixed connective tissue disease) & Sharp’s syndrome.
Current medicinal treatment options for mixed connective tissue disease can help manage the signs and symptoms and are prescribed depending on the stage and severity of the diagnosis and patient symptoms. Traditional medications for the disease can include:
Compared to traditional medical treatments such as immunosuppressive medications and biologicals, UC-MSCs+ stem cell transplants for connective tissue diseases do not just suppress the patient’s immune system. Still, they can promote fundamental changes in the immune system, which are vital for long-lasting remission. Other benefits of stem cells for MCTD include:
The Regeneration center protocol combines isolated UC-MSC+ stem cells with several types of growth factors, including:
Our proprietary stem cell treatment for Connective Tissue Diseases & mixed connective tissue diseases requires 10-14 days in total helps in restoring cytokine imbalances, inducing angiogenesis, modulation of the immune system, and reparative effects of UC-MSC+ stem cell transplants.
The human joints are discrete organs of various connective tissues, including tendons, cartilage, bone, ligaments, and muscles. Any trauma or degeneration in these tissues can cause joint dysfunction, which leads to restricted function and movement. In the past, this means having risky, common surgeries. Recent studies have shown that nearly 45% of all adults live with some joint-related condition. This number is almost the same as those diagnosed with type 2 diabetes, heart disease, heart attacks, heart failure, COPD (chronic respiratory diseases), or pulmonary fibrosis combined.
In orthopedics’, the demand for minimally invasive stem cell therapies is also driven by the lack of adequate alternative treatments for common connective tissue degenerative diseases such as spinal arthritis. Several progenitor and self-renewable stem cell types can be differentiated into multiple musculoskeletal cell lineages. Due to rapid advancements in molecular biology and stem cell science, regenerative therapies have emerged as effective treatments for existing joint-relevant connective tissue diseases. They can help preserve healthy joints for years to come.
To treat immune-mediated inflammatory disease, The Regeneration Center has developed a unique combination therapy using isolated UC-MSC+ stem cells and tissue-specific growth factors that are particularly effective in stabilizing an otherwise abnormal rate of osteogenic differentiation. UC-MSC+ cells are engineered to provide low immunogenicity and immunomodulatory properties. UC-MSCs+ therapy for connective tissue disorders does not require immunosuppressive medications. The UC-MSC+ cells used can be autologous or allogeneic. Allogeneic UC-MSC+ cells do not express HLA-DR, which makes them the ideal therapeutic medium for transplantation in patients with immune-mediated disorders. UC-MSC+ can eradicate dysfunctional cells and restart the immune system by replacing damaged cells with cells differentiated into standard B and T cells required for immune system homeostasis.
Total Number of UC-MSC+ Cell Infusions: Total Endogenous Cell Count, UC-MSC+ Cell count, and tissue-specific growth factors will vary based on patient symptoms.
Types of Injections for Treating SLE: UC-MSC+ Mesenchymal Stem Cells. Depending on the severity of the patient’s needs, treatment injections will be made via Intravenous Drip, Intra-Articular Injections, Subcutaneous Injections, Intramuscular Injections, Intrathecal injections, or a combination of methods using multiple delivery routes. Patients with various conditions may require cell delivery via CT-guided scope (Hospital Setting Only)
Rehabilitation Post Treatment: Physical Rehabilitation in Bangkok is optional but highly recommended. Complete physical rehab services post-therapy can be provided upon request for 2-3 hours per day and up to 5 days per week.
Total Treatment Time Required: It is estimated to be around two weeks (depending on the type and seriousness of the condition). Medical and travel visas for extended accommodations at a hotel or apartment for the patient and family can also be provided upon request.
The cost of treatment of dense regular connective tissue, collagen vascular disease, and overlap syndrome will vary depending on degrees of severity. Our medical team will need to evaluate the patients using current medical records. Evaluations can be done in person or online (submitting documents online). After review, a detailed treatment plan will be provided that will include the specifics, such as the total number of nights required and total medical costs for treatment of connective tissue disease with stem cells. Please prepare all current medical records and contact us today to begin the evaluation process.
[1] ^Peng, Hairong, and Johnny Huard. “Stem cells in the treatment of muscle and connective tissue diseases.” Current opinion in pharmacology vol. 3,3 (2003): 329-33. doi:10.1016/s1471-4892(03)00051-1 https://www.ncbi.nlm.nih.gov/pubmed/12810201
[2] ^ Usas, Arvydas, and Johnny Huard. “Muscle-derived stem cells for tissue engineering and regenerative therapy.” Biomaterials vol. 28,36 (2007): 5401-6. doi:10.1016/j.biomaterials.2007.09.008 https://www.ncbi.nlm.nih.gov/pubmed/17915311
[3] ^Seong, Jeong Min et al. “Stem cells in bone tissue engineering.” Biomedical materials (Bristol, England) vol. 5,6 (2010): 062001. doi:10.1088/1748-6041/5/6/062001 https://www.ncbi.nlm.nih.gov/pubmed/20924139
[4] ^Zha, Kangkang et al. “Recent Advances in Enhancement Strategies for Osteogenic Differentiation of Mesenchymal Stem Cells in Bone Tissue Engineering.” Frontiers in cell and developmental biology vol. 10 824812. 23 Feb. 2022, doi:10.3389/fcell.2022.824812 https://www.ncbi.nlm.nih.gov/pubmed/35281084
[5] ^ Derakhshan, Tahereh et al. “Human Mast Cell Development from Hematopoietic Stem Cells in a Connective Tissue-Equivalent Model.” Tissue engineering. Part A vol. 25,21-22 (2019): 1564-1574. doi:10.1089/ten.TEA.2018.0347 https://www.ncbi.nlm.nih.gov/pubmed/30896346