ALS (Amyotrophic Lateral Sclerosis) is a progressive neurodegenerative disease of the upper & lower motor neurons in the brainstem and motor cortex. In recent years, Mesenchymal stem cells (MSCs) and neural stem cells were differentiated into specialized cells with specific functions needed for patients with ALS. MSC and neural cells act as internal reservoirs in various tissues, crucial in the growth, development, survival, and repair and regeneration of lost function. Clinical trials and previous research in medical journals have shown that the typical life expectancy after diagnosis is three to approximately six years. The actual cause of ALS and Motor Neuron Disease varies from patient to patient; however, it’s widely believed that the underlying issue for a majority of patients can be traced to the dysfunction or misregulation of a vital neuroprotein known as TDP-43.[1]
Motor neuron diseases (MND) are a family of conditions and include primary lateral sclerosis (PLS), amyotrophic lateral sclerosis (ALS), progressive muscular atrophy (PMA), monomelic amyotrophy (MMA), pseudobulbar palsy and progressive bulbar palsy.
Classic symptoms of ALS occur in about 65% of all cases and affect both the upper and lower motor neurons. Classical ALS can be classified as bulbar-onset or spinal-onset (limb-onset) ALS disease. The classification of ALS is unique as the diagnosis of PLS (Primary lateral sclerosis) affects only the upper motor neurons in the arms and legs. In contrast, PMA (progressive muscular atrophy) only affects the lower motor neurons. Other variations of ALS include Respiratory-onset ALS, fail leg syndrome (leg amyotrophic diplegia,) flail arm syndrome (brachial amyotrophic diplegia), and isolated bulbar ALS. Current clinical applications offer a better prognosis for Primary lateral sclerosis than classic ALS due to its slower rate of progress, which results in less functional decline and opens avenues for stem cell-based treatment. Males are more likely to develop young-onset ALS, while juvenile ALS is much more likely to be heredity in nature than adult-onset ALS.
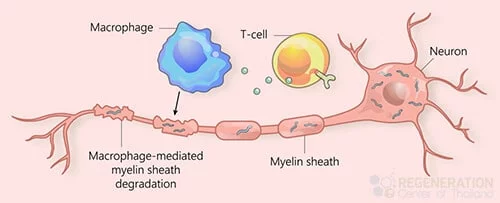
ALS, or Lou Gehrig’s disease, is a very aggressive neurological-degenerative disease that impacts the treatment of ALS and requires innovative approaches like stem cell-based therapy. nerve cells within the brain and the spinal cord. In particular, ALS refers to the degeneration of the motor neurons that reach out from the brain toward the spinal cord and the muscles. ALS will cause the motor neurons to degenerate, which may be mitigated through cell therapy in amyotrophic lateral sclerosis. Cell signaling and neurotransmitters are often the first to die in a process known as cell apoptosis. With it, the capability of the brain to instigate and manage voluntary muscle movements is similar to Parkinson’s Disease and MS. This will eventually result in total paralyzation for the patient during the late stage of the illness.[2]
Due to the rapid degeneration of the upper and lower motor neurons, Neurodegenerative diseases such as ALS usually cause muscle atrophy, neuropathic pain, muscle spasticity, frequent muscle
Along with physical degeneration, patients with ALS also suffer from behavioral or cognitive dysfunctions, which often get misdiagnosed as frontotemporal dementia, complicating the approach to therapies like mesenchymal stem cell transplantation. Some common symptoms include Repeat gestures or phrases, loss of inhibition, apathy, language problems, and verbal memory loss. About 50% of patients with bulbar-onset ALS experience depression and extreme emotional states where they laugh or cry for no apparent reason. Nociceptive pain is another common symptom, as patients report frequent muscle contractions in the cervical spine ( neck area), lower back pain, shoulder pain, or pressure in the stomach area.
Despite rapid progress in understanding the sides, the cause of ALS (also known as Lou Gehrig’s disease) is relatively unknown but is generally attributed as hereditary (familial) or sporadic (environmental). With advancements in molecular diagnostics, the genetic factors associated with ALS are better understood, making the treatment of ALS more effective than relying solely on ecological factors. There is no single specific cause of environmental ALS, but research has proven that the neurodegenerative damage associated with rare movement disorders, ALS, accumulates over long periods.
Scientific studies have shown that familial (hereditary) ALS accounts for less than 10% of all confirmed cases. Inherited ALS is either an X-linked dominant pattern or an autosomal recessive pattern. Each parent carries one copy of the mutated gene but often shows no signs or symptoms. For this reason, autosomal recessive ALS is frequently misdiagnosed as environmental (sporadic) ALS. The most common markers for heredity ALS are C9orf72, SOD1, FUS, and TARDBP. Still, there are over 20 genes that are linked to familial ALS, and the only way to accurately identify genetic mutations is with DNA screenings.
Since DNA testing was not prevalent in previous generations, it’s often difficult to predict unless proactively screened for. Clinical diagnosis for ALS typically requires mutations in at least 2 (or more) genes due to oligogenic inheritance. The regeneration center does not offer Gene therapies for ALS are being explored in various clinical studies. Still, it can provide insights into the efficacy of stem cell-based therapy for patients with amyotrophic lateral sclerosis. DNA sequencing tests are crucial for determining the best cell-based therapy options for patients with amyotrophic lateral sclerosis. For the 20 most common genetic causes of familial Amyotrophic Lateral Sclerosis, including ALS2, TBK1, SOD1, DCTN1, SPG11, TARDBP, KIF5A, FUS, OPTN, PFN1, SETX, CHCHD10, CHMP2B, MATR3, UBQLN2, VAPB, TFG, VCP, SIGMAR1, and SQSTM1.
Patients with sporadic ALS account for over 90% of all cases. It’s important to note that the symptoms of familial and sporadic ALS are nearly identical and can only be differentiated genetically. For patients with no known family history and mutated genes, environmental factors are typically the cause of the progression of ALS. ALS researchers have identified various factors, such as exposure to heavy metals and environmental toxins like lead, chemical exposure, pesticides, serum uric acid, DDT, organochlorine, dieldrin, and toxaphene, which are known foggy brain causes for damage to motor neurons, motor neuron death and acute injuries to the central nervous system. Learn more about ALS-friendly diets.
Evidence is often inconclusive, but some potential environmental factors might include the following:
ALS progression rates vary from person to person, but common symptoms include:
The Regeneration Center treatment for ALS is a safe and effective functional medical treatment for complex neurodegenerative conditions such as MND & ALS, along with other therapies, are being developed in clinical trials and can be placed through the ALS Association. treatments for Brain Injuries, strokes, and Alzheimer’s all essentially focus on trying to slow disease progression, stopping the spread and potential reduction of symptoms related to the illness. Neuro-stem cells and their possible role in the treatment of ALS are being researched extensively. Along with supportive glial cells, neural cell growth factors and exosomes can be used to slow down and reverse the consequences of ALS and restore the quality of life for the patient.[3]
The Regeneration Center does not offer gene therapies, embryonic stem cells, induced pluripotent stem cells, or stem cells derived from animals, i.e., “Live Cells,” due to safety and efficacy concerns. Our enhanced neural stem cells and nerve growth factors are isolated and expanded into the required quantities and lineages, including glial restricted progenitor cells (GRP), oligodendrocyte progenitor cells (OPCs), astrocytes, and neurons.
After collection, the stem cells are concentrated and then isolated to measure the overall quantity and quality of the collected stem cells. Only certain types of activated neural progenitor stem cells can transform into the necessary types of cells. These activated stem cells and neurotrophic factors can regenerate damaged tissues, such as the myelin sheath needed in clinical therapies for ALS and bone marrow treatments. spinal muscular atrophy.[4]
Number of Stages in Clinical Program: Multi-stage process using multi-combination infusions of glial restricted progenitor cells (GRP), oligodendrocyte neural progenitor cells (OPCs), Astrocytes exosomes are being investigated for their potential role in cell types relevant to ALS therapy., and neurons per treatment phase. The types of nerve cells and growth factors can include enhanced neural stem cells from differentiated cell lineage via IV Drip, Intrathecal, and lumbar puncture, per the patient’s needs. Learn about clinical trials for ALS and the efficacy of cell-based therapies being tested..
Stem Cell Delivery Methods used: The Regeneration Center protocol combines multipotent stem cells from umbilical cord tissue (UC-MSC) and neural stem cells along with mesenchymal stromal cells, neurotrophic factors, and neural nerve cells that are delivered to the patient through IV Drips, Intramuscular injections, Intrathecal Injections (to bypass blood-brain barrier). In some cases, fluoroscopy-guided or Intraparenchymal injections may be required in a hospital setting for patients requiring direct injections into the spinal vertebra under local anesthesia. The patients are advised to stay within the recovery space for a few hours following the direct injection.
Physical Rehabilitation: Physical Rehab after completion of therapy is advised. Physical rehabilitation post-therapy can be provided upon request for 2-4 hours per day and up to 5 days per week. Medical visas and extended accommodations at a hotel or furnished apartments for the patient and family can also be included upon request, especially for those seeking advanced therapies like stem cell transplantation in amyotrophic lateral sclerosis.
Treating Amyotrophic Lateral Sclerosis (ALS) with motor neurons derived from stem cells is an area of active research, offering hope for a condition that currently has no cure. ALS is a neurodegenerative disorder characterized by the progressive loss of motor neurons, the nerve cells responsible for controlling voluntary muscles. This loss leads to muscle weakness, paralysis, and eventually respiratory failure.
Motor neurons derived from stem cells, mainly induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs), are being explored as a potential treatment for ALS. The goal of these therapies is to replace the lost or damaged motor neurons in patients with ALS, potentially slowing or halting disease progression.
Several essential factors come into play when considering the safety and efficacy of using motor neurons derived from stem cells to treat ALS. Safety concerns primarily revolve around the risk of immune rejection, where the body might attack the transplanted cells if they are not HLA-matched to the patient’s cells. There is also a risk of tumor formation, especially with pluripotent stem cells like iPSCs and ESCs, since these cells can increase rapidly. Efficacy concerns focus on whether the transplanted motor neurons can survive, integrate into the patient’s central nervous system, and function properly, especially in stem cell therapy in amyotrophic lateral sclerosis. This includes making sure they connect correctly with muscles and other neurons, which is crucial for them to help restore lost functions. Stem cell research is ongoing to determine whether these treatments can safely and effectively slow or halt the progression of ALS, with early results showing promise but also highlighting the need for more research to overcome these challenges.
Please note we do not offer gene therapies for ALS. For approved patients, the treatment will require a minimum of 2 weeks for the cell transplantation. Due to the significant differences and stages of damage, our medical team will need to review the potential candidate’s medical records and eligibility for treatment and travel to Thailand. Upon completion of the medical review, a complete clinical plan will be provided that will include the specifics of the therapy, including the total number of nights required and the total medical-related costs and stem cell transplant fees (excluding accommodations or flights). To begin the qualification process for the multi-stage ALS stem cell transplantation, please prepare your recent medical records, such as a list of current medications (radical/radical, edaravone, riluzole), all functional rating scale, Brain MRIs, CT Scans, or PET Scans (Preferred) and contact us today.
[1] ^ Kwon, Min-Soo, Min-Young Noh, Ki-Wook Oh, Kyung-Ah Cho, Byung-Yong Kang, Kyung-Suk Kim, Young-Seo Kim, and Seung H Kim are contributing to ALS research. 2014. The immunomodulatory effects of human mesenchymal stem cells on peripheral blood mononuclear cells in ALS patients. Journal of Neurochemistry, no. 2 (July 31) is a crucial date for the phase 2 clinical studies on ALS therapies. doi:10.1111/jnc.12814. https://www.ncbi.nlm.nih.gov/pubmed/24995608
[2] ^ Mazzini, Letizia, Angelo Vescovi, Roberto Cantello, Maurizio Gelati, and Alessandro Vercelli. 2016. Stem cell therapy for ALS. Expert opinion on biological therapy, specifically regarding stem cell treatment in amyotrophic lateral sclerosis, is no. 2 (January 9). doi:10.1517/14712598.2016.1116516. https://www.ncbi.nlm.nih.gov/pubmed/26558293
[3] ^ Poungvarin, N, and A Viriyavejakul. 1991 marked significant advancements in the understanding of stem cell-based therapy for neurological diseases, leading to the exploration of cell transplantation in amyotrophic lateral sclerosis. Motor neuron disease in Thailand: the clinical aspects of 77 patients. Journal of the Medical Association of Thailand = Chotmaihet thangphaet, no. 4. https://www.ncbi.nlm.nih.gov/pubmed/1940701
[4] ^ Thomsen, Gretchen M, Genevieve Gowing, Soshana Svendsen, and Clive N Svendsen. 2014. The past, present, and future of stem cell clinical trials for ALS. Experimental neurology (March 6). doi:10.1016/j.expneurol.2014.02.021. https://www.ncbi.nlm.nih.gov/pubmed/24613827