A stroke is an interruption of blood flow and oxygen to parts of the brain. Cell death begins once the gray matter in brain cells stops getting enough oxygen and nutrients to survive. Gray matter contains most neuronal cell bodies in the human mind. It manages many functions, such as emotions, muscle control, hearing, decision-making, sensory perceptions, memory, speech, and self-control.
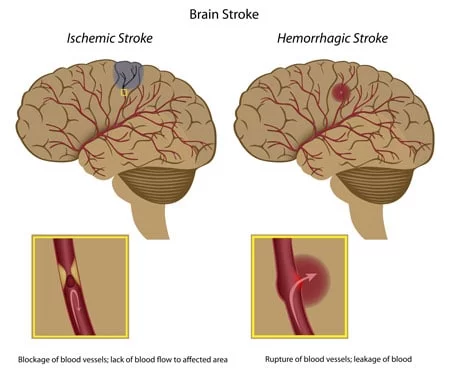
There are two main types and causes of brain strokes in the central nervous system. Sudden blocking of arteries can cause acute ischemic strokes or damage to blood vessels, resulting in bursting or leaks that can cause hemorrhagic strokes and cryptogenic strokes. Over 80-85% of strokes are ischemic, and about 10-15% of strokes are hemorrhagic. Strokes caused by bleeding cause more damage and are more challenging to treat than ischemic. Some patients may have a very short disruption to the brain known as a transient ischemic attack (TIA) or “mini-strokes,” but these types of strokes are not as dangerous and might not cause permanent brain damage.
A stroke caused by blockage of the blood vessels that supply blood to our brain is known as an ischemic stroke and is generally the most common type of stroke we treat at the Regeneration Centre. There are two main classifications for ischemic strokes.
Acute Ischemic strokes are caused by blood clots or stenosis (narrowing of the blood arteries.) Stenosis is often caused by poor habits that lead to atherosclerosis, causing thick artery walls, hardening, and a loss of elasticity, decreasing blood flow. Other factors include a family history of strokes/genetics, dementia, atrial fibrillation, heart disease, Congestive heart failure, diabetes, high cholesterol, and Smoking.[1]. DNA tests are now available for genetic predisposition to strokes.
A rupture in the blood vessels usually causes a hemorrhagic stroke. Several causes exist, including aneurysms, weak spots on the arterial walls, and Hypertension or High blood pressure. There are two main types of hemorrhagic strokes.
The severity of the physical damage caused by a stroke depends on how much blood flow was restricted and for how long. Some visible and noticeable consequences of impaired brain function are:
For most people, the symptoms of a stroke typically start without prior warning and can last from just a few seconds to a few minutes. Fortunately, patients recover quickly without further damage or issues, but this is not the case for many. The symptoms and warning signs often depend on which brain area gets affected. Severe strokes affect more significant regions in the brain; thus, more physical functions are likely lost and can result in orthopedic injuries to knees, hips, hands, or shoulders due to falls.
Currently, the only traditional treatments of ischemic strokes require restoration of proper blood flow back into the affected area by using a mechanical device or thrombolytics that physically removes any brain clots. The use of thrombolytics is very beneficial if introduced a few hours after the patient displays chronic stroke symptoms but not very useful the longer a patient waits. This means that only a few stroke patients can take advantage of this therapy due to the timing requirements.
Several factors can increase or reduce a person’s risk of getting strokes. Some controllable risk factors for strokes include:
Other medical-related risk factors include:
Brain stroke kills twice as many women per year as breast cancer. Strokes are currently the third leading cause of death for women across the world. For this reason, women should take the necessary steps by understanding the factors and making changes to reduce overall risk factors.
Some female-specific risk factors for having brain strokes include:
At the hospital, nerve function tests can help provide clues as to which parts of the brain are affected by the stroke and how severe the damage is. Blood collection and testing provide information on, among other things, blood counts, blood clotting, inflammatory parameters, and risk factors such as elevated cholesterol or blood glucose levels. The medical team can then use imaging techniques such as CT Scan (computed tomography) or MRI scan (magnetic resonance tomography) to scrutinize the patient’s brain. The radiology scans are beneficial in diagnosing if the patient has an ischemic or hemorrhagic stroke present and detect circulatory disorders or existing cerebral hemorrhages. In addition, the cerebral vessels can also be visualized by a CT angiography to detect blockages.
Other tests used to check the cause of the stroke and brain vessels affected by arteriosclerosis, narrowing, or thrombosis include ultrasound or duplex sonogram. Carotid arteries are also checked for permeability and can be visualized using a contrast medium on a CT or MRI scan. An electrocardiogram (ECG) is used to detect cardiac arrhythmias.
Stroke treatment depends on what type of stroke it is and what the underlying cause is. For ischemic & cryptogenic strokes, doctors need to act quickly to restore blood flow to the brain and avoid further brain damage.
Some medications for ischemic strokes can be used to try to break the clots inside the veins and must be given a few hours after a stroke.
The goal of hemorrhagic stroke treatment is to control/stop the bleeding and reduce any extra pressure on the brain. Medications for Hemorrhagic strokes include warfarin (Jantoven, Coumadin) and anti-platelet medications such as Plavix (clopidogrel) to help prevent blood clots. Note that anti-clotting medications and some blood thinners can conflict with stem cell therapy. Other medicines for Hemorrhagic strokes are used to lower intracranial pressure, lower blood pressure, prevent seizures, or prevent vasospasm.
Traditional treatments for stroke patients can only manage the symptoms but cannot do much to try to repair the damaged tissue or replace the dead cells. Exosome therapy using astrocytes and neural stem cell growth factors helps target the underlying cause of the patient’s injury and not just mask the symptoms. Neural stem cell transplants are safe and painless to inject and have been shown to survive transplantation and begin differentiating into neuronal cells and new functional neurons in the brain tissue. In addition to replacing damaged cells, replacement therapy to bypass the blood-brain barrier can induce endogenous neural precursors that help boost the brain’s structural neuroplasticity and regulate pro-inflammatory cytokines and the neuronal apoptotic death process. To learn about stem cells and brain-friendly diets.
Damage to the brain usually occurs when the proper flow of oxygen and blood is stopped or blocked for some time. Getting immediate medical intervention is critical to restore the brain tissue’s average blood and oxygen circulation and avoid long-term damage. We typically recommend having active treatments like human neural stem cell replacement as quickly as possible following a stroke to prevent the chances of lesions forming, which lead to scar tissue that cannot be repaired after a certain length of time, causing permanent paralysis with peripheral neuropathic pain in ischemic stroke patients.
Neural stem cell therapy uses the paracrine cell signaling method to target the damaged part of the brain’s neural circuitry that controls motor functions. The cells are first enhanced in our stem cell lab and then injected intravenously via a proprietary stem cell nebulizer treatment to deliver cells near the motor neuron tracts close to the lesions to promote regeneration and repair through the section of Cytokines and nerve growth factors. The benefits are gradual; however, most patients show immediate improvements after the first or second infusions and continue to show improvement 3-6 months post-therapy. The results are permanent but will require consistent physical and speech rehabilitation after treatment to allow the brain to return to proper function, especially for cases with cerebral hemorrhaging and cerebral infarction.[3]
Other noticeable improvements after mesenchymal stem cell therapy for strokes include:
Mesenchymal stromal cells and isolated glial cells offer a breakthrough technology but have limitations. Based on research and experiences, the most successful patient recoveries happen for patients who start intervention treatment with pluripotent stem cells very early after the incident. Lack of oxygen to the brain tissue can cause rapid damage and failure to other vital organs.[4] Suppose you or a loved one are unable to get stem cell therapy quickly after a stroke. In that case, we recommend daily use of hyperbaric oxygen chambers, External counterpulsation therapy (ECP), pulsed electromagnetic therapy (PEMFT) to areas on the back of the patient’s head, neural growth factors, nutritional IV injections, and periodic acceleration therapy.
Brain stroke can lead to severe brain tissue damage, resulting in permanent paralysis for some patients. Neural stem cell therapy for strokes has limitations but offers a viable potential cure for paralysis caused by brain infarction. There is clinical trial evidence that has shown neurogenic endogenous stem cells & multipotent adult progenitor cells transplanted into the brain can initiate repair and repair-related events reaching peak levels, suggesting that exogenous cell therapies can indeed regenerate damaged brain tissue and help to promote functional recovery for some stroke patients.
Pluripotent stem cell therapies offer a promising way to regenerate neurons damaged by a brain stroke. Stem cell research has shown that isolated and expanded UC-MSC+ cells rapidly promote functional recovery in stroke patients by reducing the severity of brain damage after infarction. These cultured stem cells release growth factors that promote the development of new blood vessels (angiogenesis), reduce systemic inflammation, and help regenerate damaged brain tissue.
Physical and Speech Rehabilitation is highly recommended after a stroke treatment and can be provided at a local hotel facility upon request. We can also assist you in finding certified physical or speech rehabilitation with an accredited therapist in your home country, depending on where you live. Medical visas and accommodations for an extended stay at serviced apartments are provided upon request.
Due to varying severity, our medical team must review the patient’s medical records and diagnostic imaging results. Once the medical review is complete, we can determine whether the patient is a good candidate and provide a fixed cost for the treatment. To help us make an accurate assessment and provide a detailed treatment plan, our medical staff will need to review the recent medical records, including any imaging results from Brain radiology scans. (Test Results less than three months old are required for treatment evaluation)
To begin the medical evaluation for our multi-stage stroke treatment, please contact us today.
[1] ^ Bandasak, Ratanaporn, Kulaya Narksawat, Chanpong Tangkanakul, Yotin Chinvarun, and Sukhontha Siri. 2011. Association between hypertension and stroke among young Thai adults in Bangkok, Thailand. The Southeast Asian journal of tropical medicine and public health, no. 5. https://www.ncbi.nlm.nih.gov/pubmed/22299451
[2] ^ Nilanont, Yongchai, Samart Nidhinandana, Nijasri C Suwanwela, Suchat Hanchaiphiboolkul, Taksin Pimpak, Pyatat Tatsanavivat, Gustavo Saposnik, and Niphon Poungvarin. 2013. Quality of acute ischemic stroke care in Thailand: a prospective multicenter countrywide cohort study. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association, no. 2 (January 8). doi:10.1016/j.jstrokecerebrovasdis.2012.12.001. https://www.ncbi.nlm.nih.gov/pubmed/23305673
[3] ^ Dharmasaroja, Permphan. 2008. Bone marrow-derived mesenchymal stromal stem cells for the treatment of ischemic stroke. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, no. 1 (November 18). doi:10.1016/j.jocn.2008.05.006. https://www.ncbi.nlm.nih.gov/pubmed/19017556
[4] ^ Hao, Lei, Zhongmin Zou, Hong Tian, Yubo Zhang, Huchuan Zhou, and Lei Liu. 2014. Stem cell-based therapies for ischemic stroke. BioMed research international (February 26). doi:10.1155/2014/468748. https://www.ncbi.nlm.nih.gov/pubmed/24719869