Macrophage are specific type of WBC or white blood cells, which are known to have a versatile functionality inside and for the immune system.
Dendritic Cells and Macrophages (VIDEO)
Macrophages are known as the body’s first line of defense against invasion from viruses and bacteria, Macrophages are generally responsible for safeguarding our inter-cellular environment by killing several types of bacterias.
During the time of infection or tissue damage,monocyte cells leave the bloodstream and rush to the affected organs such as liver and kidney or other tissues to differentiate into becoming become macrophages. These macrophage cells can modify themselves into forming different types of cell structures to fight different microbes and viruses.[1]
Macrophages are versatile immune cells that can assume a variety of functional states depending on the signals they receive from their environment. The two most commonly described macrophage activation states are the classically activated (often referred to as M1) and the alternatively activated (often referred to as M2) macrophages. However, in reality, macrophage activation exists on a spectrum, and the M1/M2 dichotomy is a simplification.
M1 Macrophages (Classically Activated):
These are typically activated by pro-inflammatory stimuli such as lipopolysaccharide (LPS) and interferon-gamma (IFN-γ). They play a role in microbial killing and promoting inflammation.
M1 Function Markers:
- Cytokines: TNF-α, IL-1β, IL-6, IL-12, IL-23
- Fractalkine
- Chemokines: CCL2, CXCL10
- Enzymes: iNOS (inducible nitric oxide synthase), which produces nitric oxide
- Surface Markers: CD80, CD86
M2 Macrophages (Alternatively Activated): are typically stimulated by anti-inflammatory signals such as IL-4 and IL-13. M2 macrophages are associated with tissue repair, wound healing, and immune regulation.
M2 Function Markers:
- Cytokines: IL-10
- Enzymes: Arginase-1 (Arg-1), which is involved in collagen formation and wound healing
- Surface Markers: CD163, CD206 (mannose receptor)
- Other Markers: Ym1 (chitinase-like protein), Fizz1 (resistin-like molecule alpha)
Fluid Activation States: The M1/M2 dichotomy is a general model. In reality, macrophages can exhibit a spectrum of phenotypes based on the myriad signals they receive. The mentioned markers are common but might not capture all the nuances of macrophage activation.
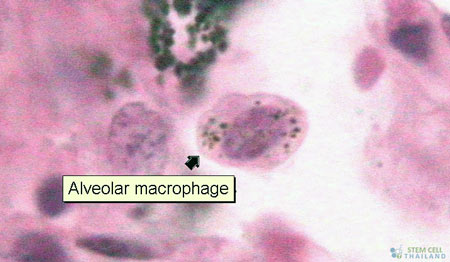
Tissue-Resident Macrophages: Apart from circulating monocyte-derived macrophages, various tissues have resident macrophages (like Kupffer cells in the liver, microglia in the brain, and alveolar macrophages in the lungs). These resident macrophages might have unique markers and functions depending on their tissue of residence.
Understanding the diverse functional states of macrophages and their associated markers is essential for both basic immunology research and the development of therapeutic strategies to modulate immune responses in various diseases.
Humans macrophages are only about 22 micrometres in diameter.[2] They can survive for several. Macrophage cells are also involved in the development of innate immunities. Different macrophages have different protein markers on their exterior surfaces.
Examples of known macrophage markers include:
- EMR1
- MAC-1
- MAC-3
- CD11b
- CD14
- CD68
- Lysozyme
Cellular Immunotherapy
Our stem cell doctors are able to identify such specific markers using a device known as a flow-cytometer.[3]
Published Clinical Citations
[1] ^ Chatterjee, Priyajit, Soma Seal, Sandip Mukherjee, Rakesh Kundu, Sutapa Mukherjee, Sukanta Ray, Satinath Mukhopadhyay, Subeer S Majumdar, and Samir Bhattacharya. 2013. Adipocyte fetuin-A contributes to macrophage migration into adipose tissue and polarization of macrophages. The Journal of biological chemistry, no. 39 (August 13). doi:10.1074/jbc.C113.495473. https://www.ncbi.nlm.nih.gov/pubmed/23943623.
[2] ^ Roger, Thierry, Julie Delaloye, Anne-Laure Chanson, Marlyse Giddey, Didier Le Roy, and Thierry Calandra. 2012. Macrophage migration inhibitory factor deficiency is associated with impaired killing of gram-negative bacteria by macrophages and increased susceptibility to Klebsiella pneumoniae sepsis. The Journal of infectious diseases, no. 2 (November 2). doi:10.1093/infdis/jis673. https://www.ncbi.nlm.nih.gov/pubmed/23125447.
[3] ^ Sun, Yu, Yu Wang, Jia-Hui Li, Shi-Hui Zhu, Hong-Tai Tang, and Zhao-Fan Xia. 2013. Macrophage migration inhibitory factor counter-regulates dexamethasone-induced annexin 1 expression and influences the release of eicosanoids in murine macrophages. Immunology, no. 2. doi:10.1111/imm.12135. https://www.ncbi.nlm.nih.gov/pubmed/23777345.